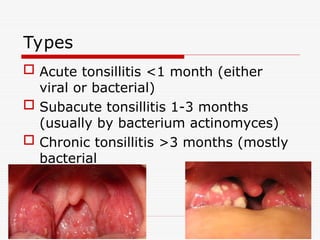
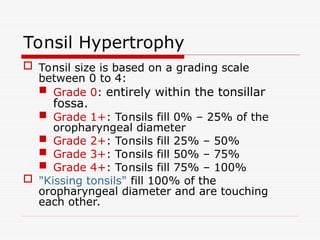
The document provides a comprehensive overview of tonsillitis, including its embryology, anatomy, epidemiology, etiology, clinical symptoms, and management. It highlights the development of tonsils, causes of inflammation, and the differentiation between acute, subacute, and chronic tonsillitis and outlines the diagnosis and treatment options. Additionally, it addresses complications and indications for surgical intervention like tonsillectomy.