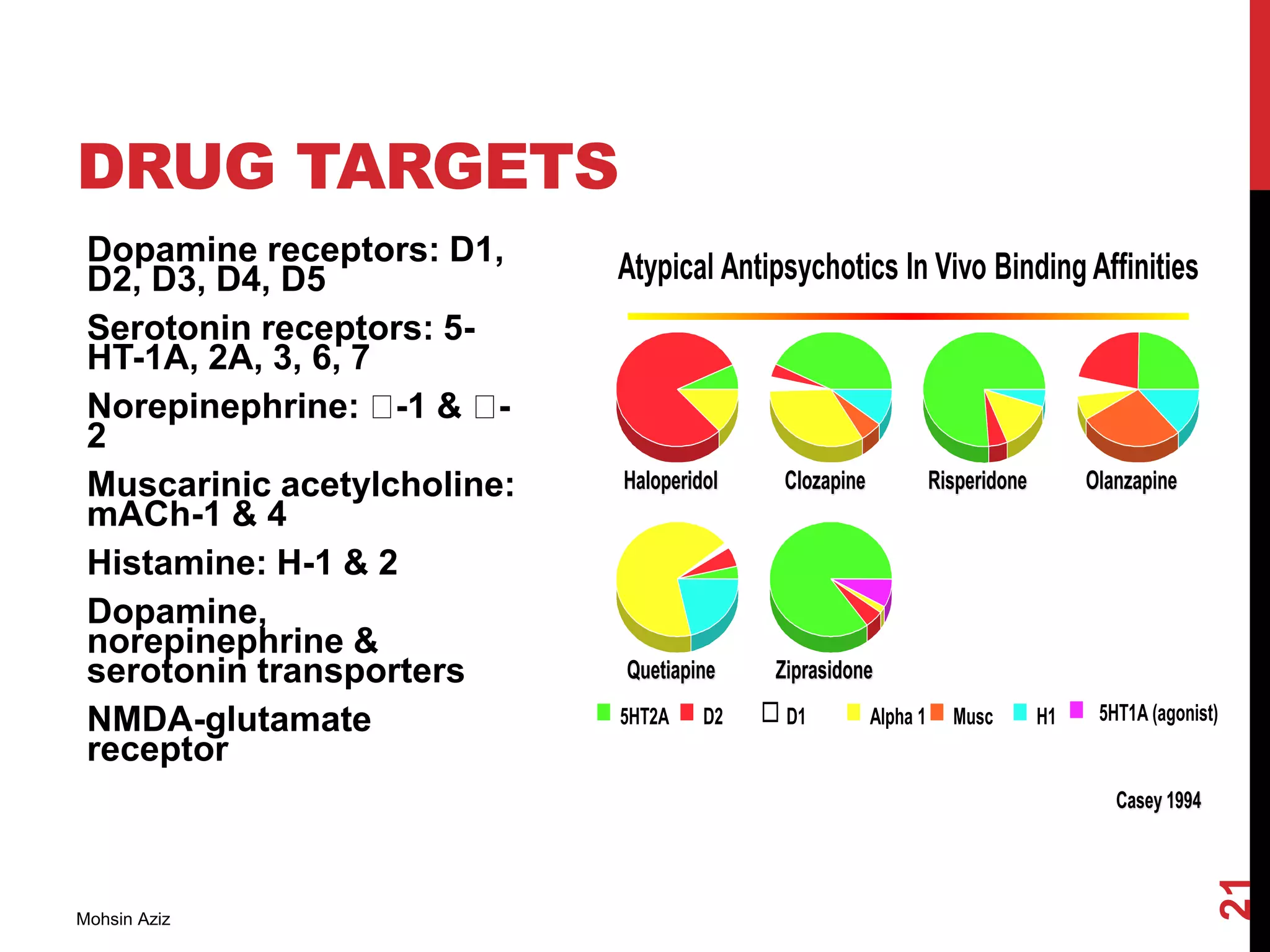
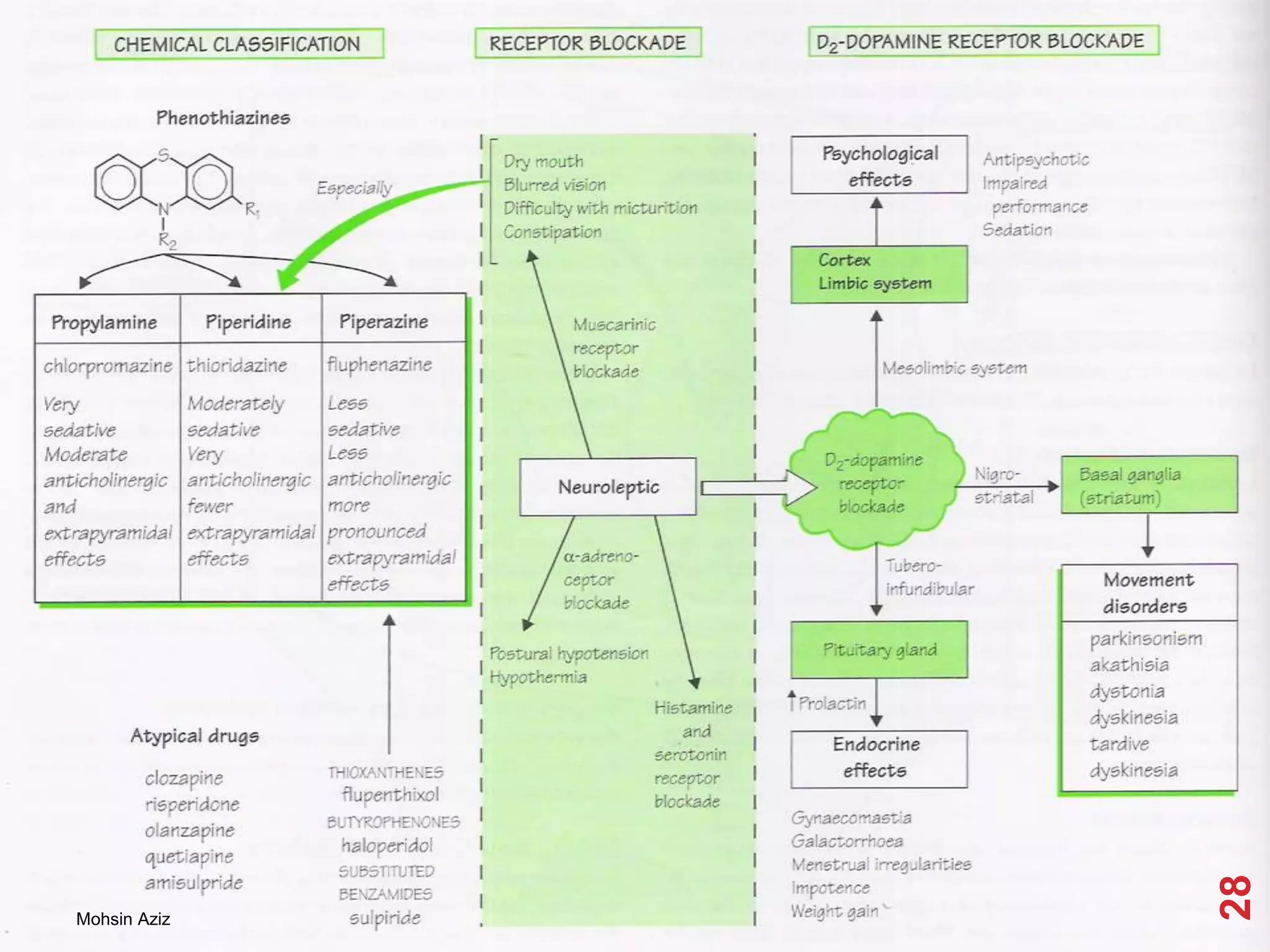
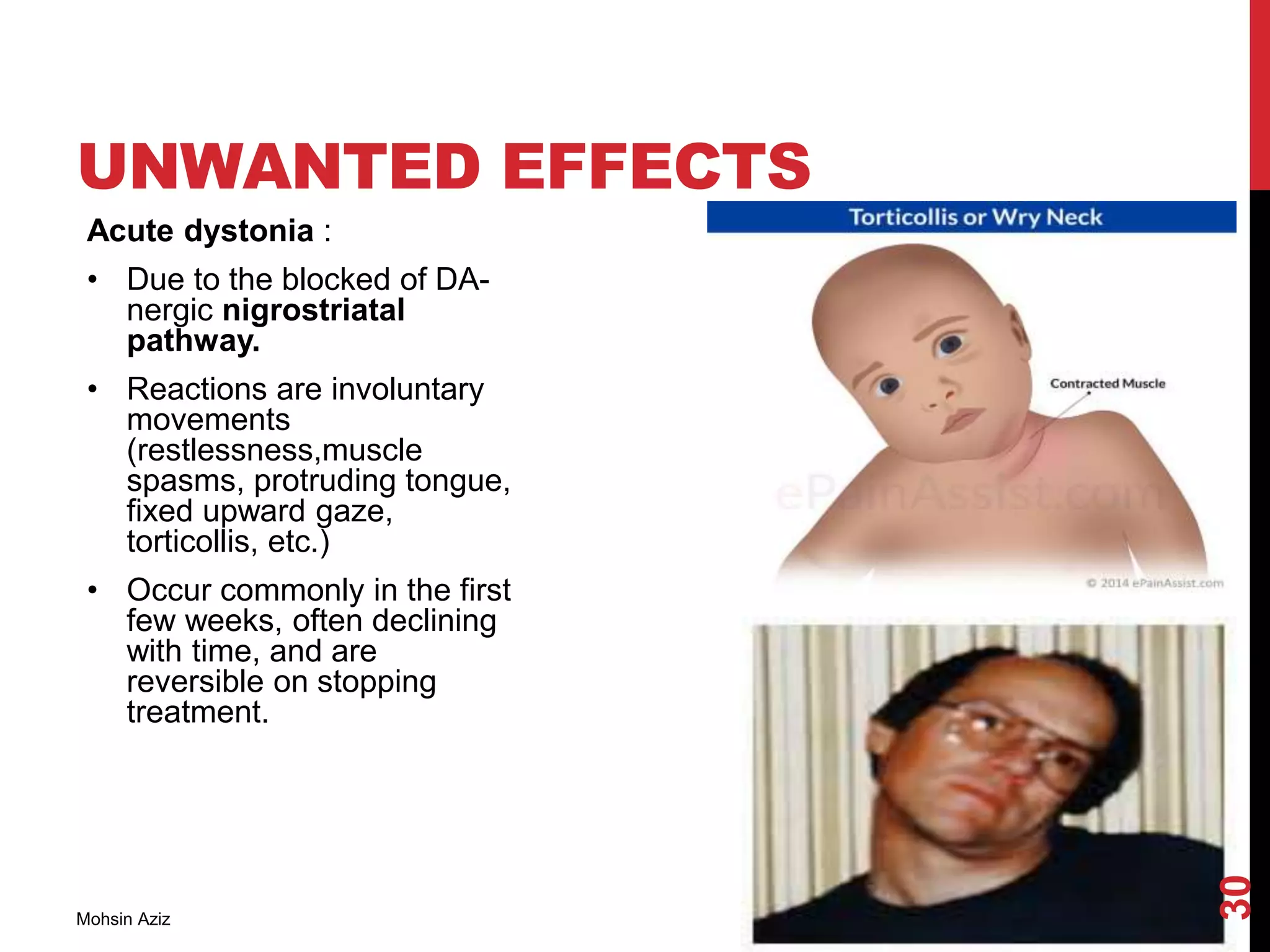
