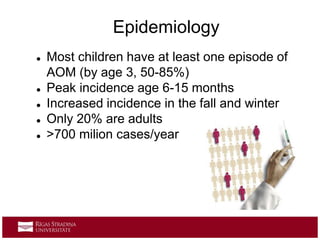
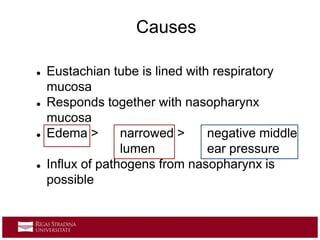
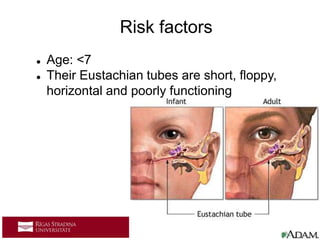
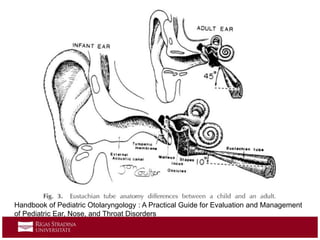
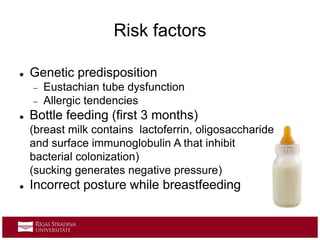
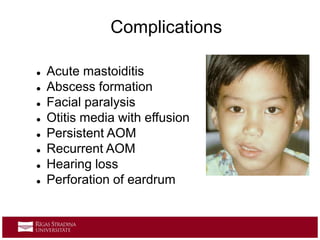
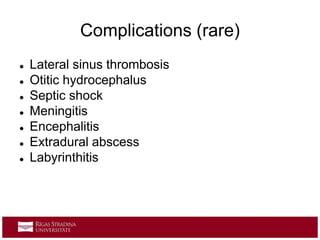
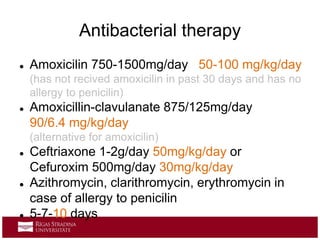
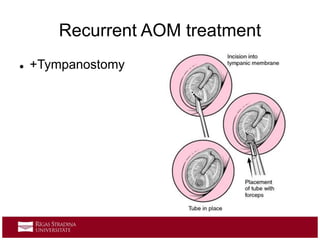
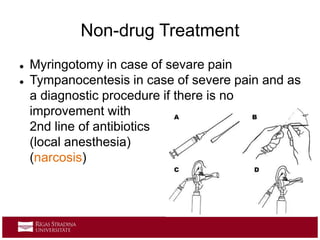
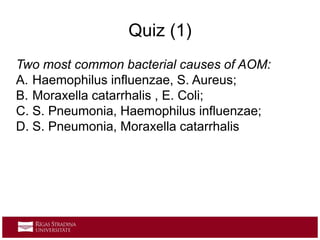
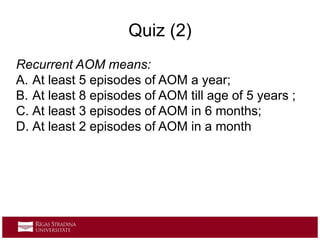
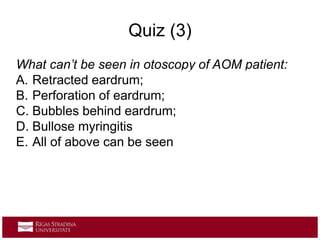
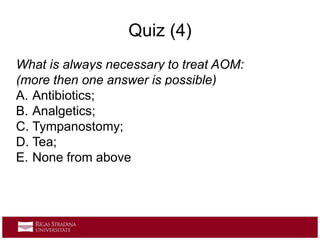
Acute otitis media (AOM) is a common middle ear inflammation often related to viral upper respiratory infections, particularly in children under five. Risk factors include eustachian tube dysfunction, allergies, and exposure to smoke, with primary symptoms including ear pain, fever, and hearing loss. Treatment may involve antibiotics, pain management, and preventive measures such as vaccinations and avoiding risk factors.