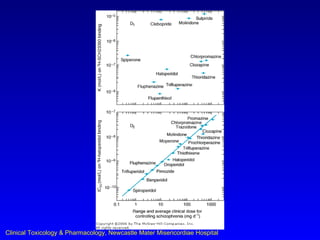
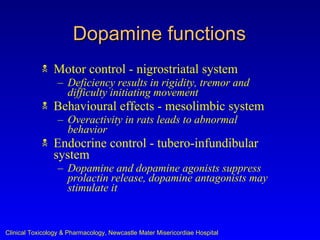
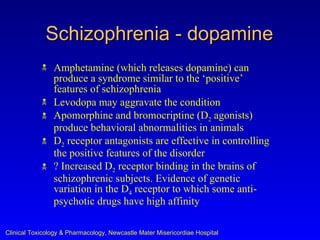
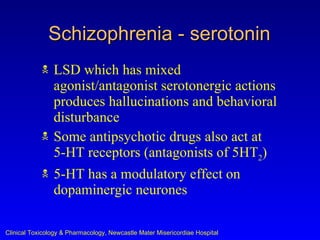
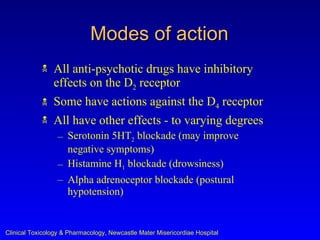
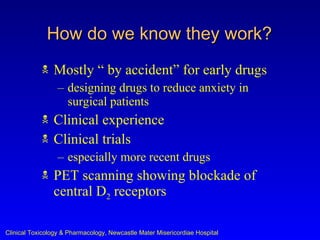
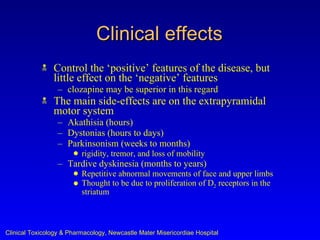
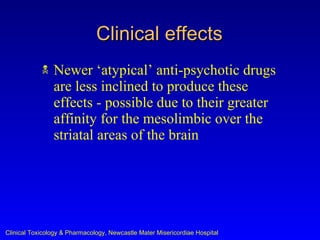
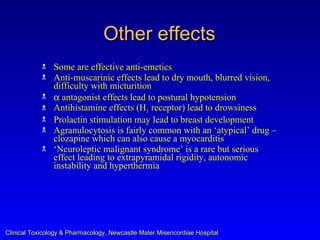
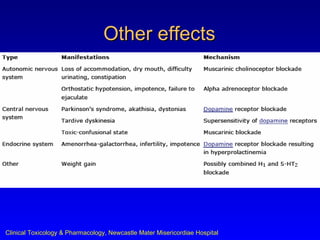
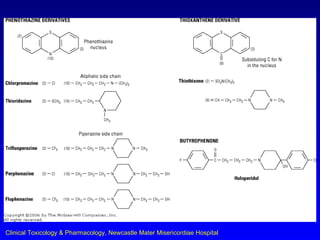
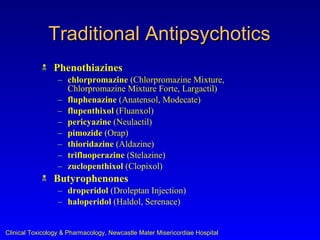
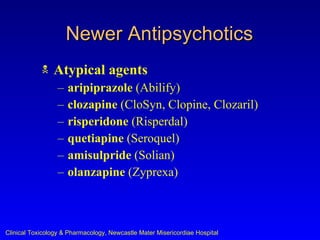
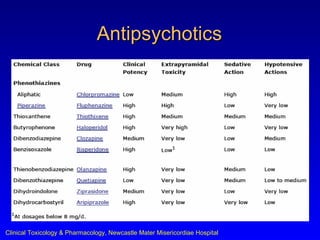
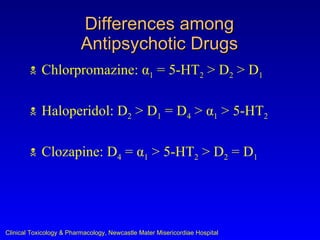
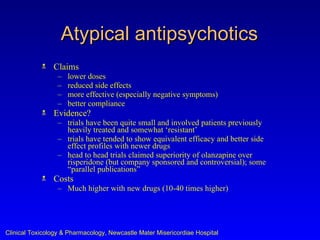
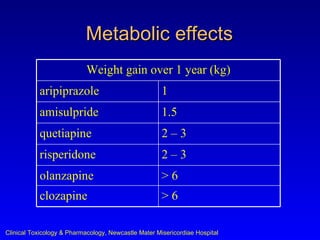
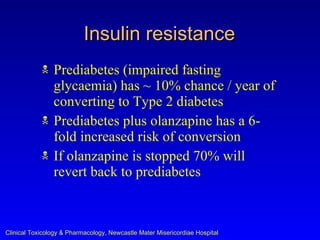
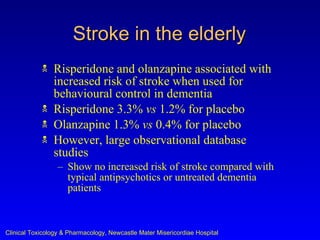
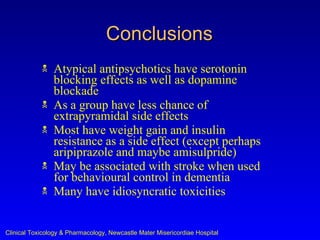
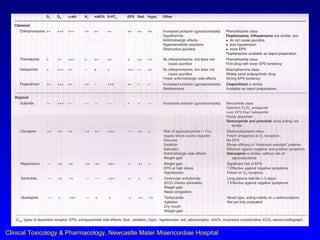
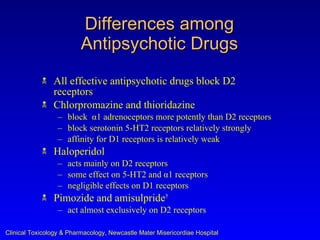
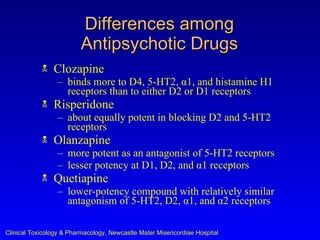
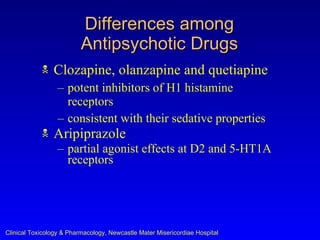
Antipsychotic drugs work by blocking dopamine D2 receptors in the brain. Traditional antipsychotics like haloperidol mainly target D2 receptors, while atypical antipsychotics also block serotonin 5-HT2 receptors. Atypical antipsychotics have fewer extrapyramidal side effects but greater risks of metabolic side effects like weight gain and insulin resistance compared to traditional antipsychotics. Antipsychotic drugs differ in their receptor binding profiles and side effect risks.