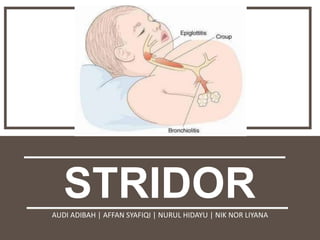
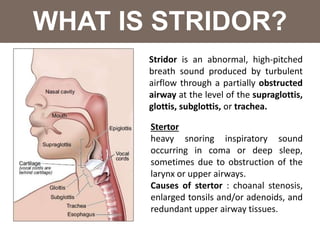
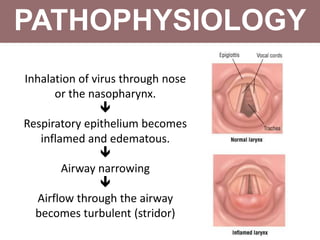
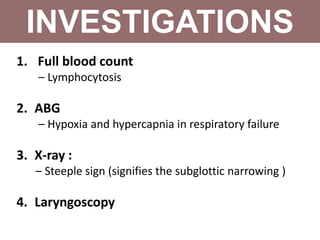
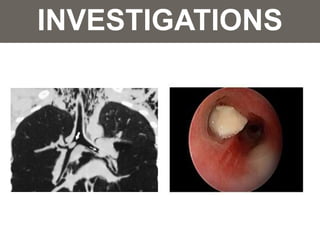
Stridor is an abnormal high-pitched sound caused by turbulent airflow through a partially obstructed airway, while stertor refers to heavy snoring during deep sleep. Common causes of stridor include congenital conditions like laryngomalacia and acquired issues such as acute epiglottitis and foreign body aspiration, particularly in children. Diagnostics involve clinical assessments, imaging, and potential interventions to manage the underlying causes and prevent respiratory failure.