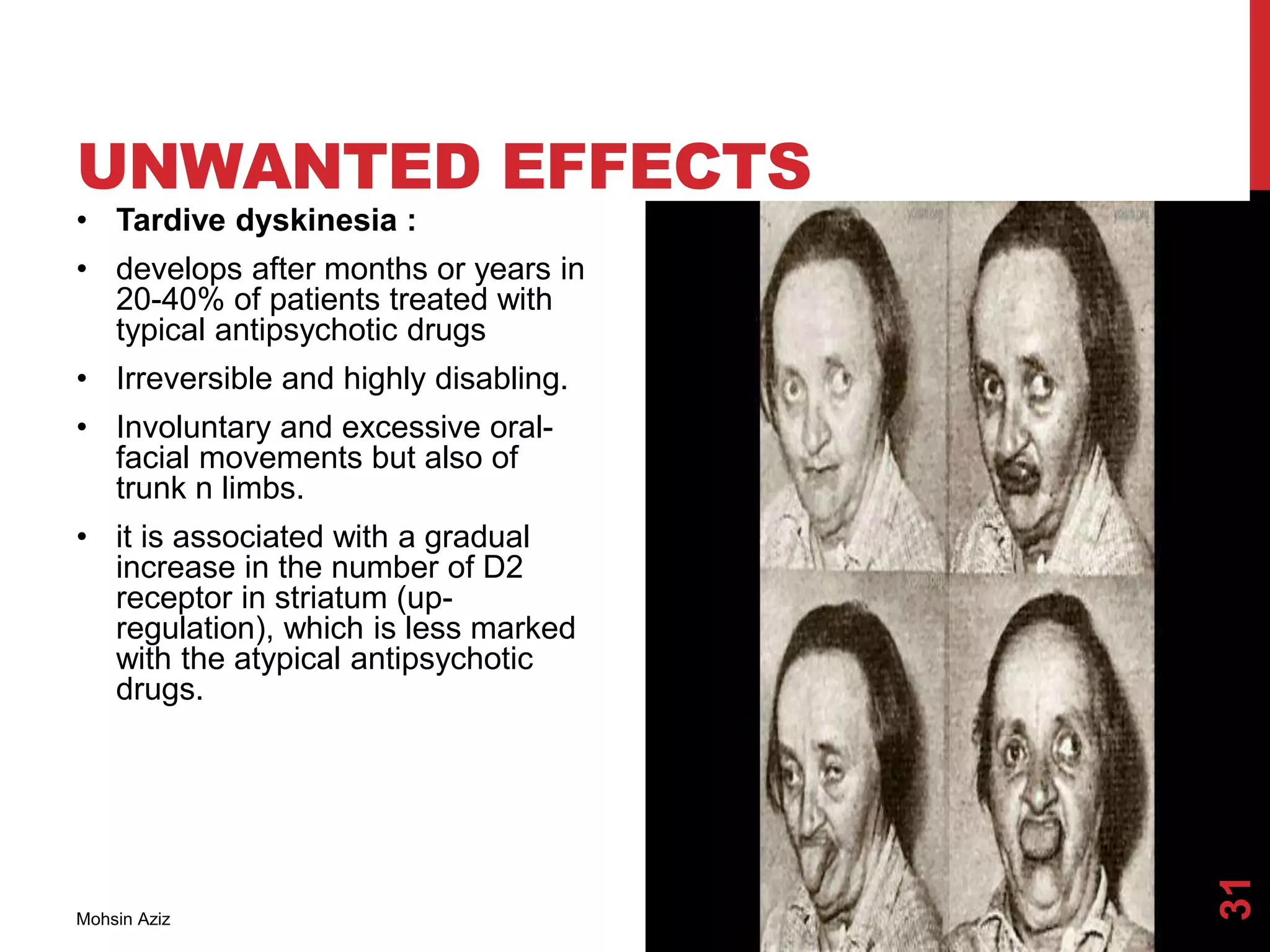
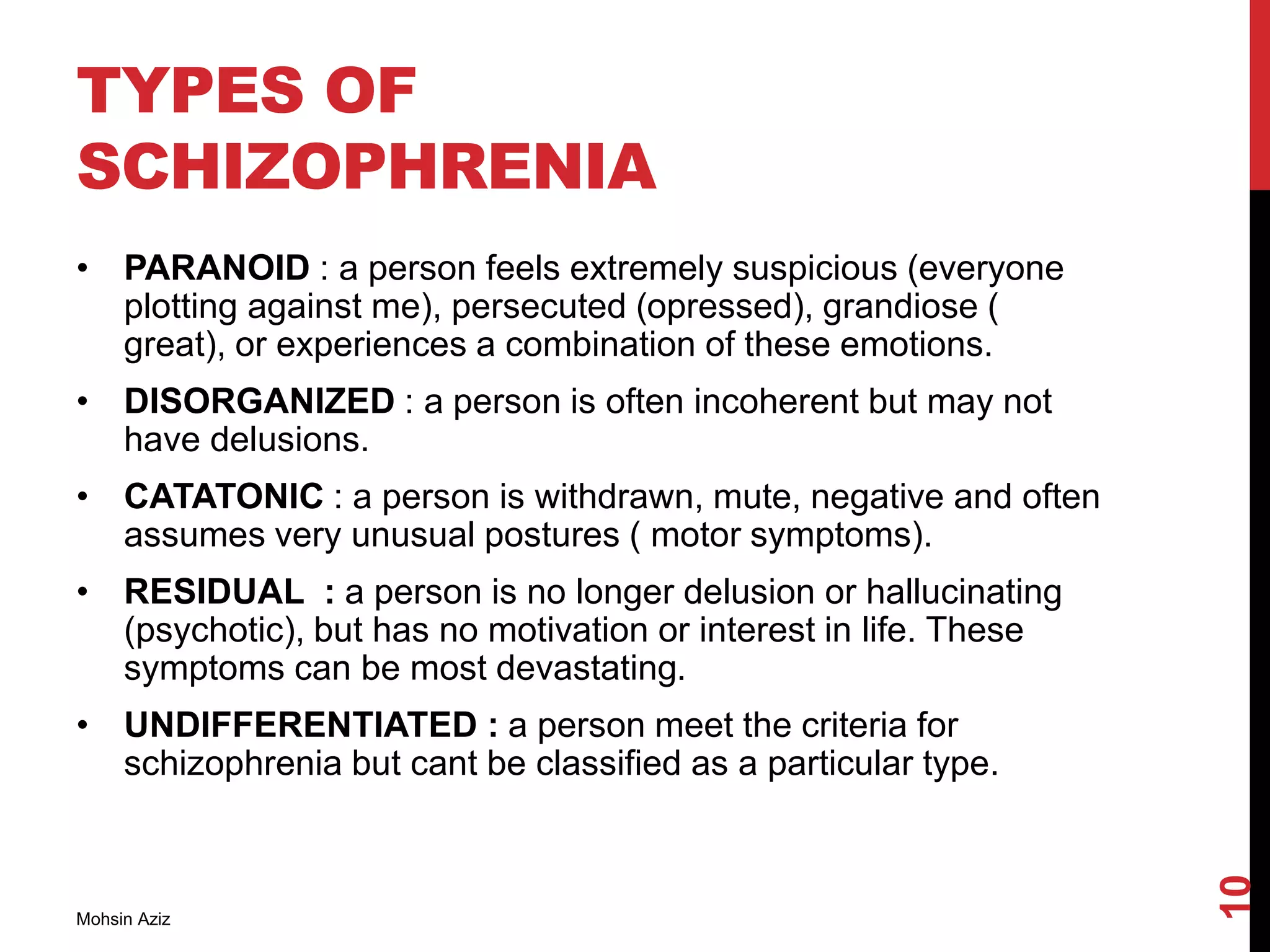
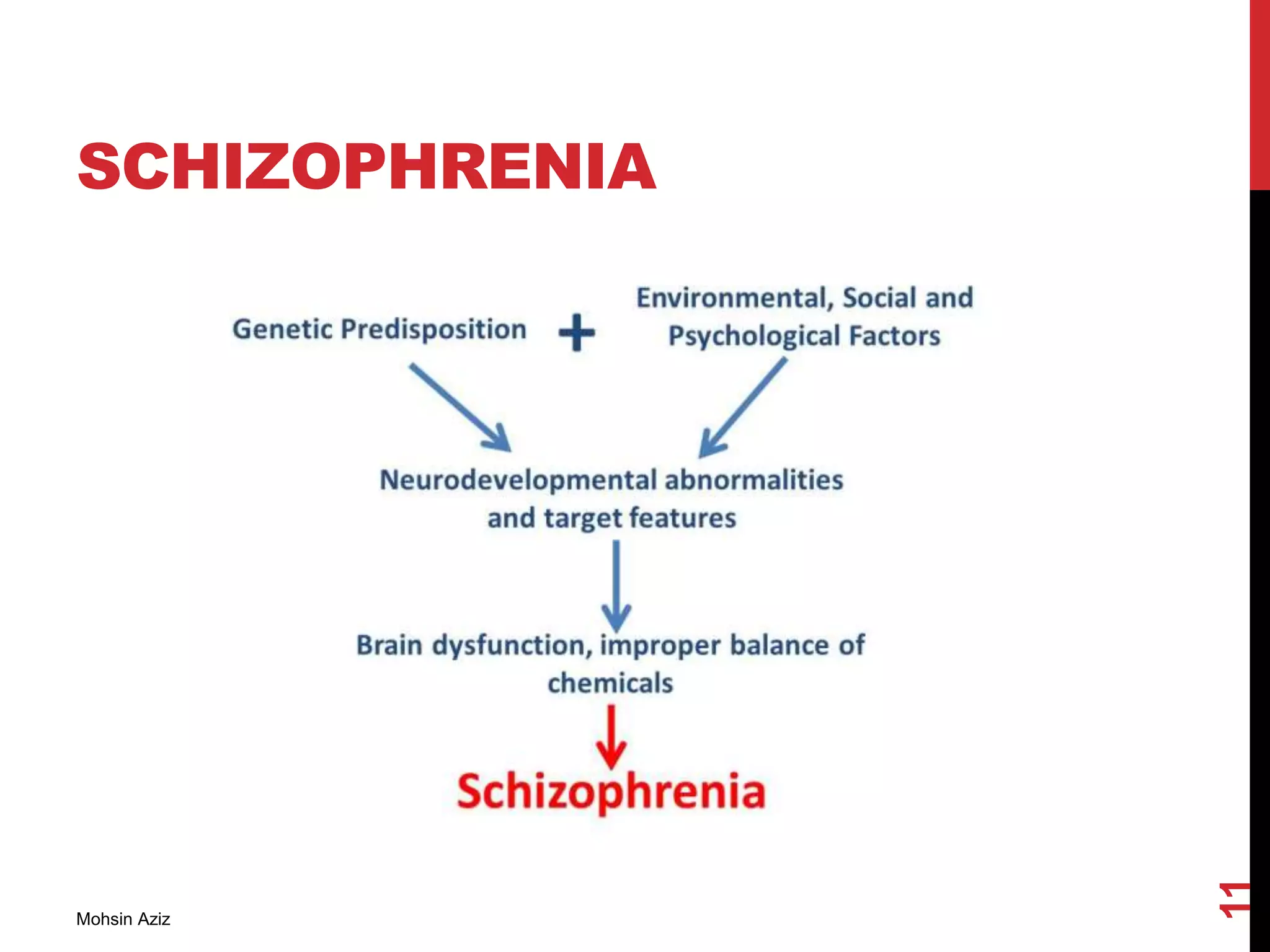
