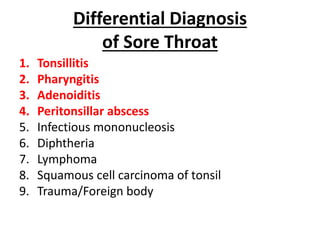
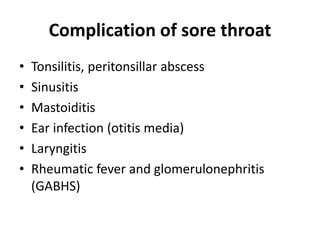
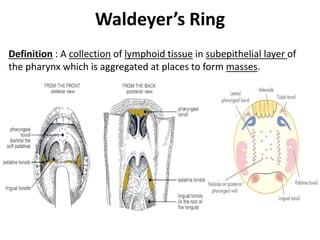
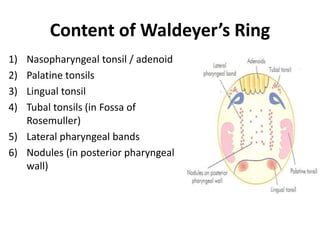
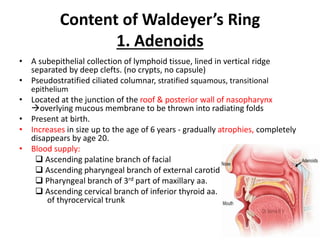
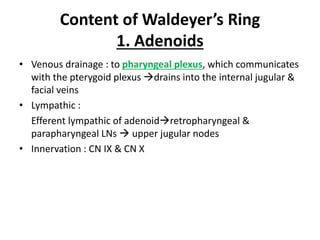
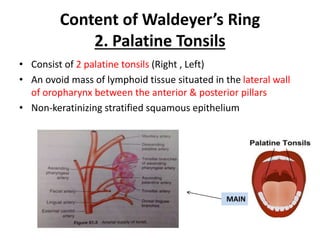
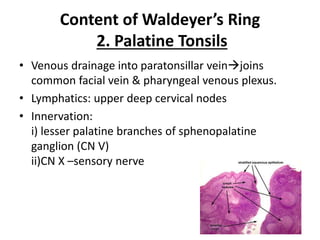
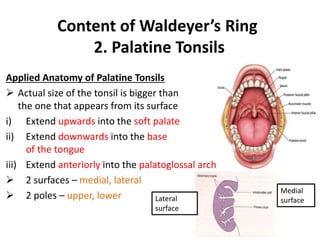
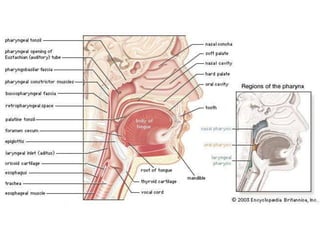
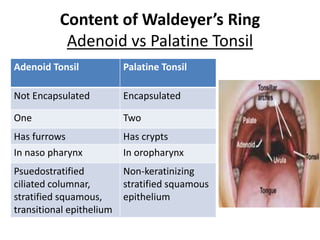
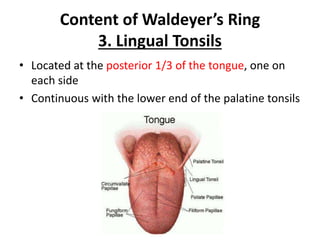
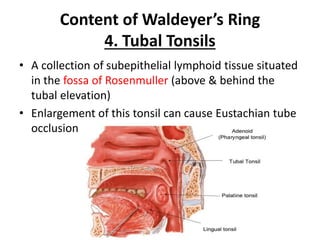
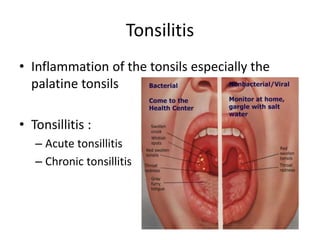
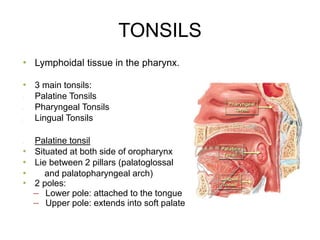
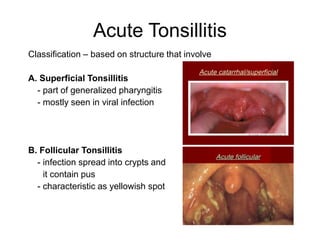
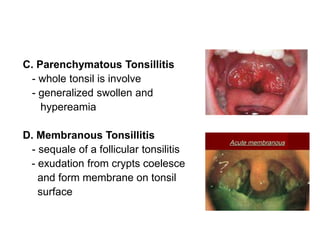
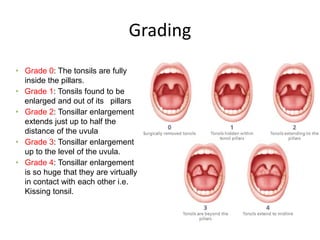
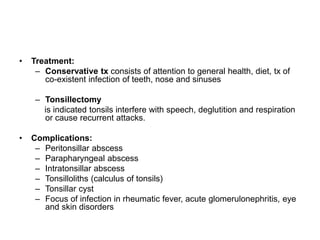
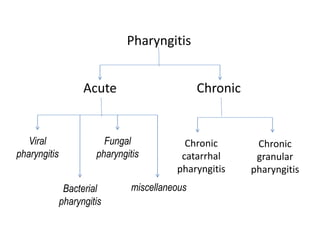
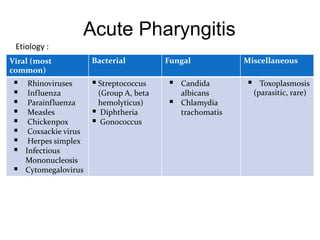
