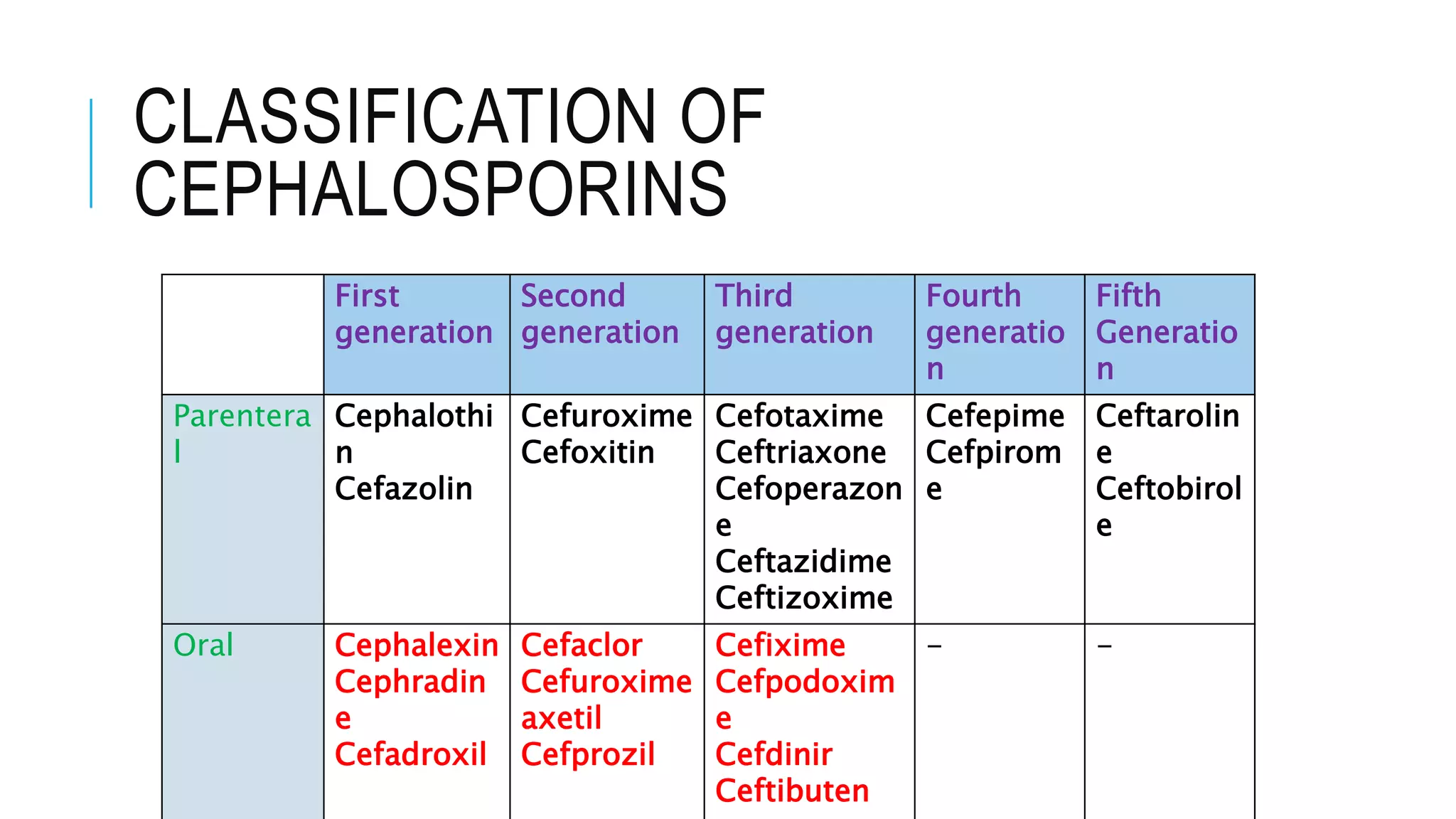
Cephalosporins are β-lactam antibiotics similar to penicillins, with a spectrum of action against various bacteria and classified into five generations. They possess a similar mechanism of action and resistance patterns, though each generation has distinct uses and pharmacokinetics. Common indications include treatment of respiratory infections, surgical prophylaxis, and urinary tract infections, while they may cause adverse effects such as allergic reactions and nephrotoxicity.