This document provides information on sudden cardiac death (SCD), including its definition, epidemiology, risk factors, etiologies, and prevention. Some key points:
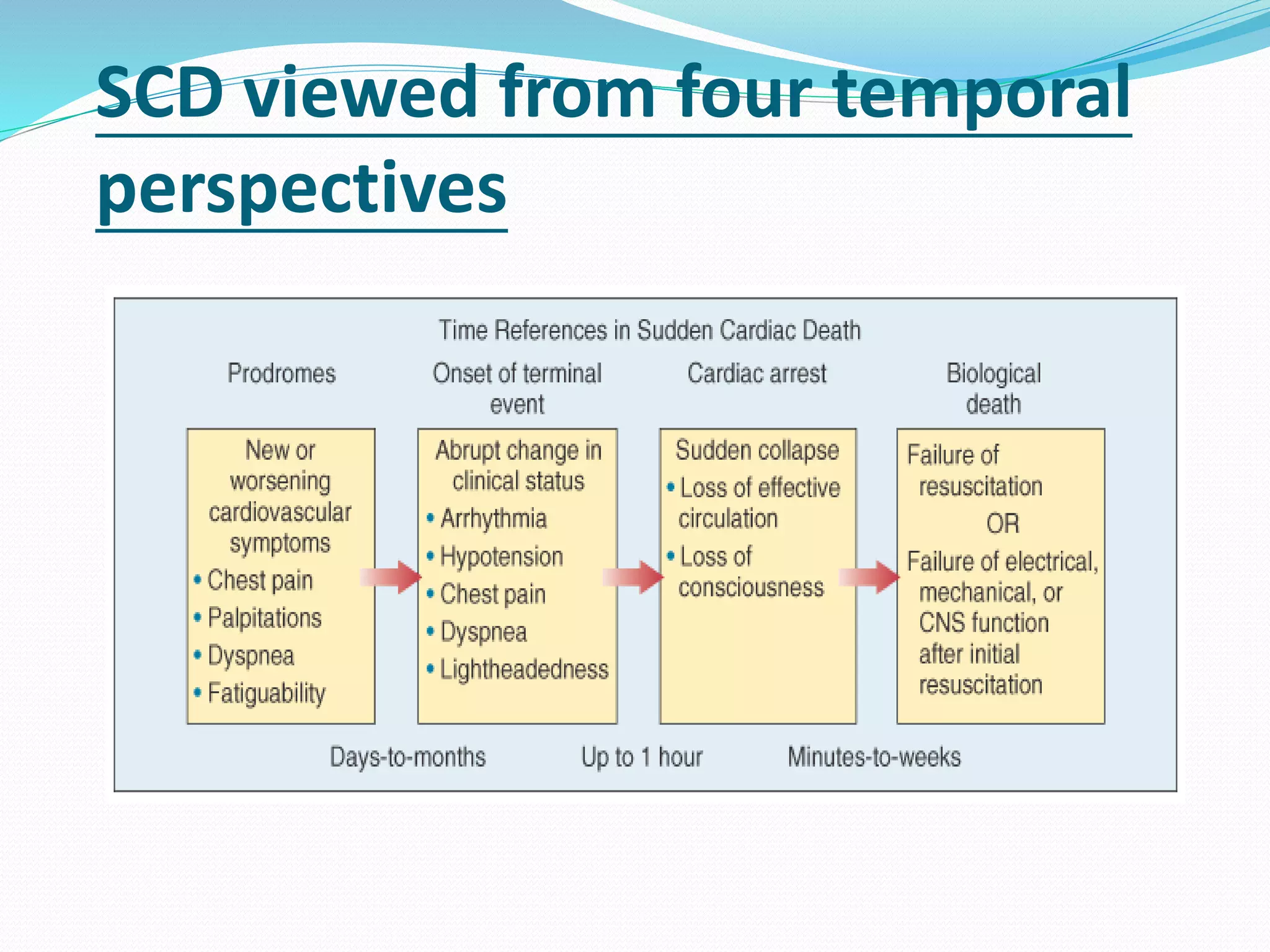
- SCD is defined as a natural death from cardiac causes within 1 hour of symptoms. It is a major cause of mortality, accounting for 10-15% of natural deaths.
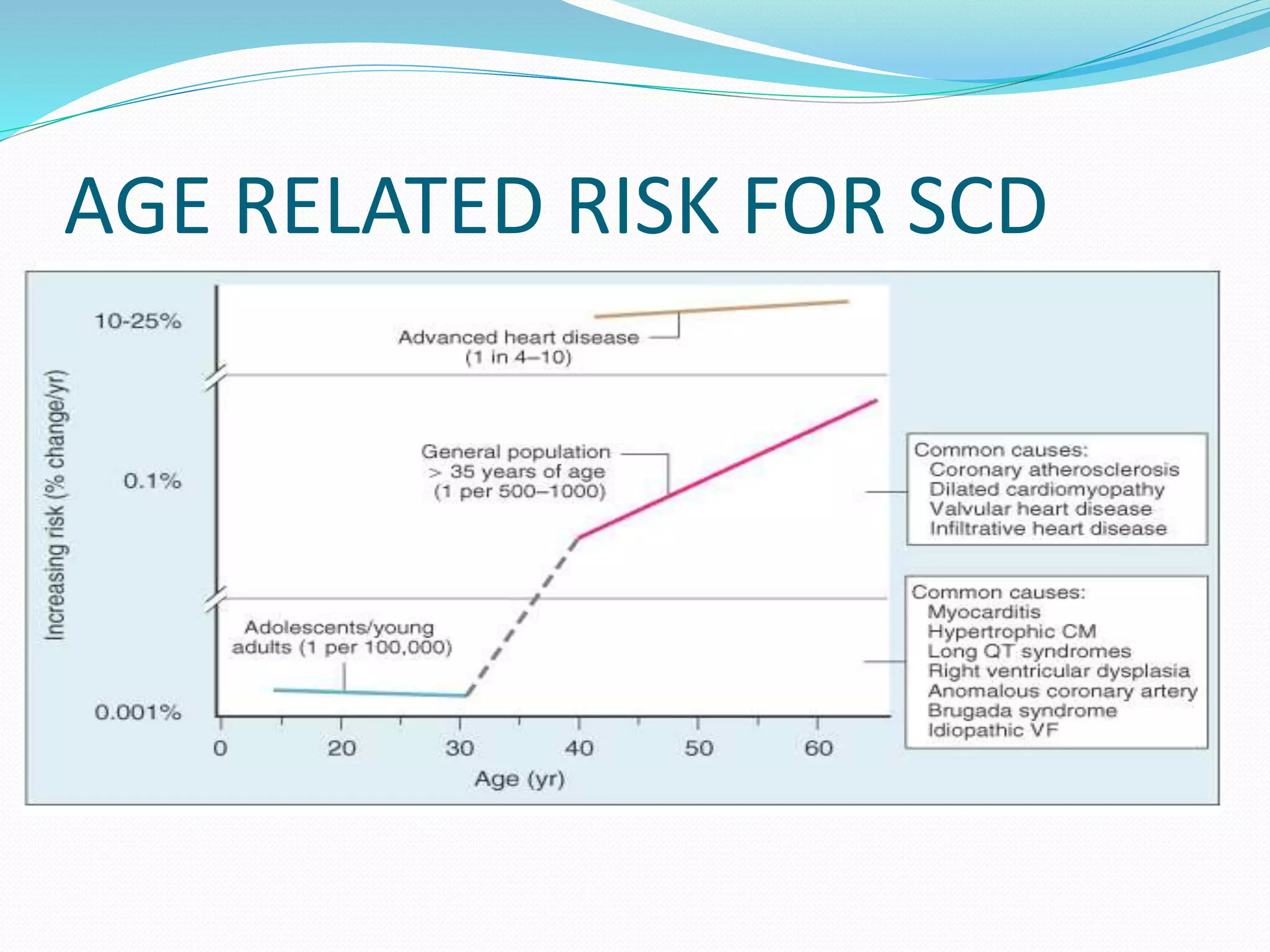
- Risk factors include prior heart disease, low ejection fraction, family history, and cardiomyopathy. The risk is bimodal with peaks under 1 year old and over 65 years old.
