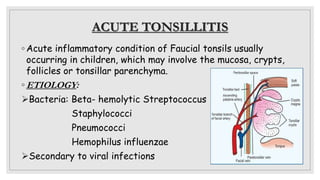
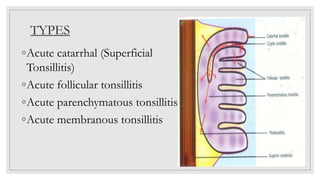
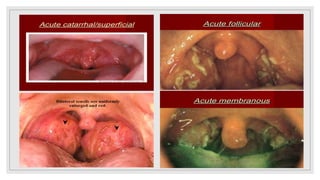
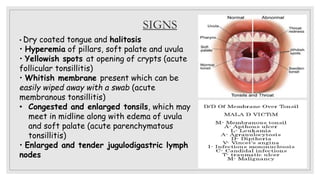
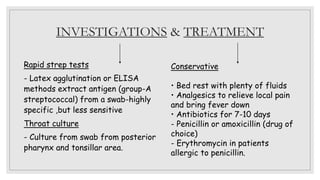
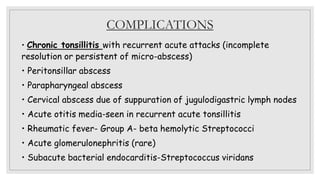
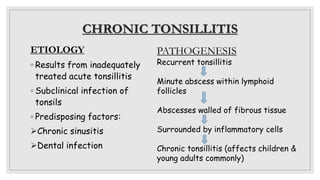
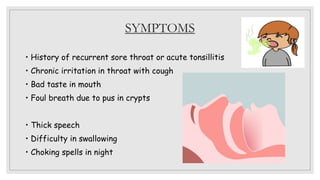
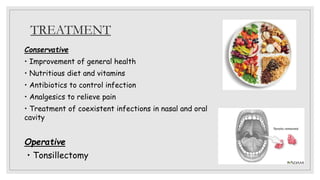
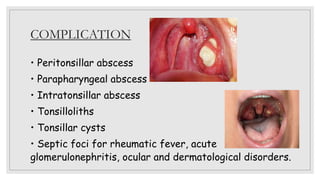
Acute tonsillitis is usually caused by bacteria and viruses infecting the tonsils. It causes sore throat, fever, earache, and enlarged lymph nodes. Examination may reveal spots in the tonsil crypts or white membranes. Rapid strep tests or throat culture can detect bacteria. Treatment involves rest, fluids, analgesics, and antibiotics like penicillin. Complications can include abscesses, rheumatic fever, or kidney problems. Chronic tonsillitis results from untreated acute infections and causes recurrent sore throats, bad breath, and difficulty swallowing. Treatment may involve antibiotics or tonsillectomy to prevent complications.