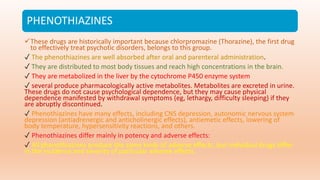
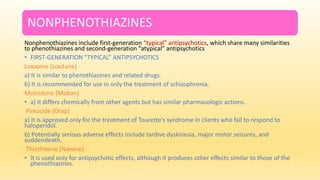
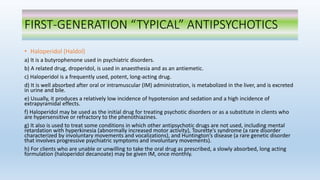
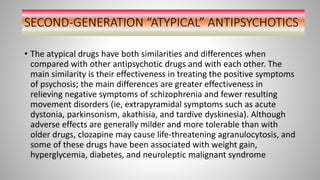
Antipsychotic drugs are primarily used to treat psychosis, including schizophrenia, and are divided into first-generation (typical) and second-generation (atypical) drugs, each with different efficacy and side effects. First-generation antipsychotics are associated with movement disorders, while second-generation ones have a lower risk of such effects but may lead to metabolic issues. Proper understanding of their mechanisms, pharmacokinetics, indications, and contraindications is crucial for effective treatment of mental disorders.





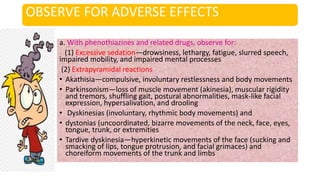
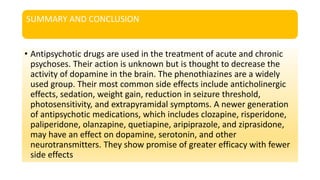
![12. Extrapyramidal symptoms (EPS)
*Observe for symptoms and report; administer antiparkinsonian drugs, as ordered .
a. Pseudoparkinsonism (tremor, shuffling gait, drooling, rigidity)
*Symptoms may appear 1 to 5 days following initiation of antipsychotic medication;
occurs most often in women, the elderly, and dehydrated clients.
b. Akinesia (muscular weakness)
*Same as for pseudoparkinsonism.
c. Akathisia (continuous restlessness and fidgeting)
*This occurs most frequently in women; symptoms may occur 50 to 60 days following
initiation of therapy.
d. Dystonia (involuntary muscular movements [spasms] of face, arms, legs, and neck)
*This occurs most often in men and in people younger than 25 years of age.
e. Oculogyric crisis (uncontrolled rolling back of the eyes)
*This may appear as part of the syndrome described as dystonia. It may be mistaken for
seizure activity. Dystonia and oculogyric crisis should be treated as an emergency situation.
The physician should be contacted, and intravenous benztropine mesylate (Cogentin) is
commonly administered. Stay with the client and offer reassurance and support during this
frightening time.](https://image.slidesharecdn.com/antipsychotictreatment-230227175155-e5ad30d1/85/ANTIPSYCHOTIC-TREATMENT-pptx-38-320.jpg)
![13. Tardive dyskinesia [bizarre facial and tongue movements, stiff neck, and difficulty swallowing] (may occur
with all classifications, but more common with typical antipsychotics)
*All clients receiving long-term (months or years) antipsychotic therapy are at risk.
*The symptoms are potentially irreversible.
*The drug should be withdrawn at the first sign, which is usually vermiform movements of the tongue; prompt
action may prevent irreversibility
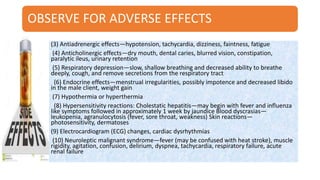
● Supervise ambulation to prevent falls or other injuries if the client is drowsy or elderly or has postural
hypotension.
● Several measures can help prevent or minimize hypotension, such as having the client lie down for
approximately an hour after a large oral dose or an injection of antipsychotic medication; applying elastic
stockings; and instructing the client to change positions gradually, elevate legs when sitting, avoid standing for
prolonged periods, and avoid hot baths (hot baths cause vasodilation and increase the incidence of
hypotension). In addition, the daily dose can be decreased or divided into smaller amounts.
● Dry mouth and oral infections can be decreased by frequently brushing the teeth; rinsing the mouth with
water; chewing sugarless gum or candy; and ensuring an adequate fluid intake. Excessive water intake should
be discouraged because it may lead to serum electrolyte deficiencies.
● The usual measures of increasing fluid intake, dietary fiber, and exercise can help prevent constipation.
● Support caregivers in efforts to maintain contact with inpatients and provide care for outpatients. One way is
to provide caregivers with telephone numbers of health care providers and to make periodic telephone calls to
caregivers.
● Provide client teaching regarding drug therapy](https://image.slidesharecdn.com/antipsychotictreatment-230227175155-e5ad30d1/85/ANTIPSYCHOTIC-TREATMENT-pptx-39-320.jpg)