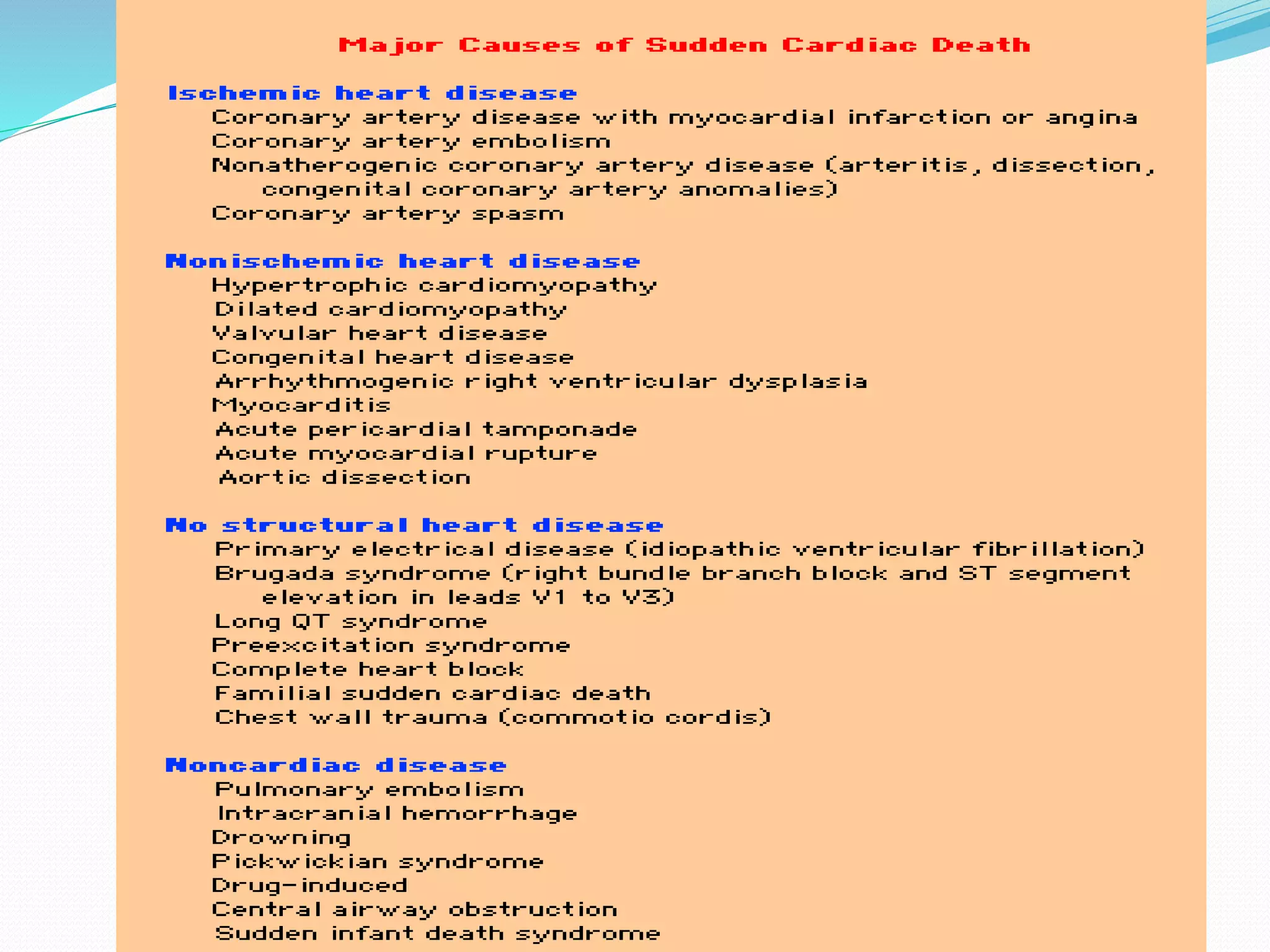
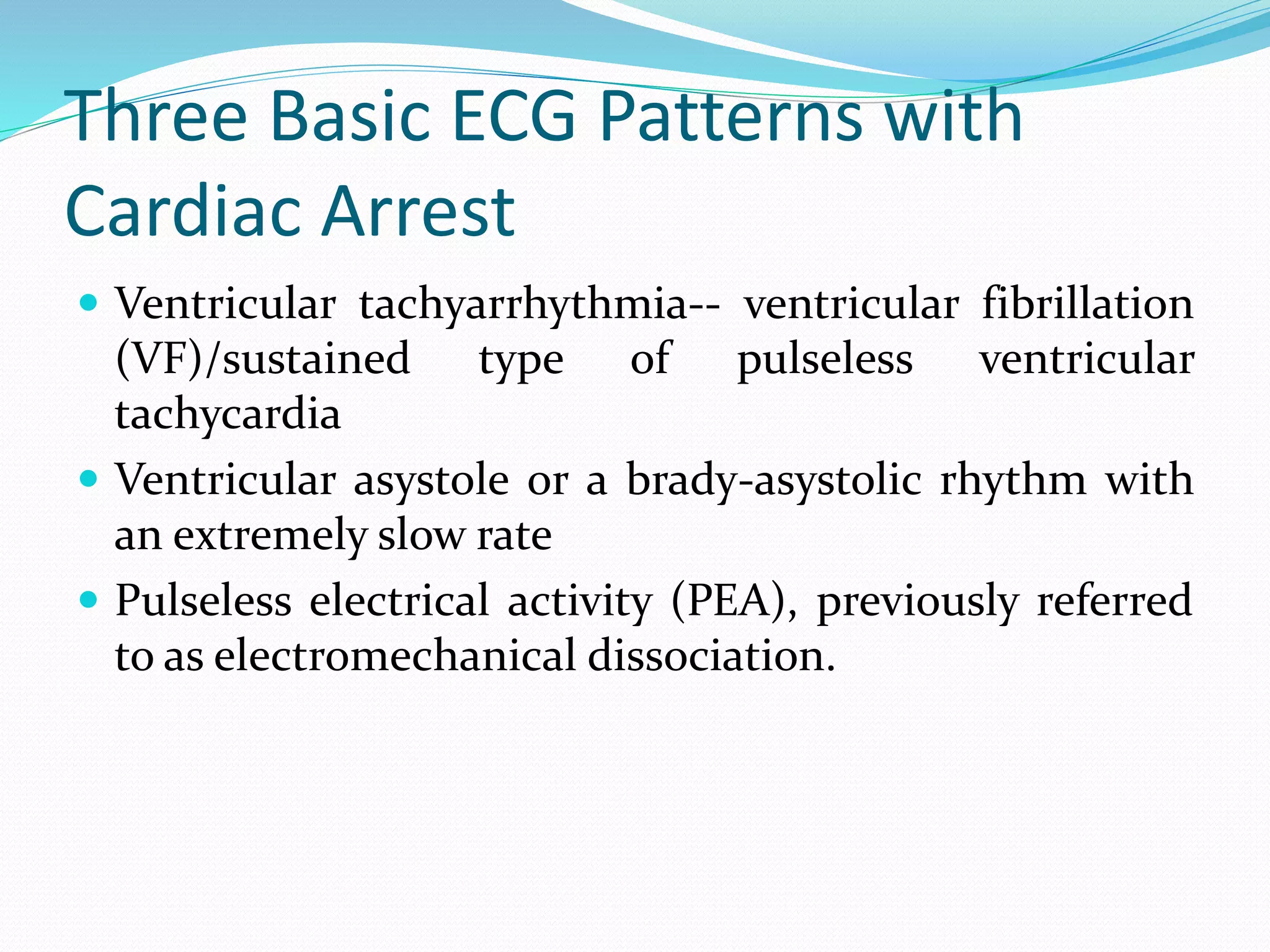
