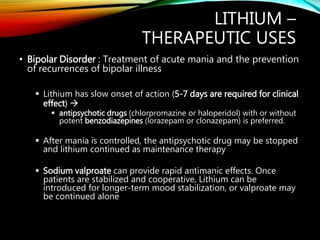
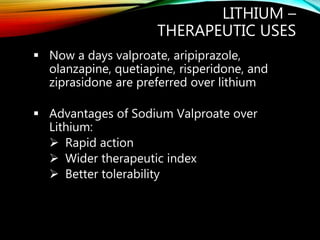
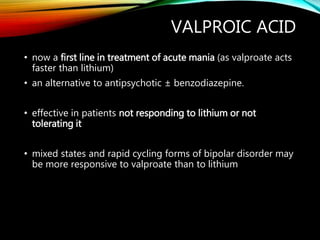
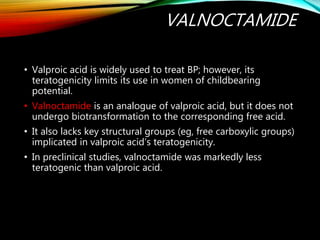
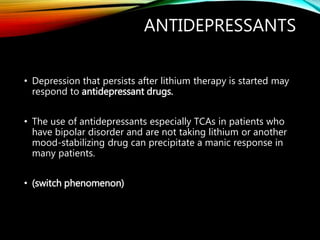
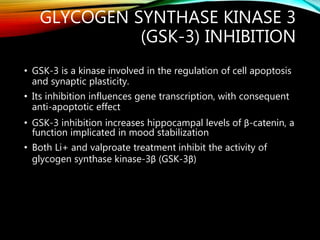
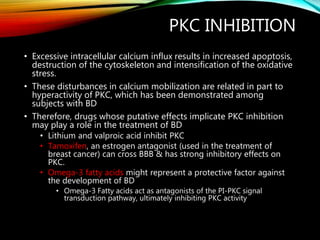
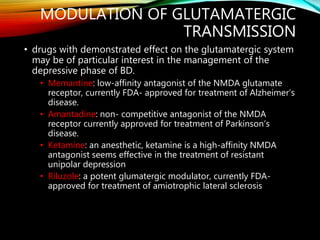
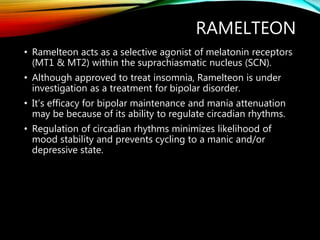
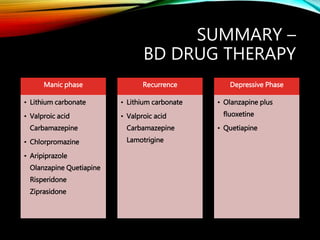
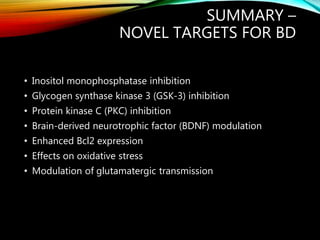
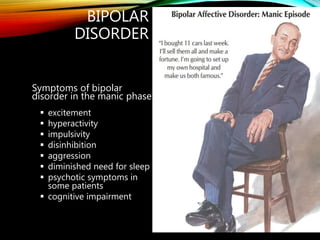
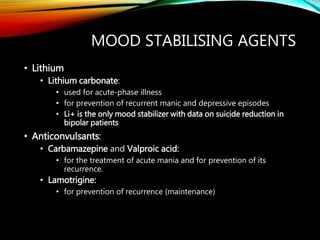
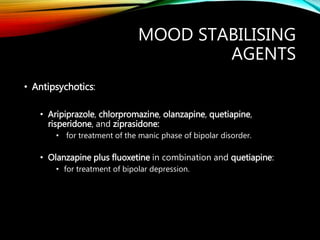
This document discusses mood stabilizers used to treat bipolar disorder. It describes the symptoms of mania and depression in bipolar disorder. Lithium, valproic acid, carbamazepine, lamotrigine and various antipsychotics are described as first-line mood stabilizing agents. The mechanisms of action of these drugs involve inhibition of inositol monophosphatase and other enzymes, decreasing intracellular inositol levels. Novel targets for treating bipolar disorder discussed include inhibition of glycogen synthase kinase-3, protein kinase C, modulation of brain-derived neurotrophic factor, enhanced Bcl2 expression, effects on oxidative stress, and modulation of glutamatergic transmission.

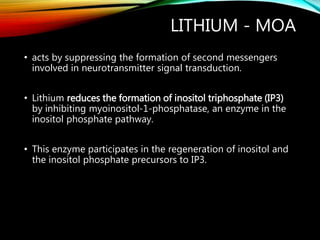

![Li inhibits inositol monophosphatase (IMPase)
↓ free inositol
↓phosphatidylinositol-4,5-bisphosphate (PIP2)
[the membrane precursor of IP3 & DAG]
depletion of the second-messenger source PIP2
causes reduced release of IP3 and DAG
decreased activity of PIP2 dependent pathways
(which are markedly increased during manic episode)
Mood Stabilising action
MECHANISM OF ACTION](https://image.slidesharecdn.com/ms-160204093125/85/Mood-Stabilisers-Antimanic-drugs-12-320.jpg)