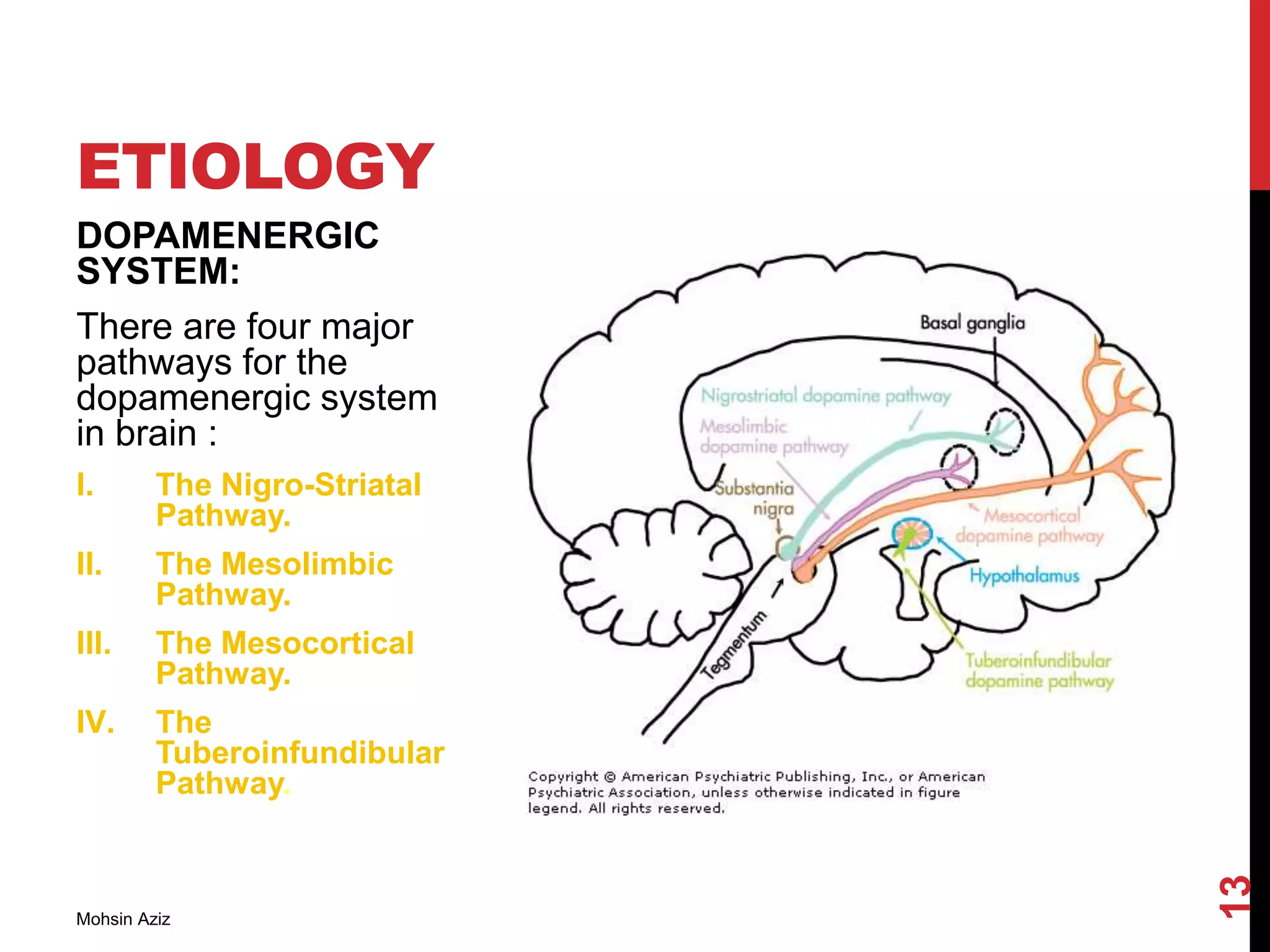
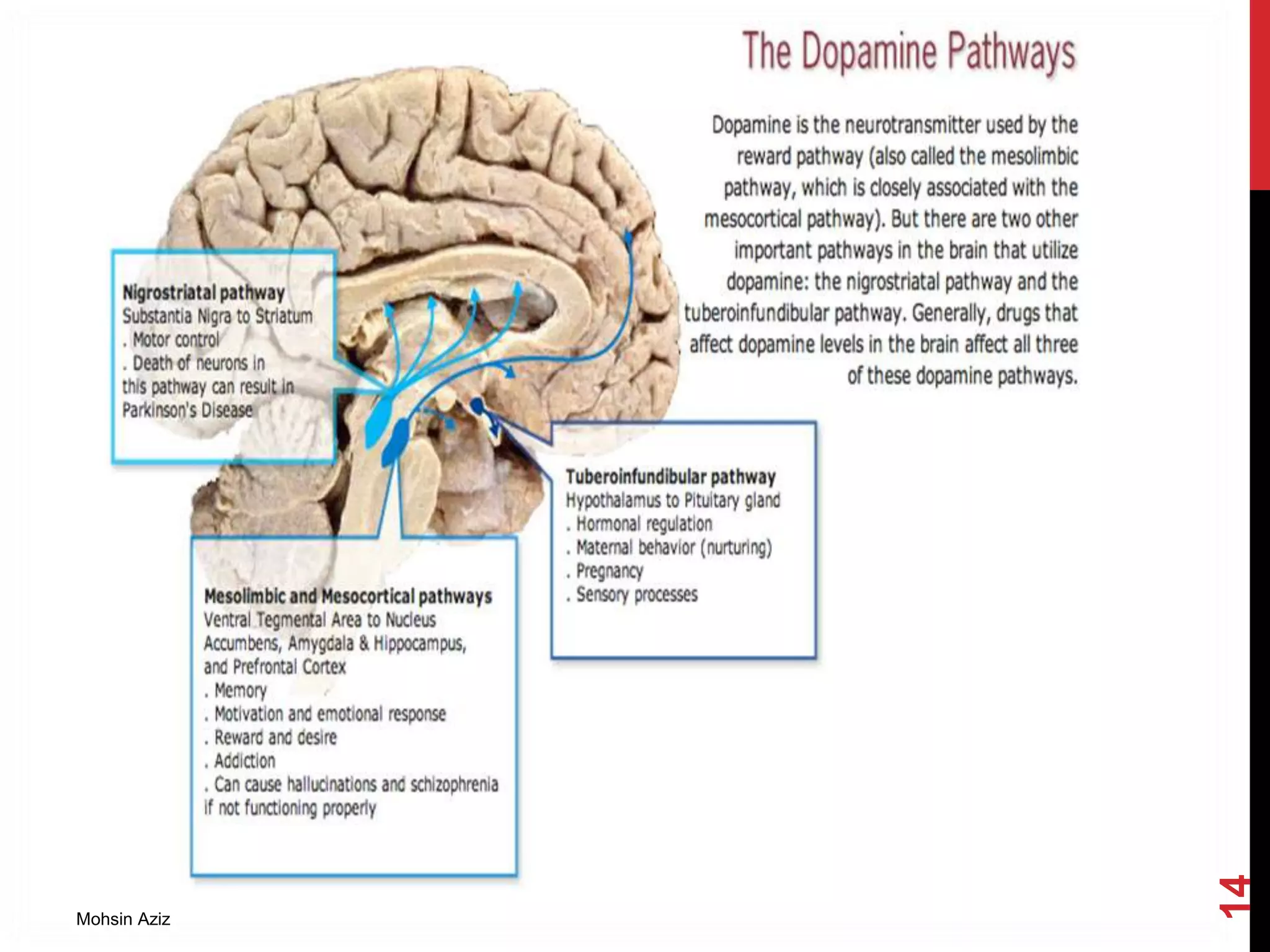
The document discusses neuroleptics, also known as antipsychotics, which are used to treat psychosis and schizophrenia by suppressing motor activity and emotionality. It details the symptoms and types of schizophrenia, the dopamine hypothesis linking excessive dopamine activity to positive symptoms, and the various classifications and effects of antipsychotic drugs. Furthermore, it addresses their mechanisms of action, side effects, and clinical uses in treating conditions like schizophrenia, nausea, and behavioral emergencies.