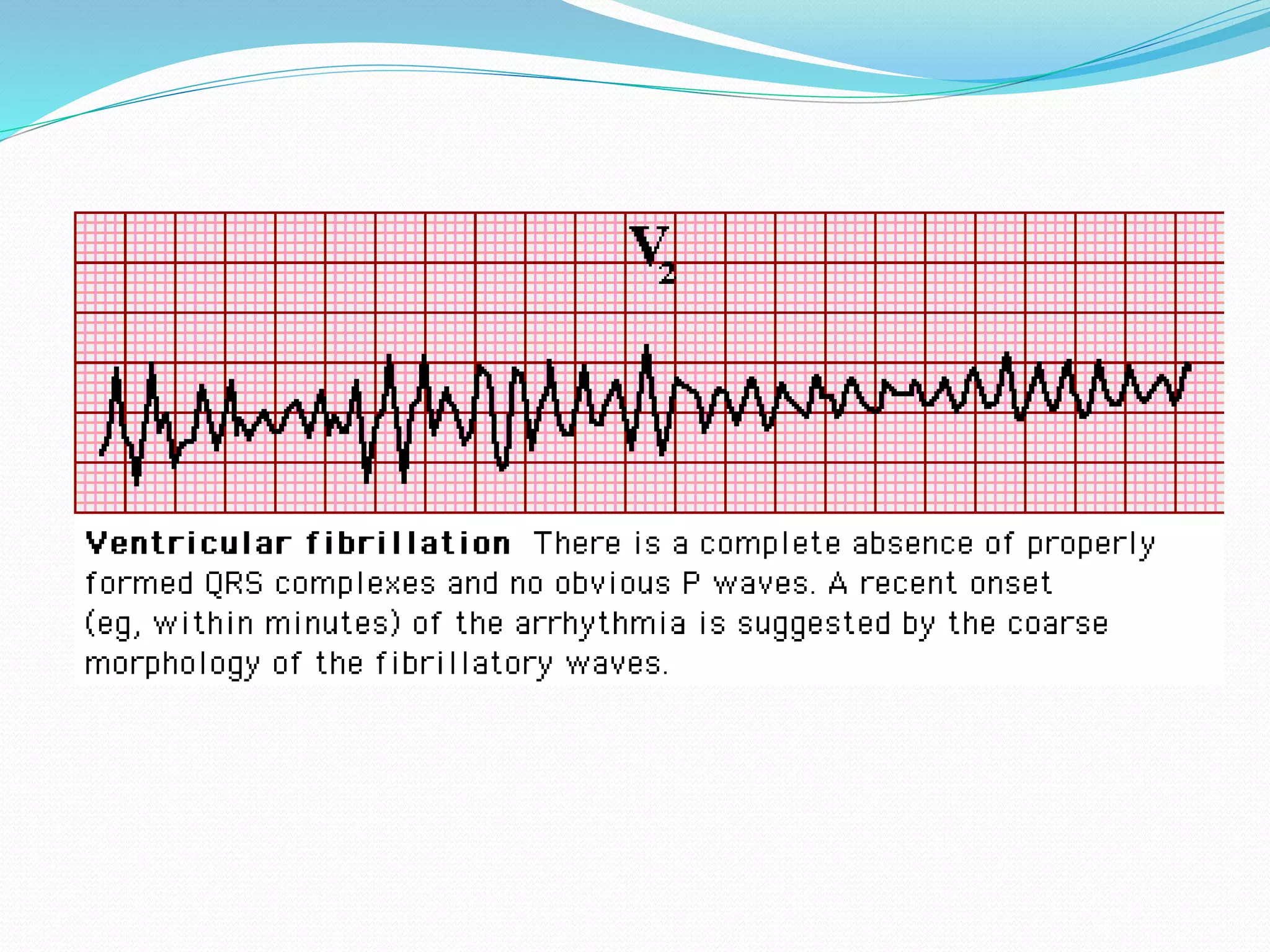
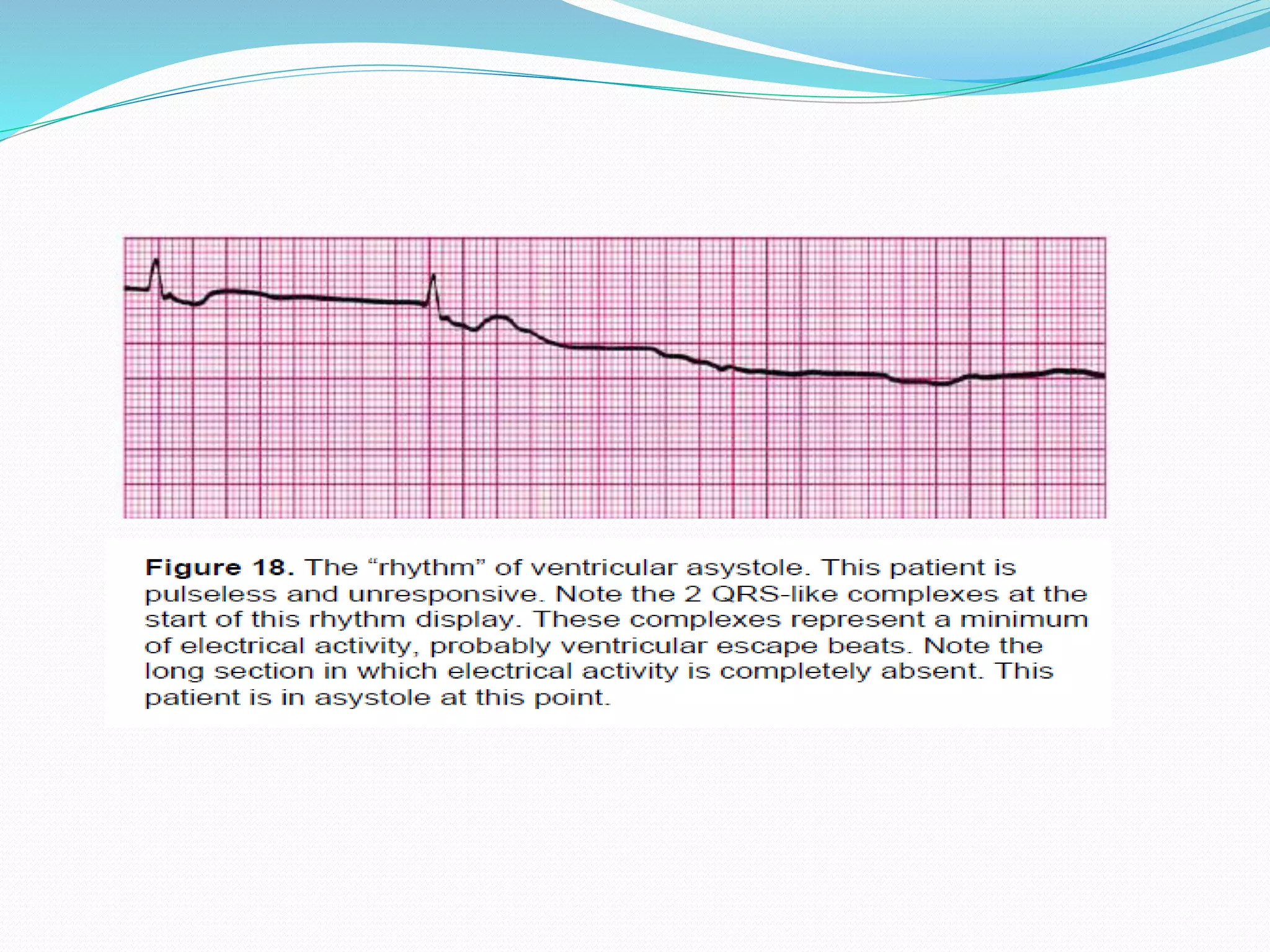
