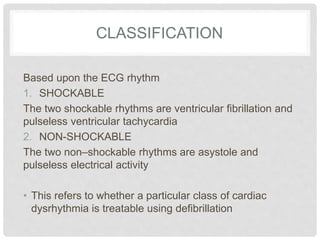
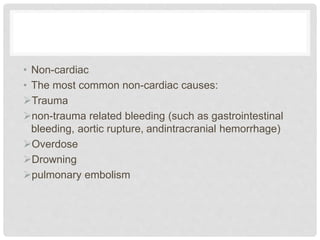
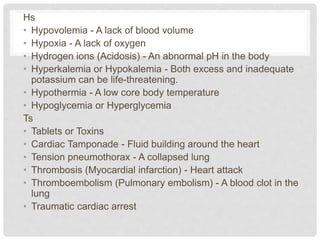
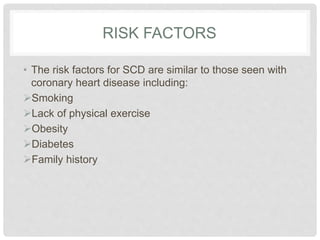
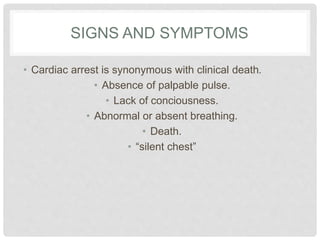
Cardiac arrest is the failure of the heart to effectively pump blood throughout the body due to problems with the electrical signals that control heart rhythm or other causes. It can be classified as either shockable or non-shockable based on the heart rhythm. Causes include coronary heart disease, cardiomyopathy, arrhythmias, and non-cardiac factors like bleeding or overdose. Treatment involves cardiopulmonary resuscitation, defibrillation for shockable rhythms, medications, therapeutic hypothermia, and other advanced techniques to restore circulation.