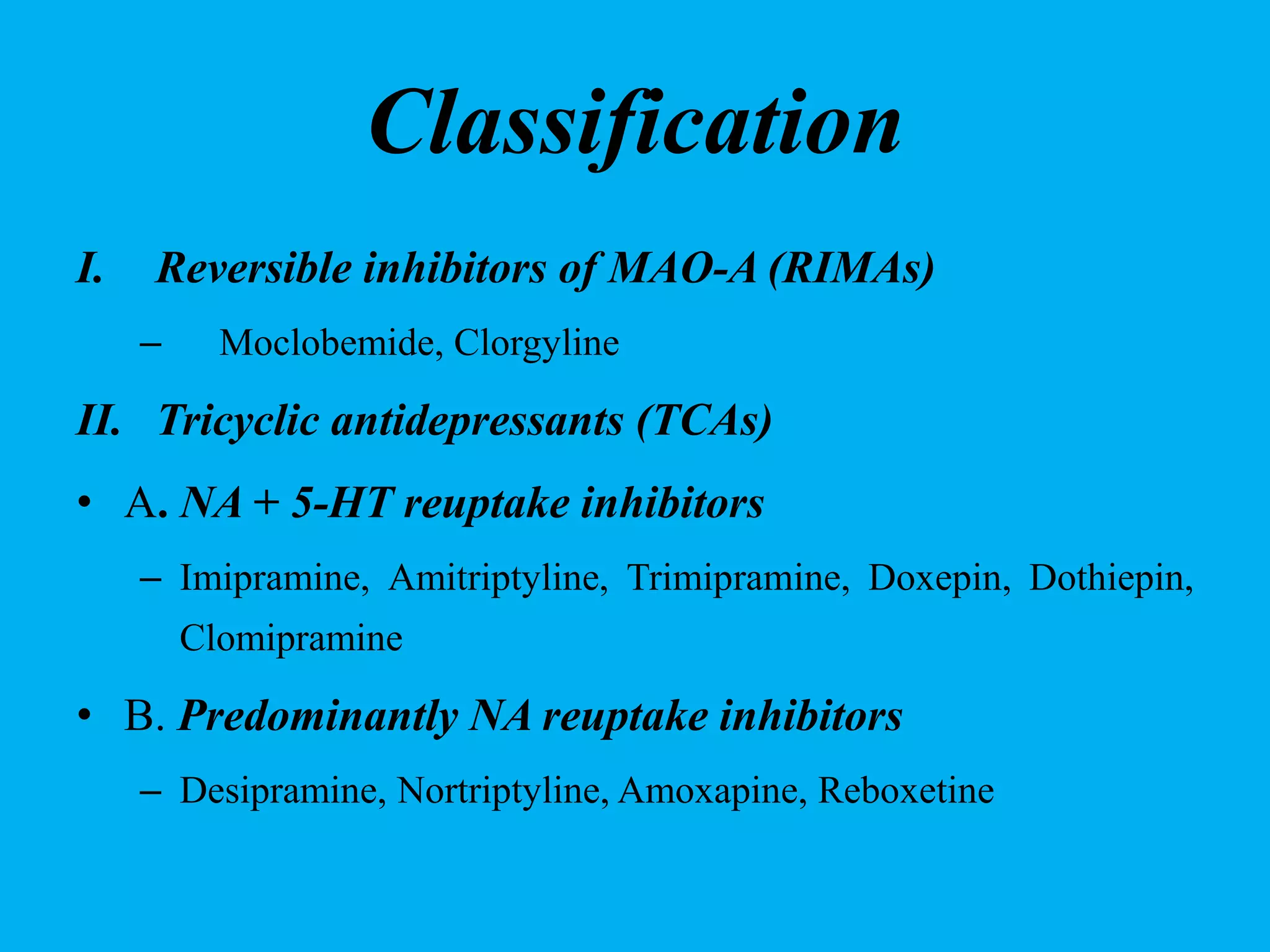
Antidepressants are medications primarily used to treat major depression and related conditions like anxiety and obsessive-compulsive disorders. They are classified into various groups, including tricyclic antidepressants, selective serotonin reuptake inhibitors, and monoamine oxidase inhibitors, each with unique mechanisms and side effects. Clinical practice emphasizes careful dosage and monitoring, especially in suicidal patients, and recommends combining therapy with medication for optimal treatment outcomes.