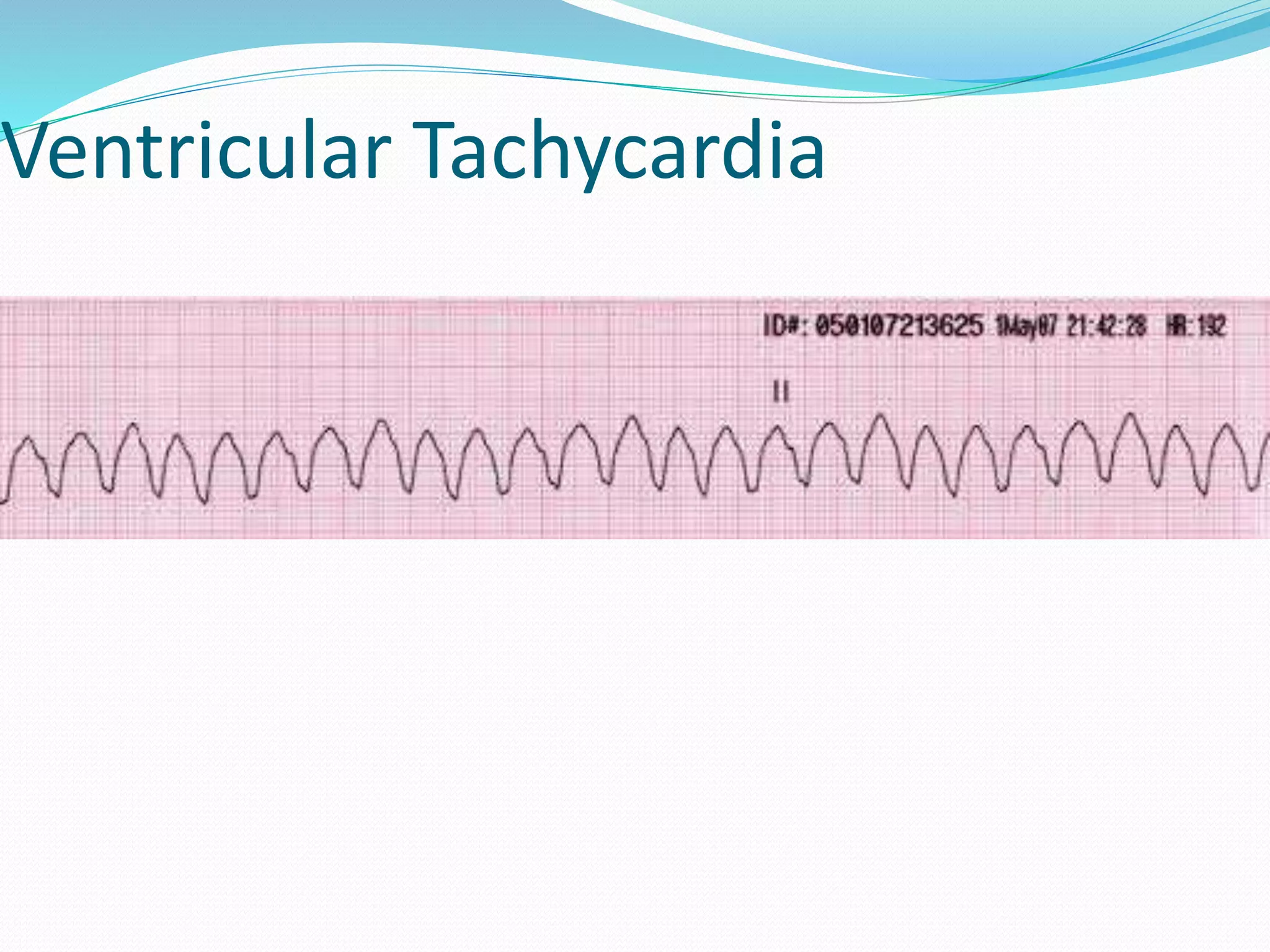
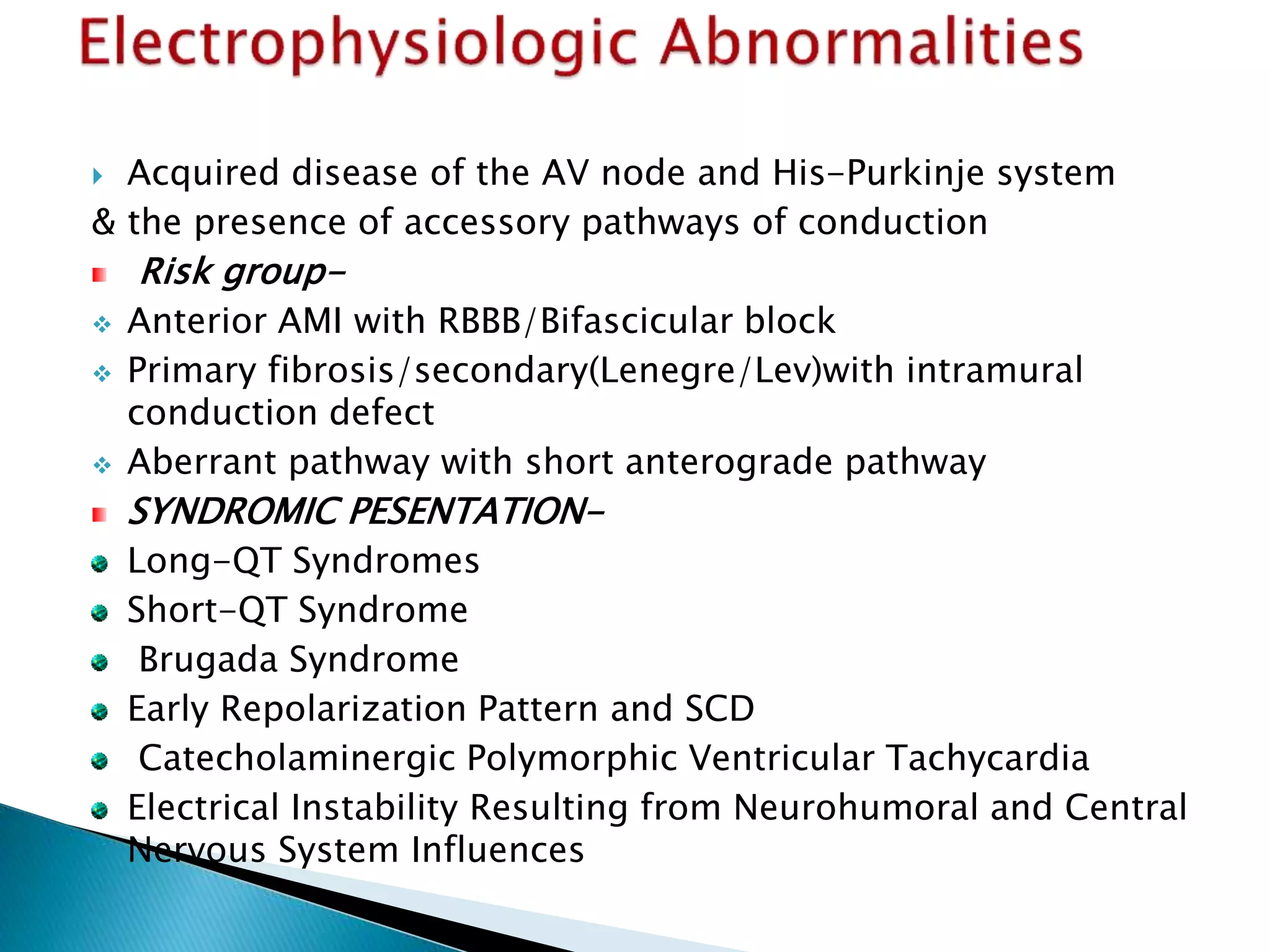