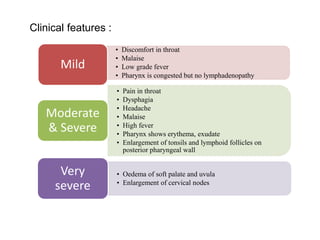
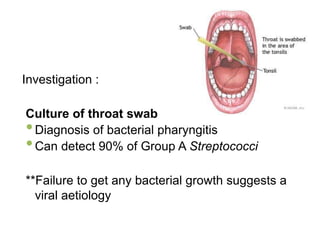
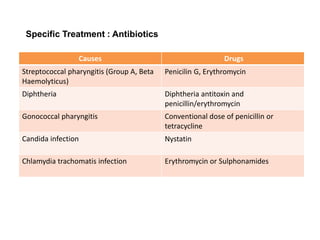
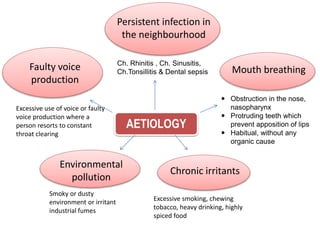
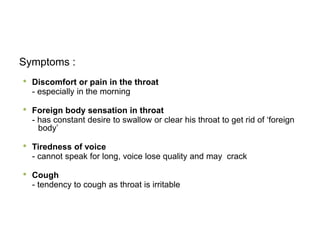
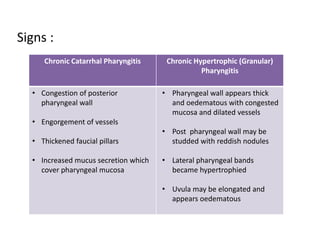
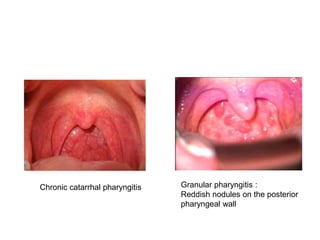
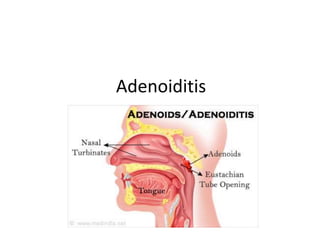
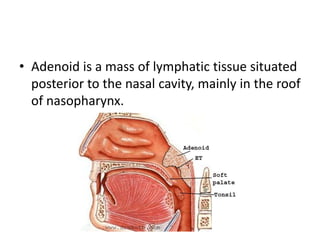
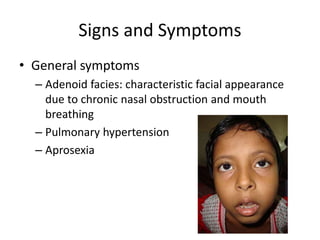
Waldeyer's ring consists of lymphoid tissue in the pharynx including the palatine tonsils, lingual tonsils, tubal tonsils, and adenoids. The document discusses the anatomy, histology, blood supply, innervation and functions of these structures. It also covers common conditions that involve the tonsils such as tonsillitis, peritonsillar abscess, adenoiditis and pharyngitis. The causes, signs, symptoms and treatment of these conditions are described.