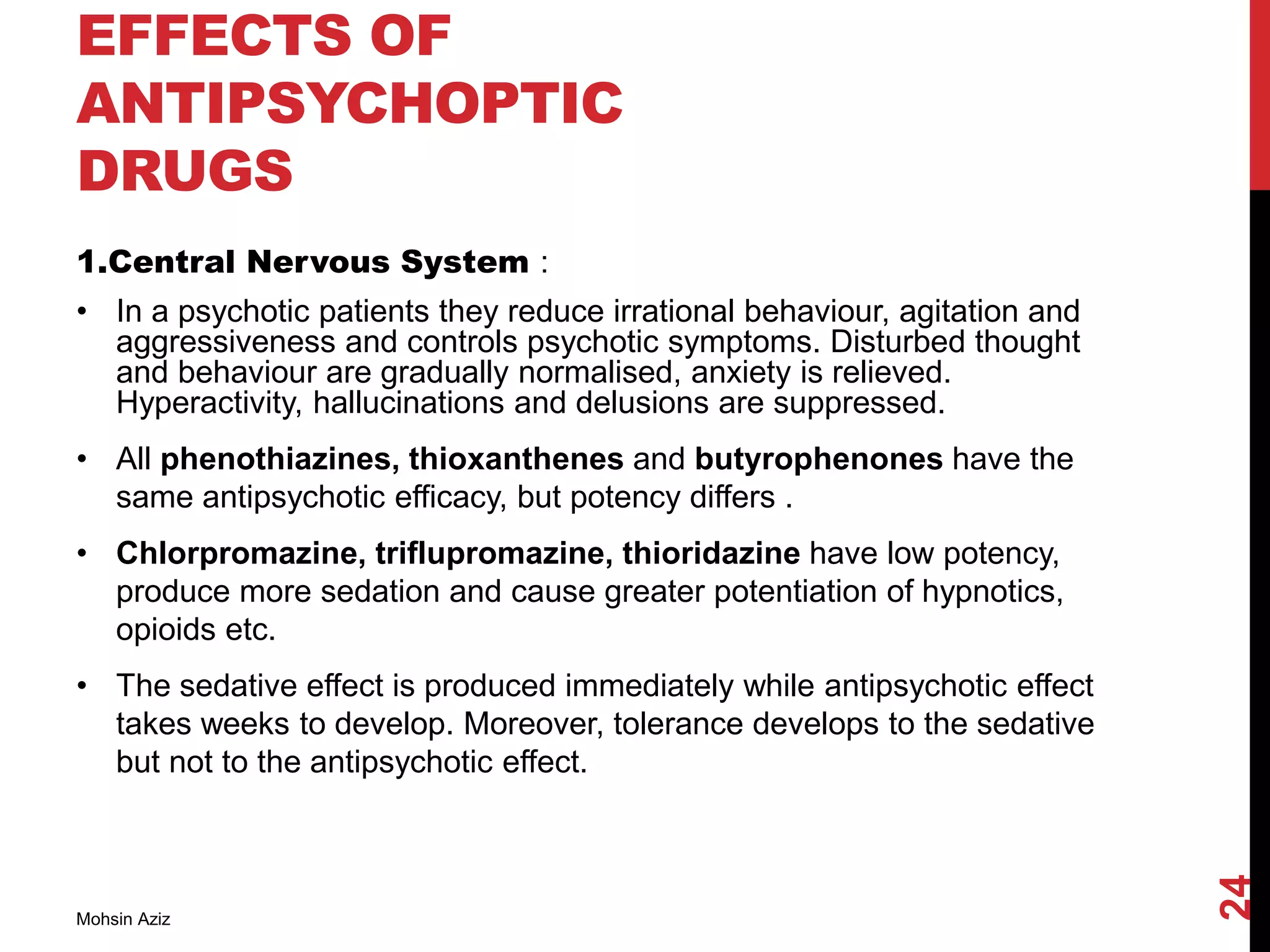
![THE DOPAMINE
HYPOTHESIS
Schizophrenia results from excess activity of dopamine
neurotransmission in Mesolimbic and Mesocortical Pathways
because:
All antipsychotic drugs block dopamine receptors.
Stimulant drugs which act through dopamine can produce schizophrenic-
like behaviors (eg.amphetamines).
Levodopa, a dopamine precursor, can exacerbate schizophrenic
symptoms, or occasionally elicit them in non-schizophrenic patients.
Higher levels of dopamine receptors measured in brains of schizophrenics
by PET.
Brain [DA] increases during psychotic episodes but not during remissions.
Mohsin Aziz
15](https://image.slidesharecdn.com/neurolepticsantipsychotics-140718132548-phpapp01/75/Neuroleptics-antipsychotics-15-2048.jpg)