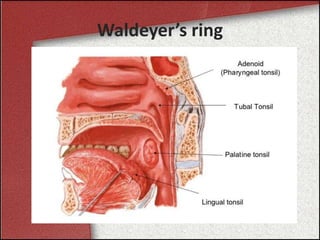
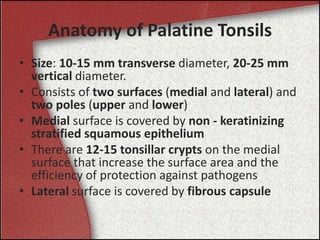
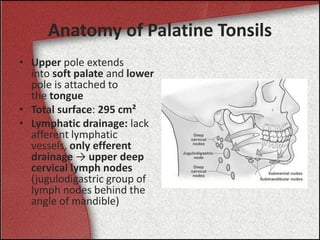
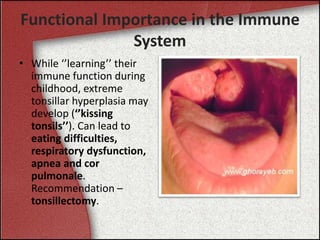
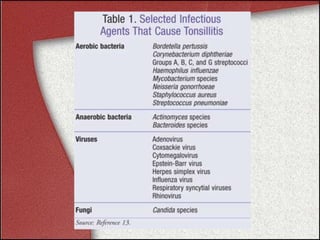
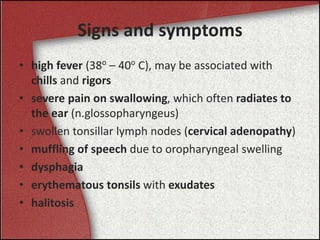
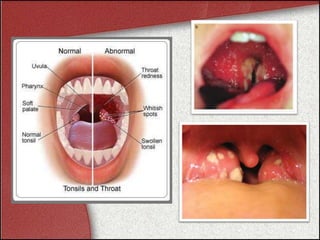
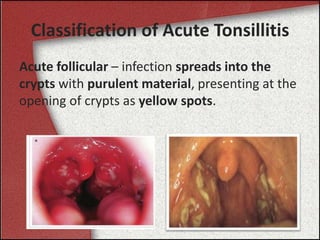
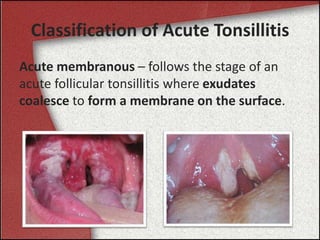
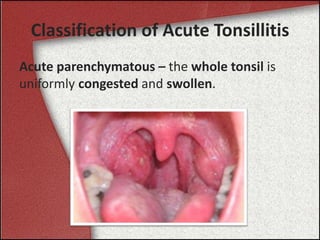
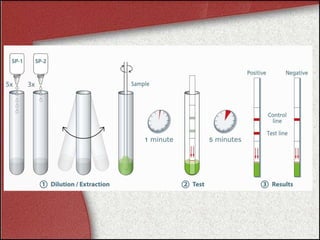
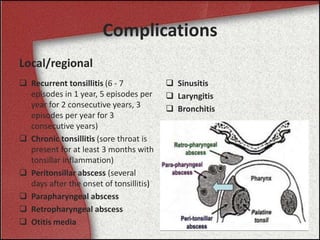
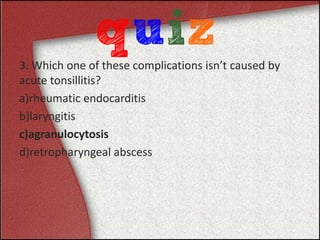
The document provides a comprehensive overview of acute tonsillitis, including its anatomy, functional importance in the immune system, epidemiology, etiology, signs and symptoms, classification, diagnosis, treatment, and complications. It highlights that Group A beta-hemolytic streptococcus is the most common bacterial cause, affecting mainly children aged 5 to 15. The document also describes a clinical case exemplifying the symptoms and treatment of bacterial tonsillitis.