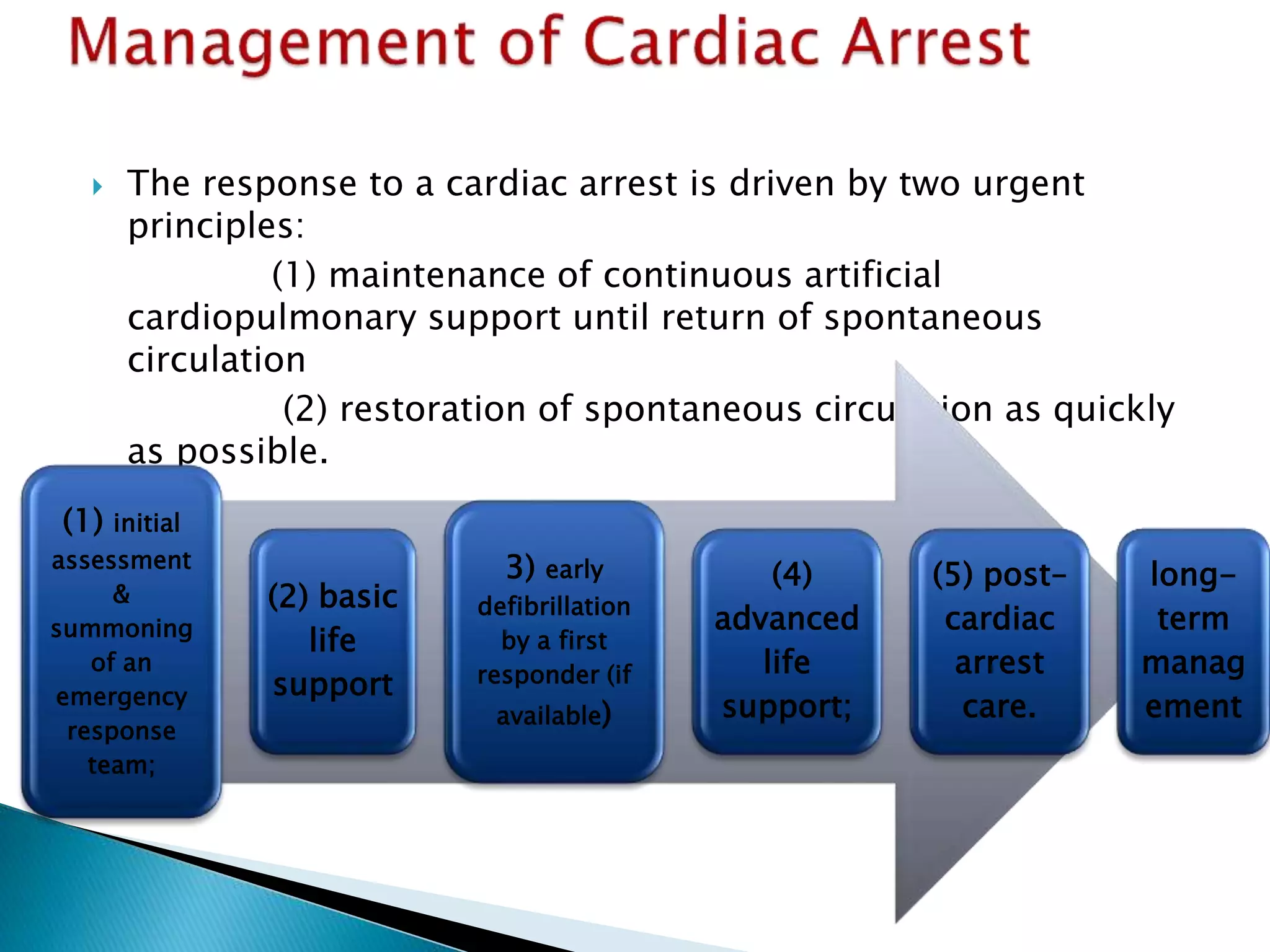
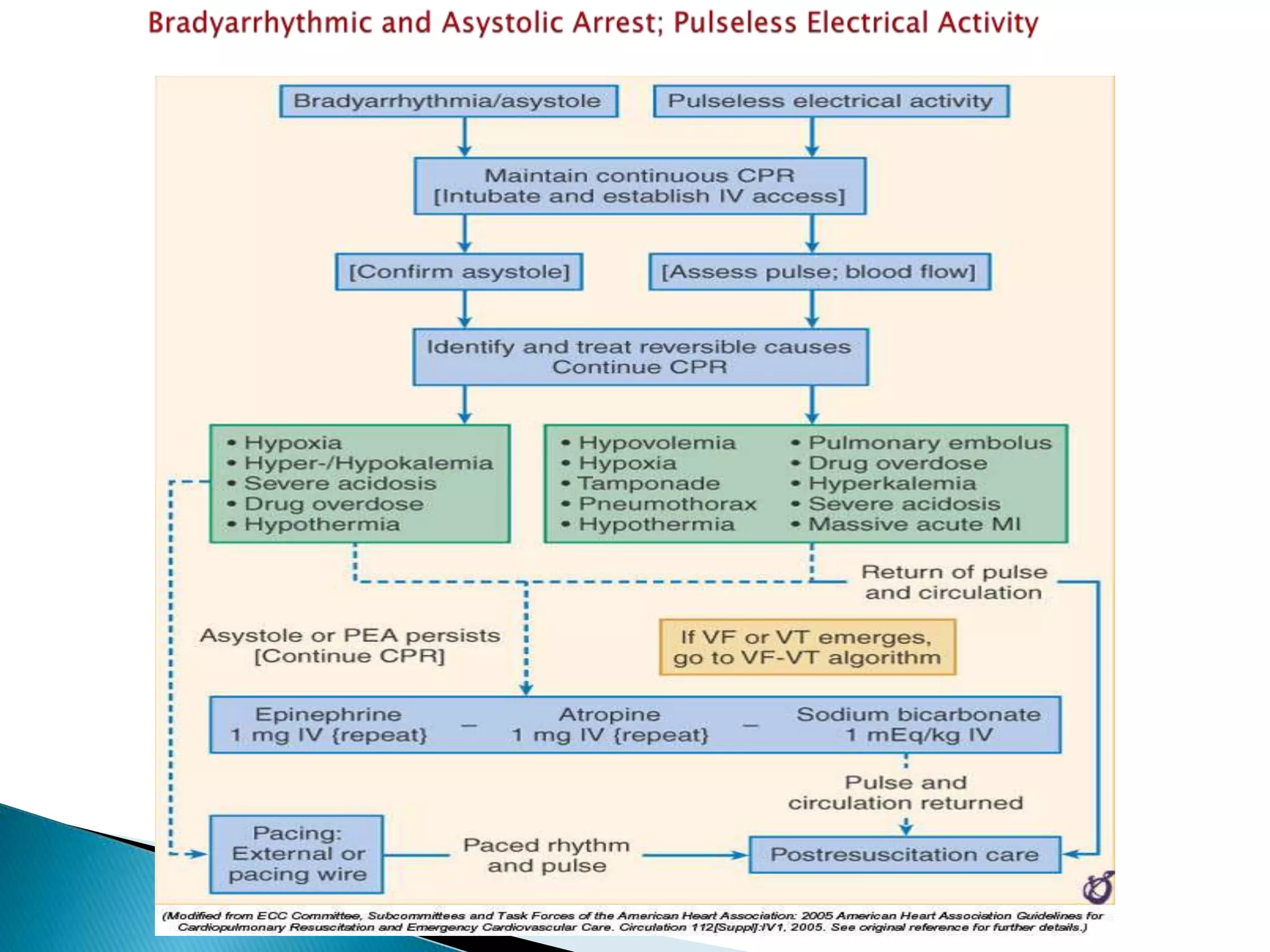
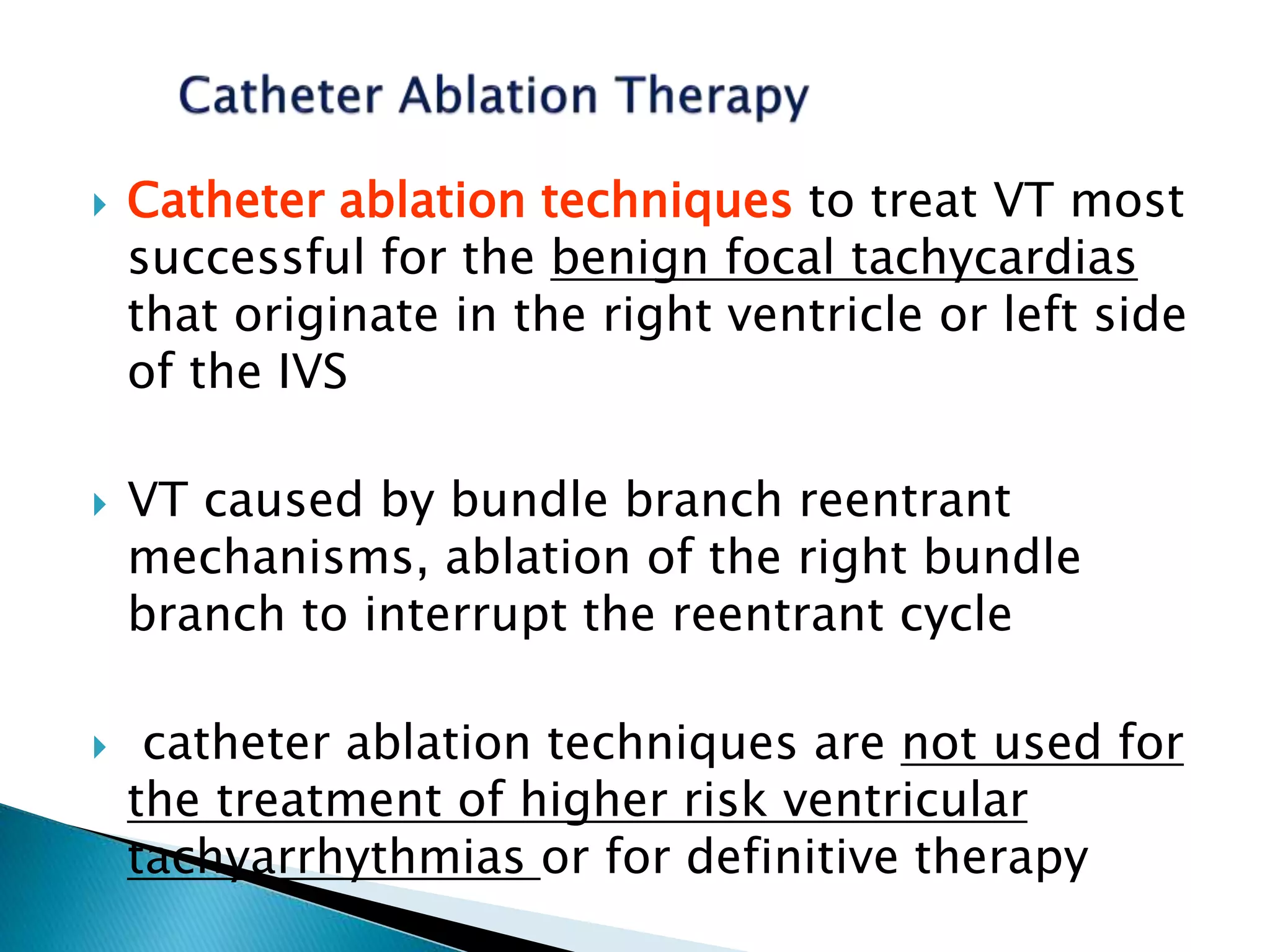
