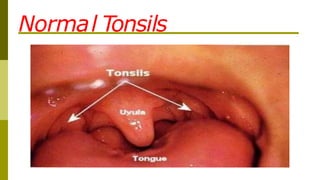
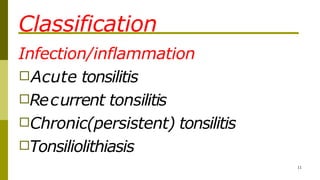
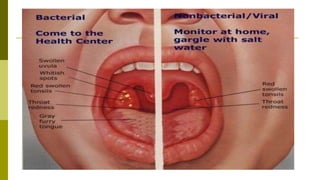
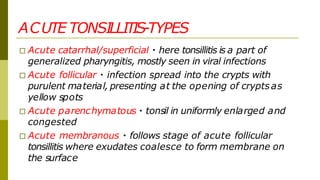
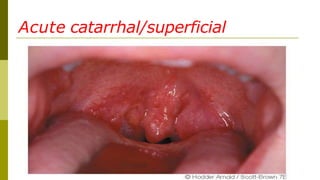
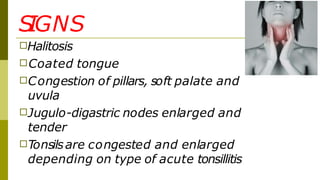
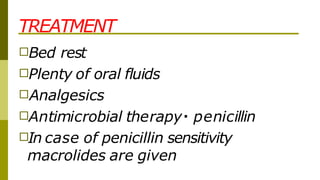
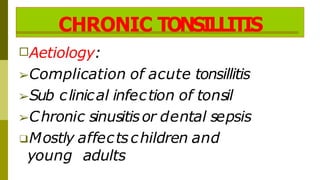
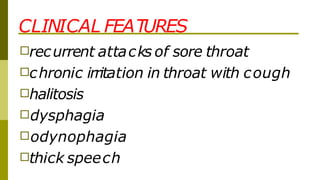
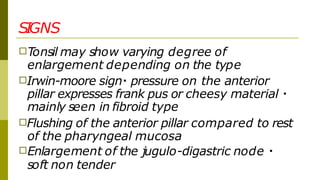
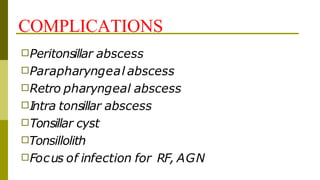
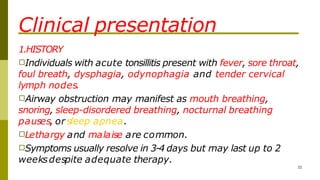
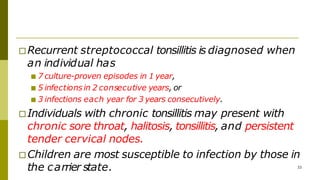
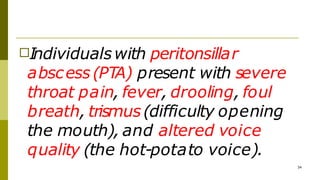
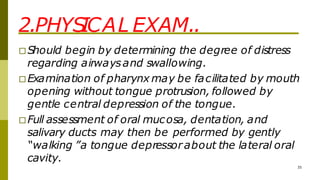
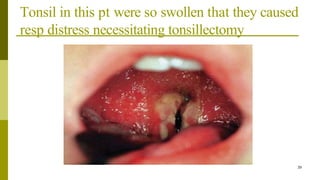
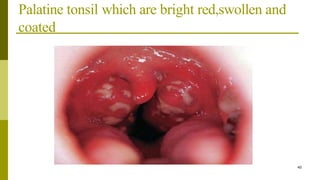
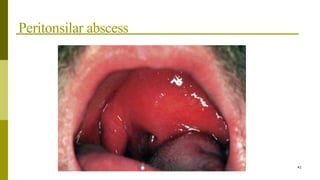
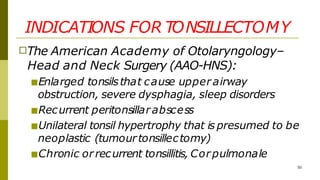
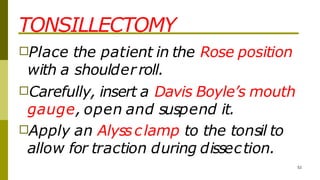
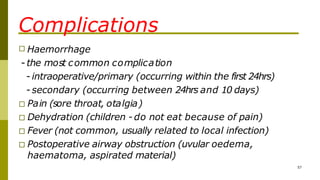
Tonsillitis is inflammation of the palatine tonsils caused by viral or bacterial infection. Common symptoms include sore throat, fever, and tender cervical lymph nodes. Physical examination reveals enlarged, inflamed tonsils that may have exudates. Throat culture is the standard test to detect Group A Streptococcus infection. Treatment involves pain relief, antibiotics if streptococcal infection is confirmed, and tonsillectomy for recurrent or chronic cases.