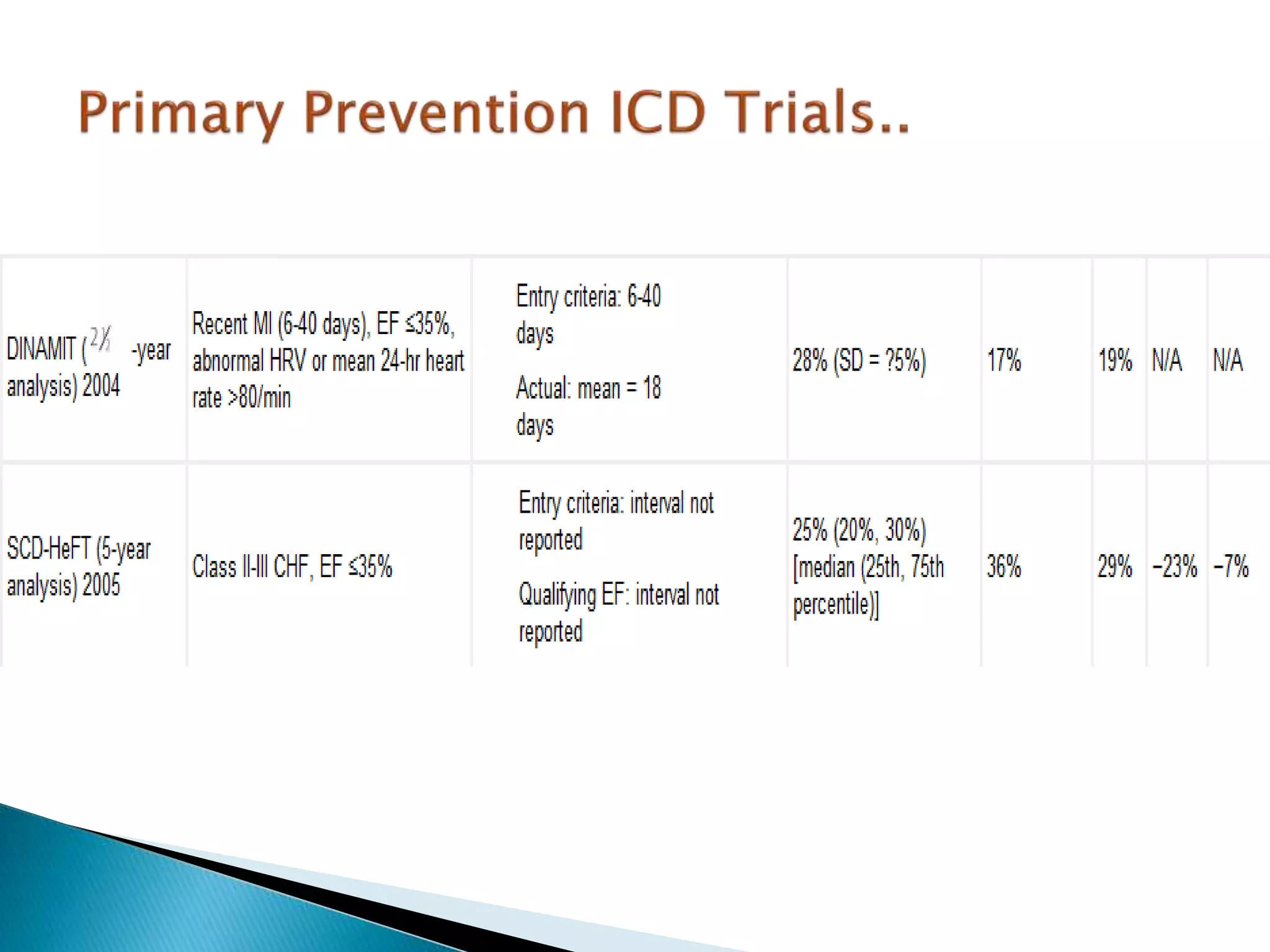
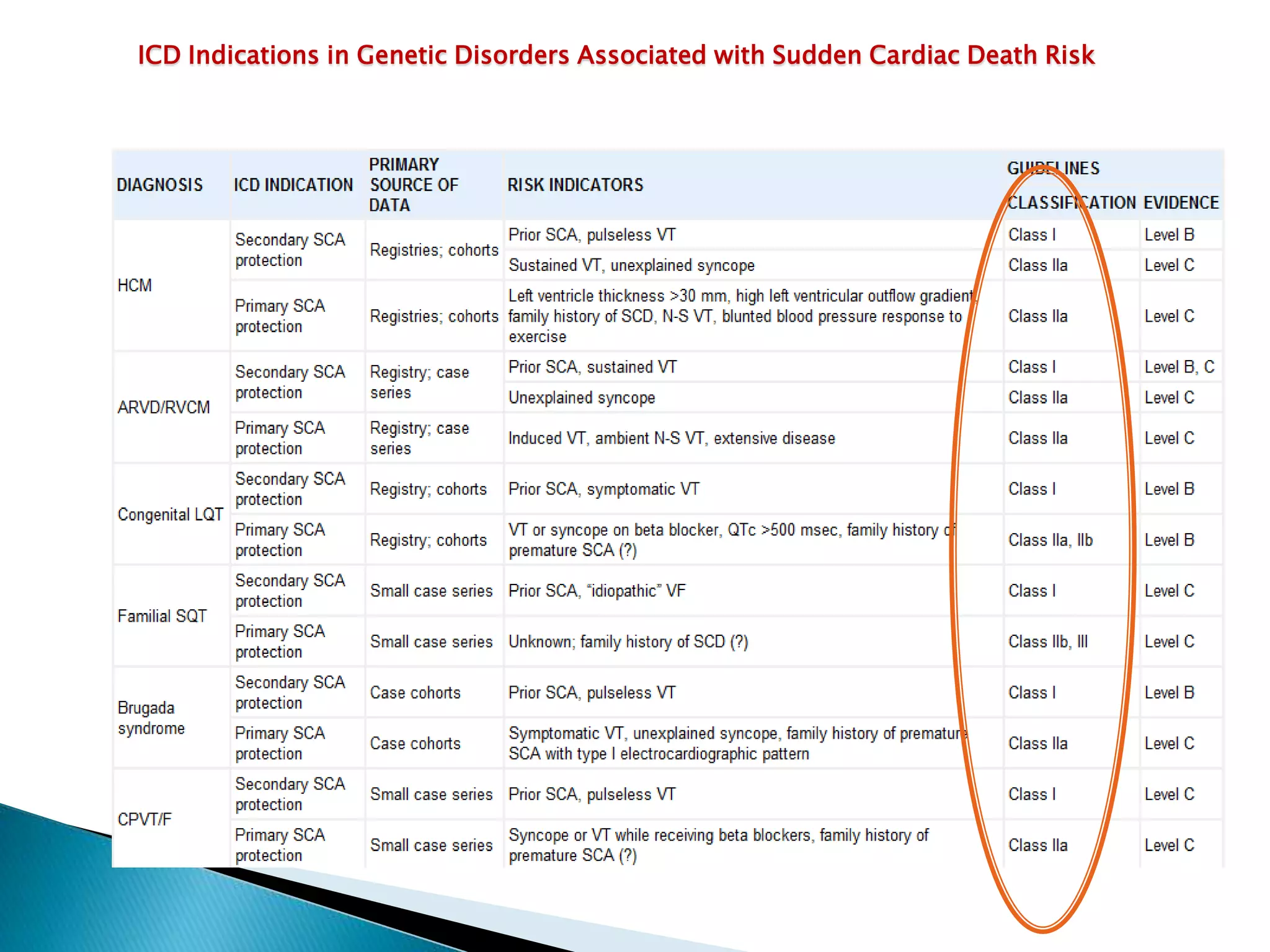
- Causes include ventricular arrhythmias, asystole, and pulseless electrical activity. Prevention strategies include implantable defibrillators, antiarrhythmic drugs