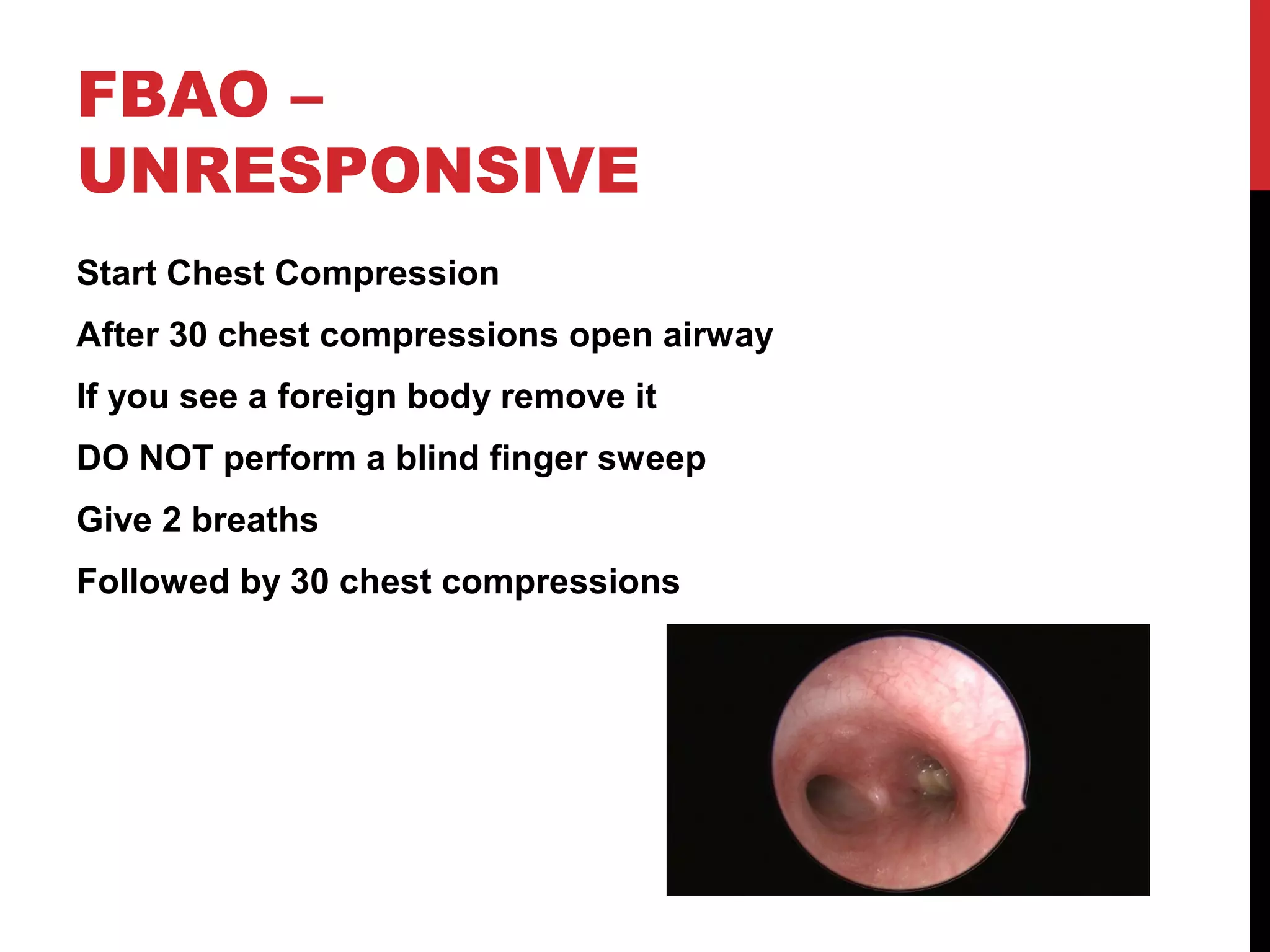
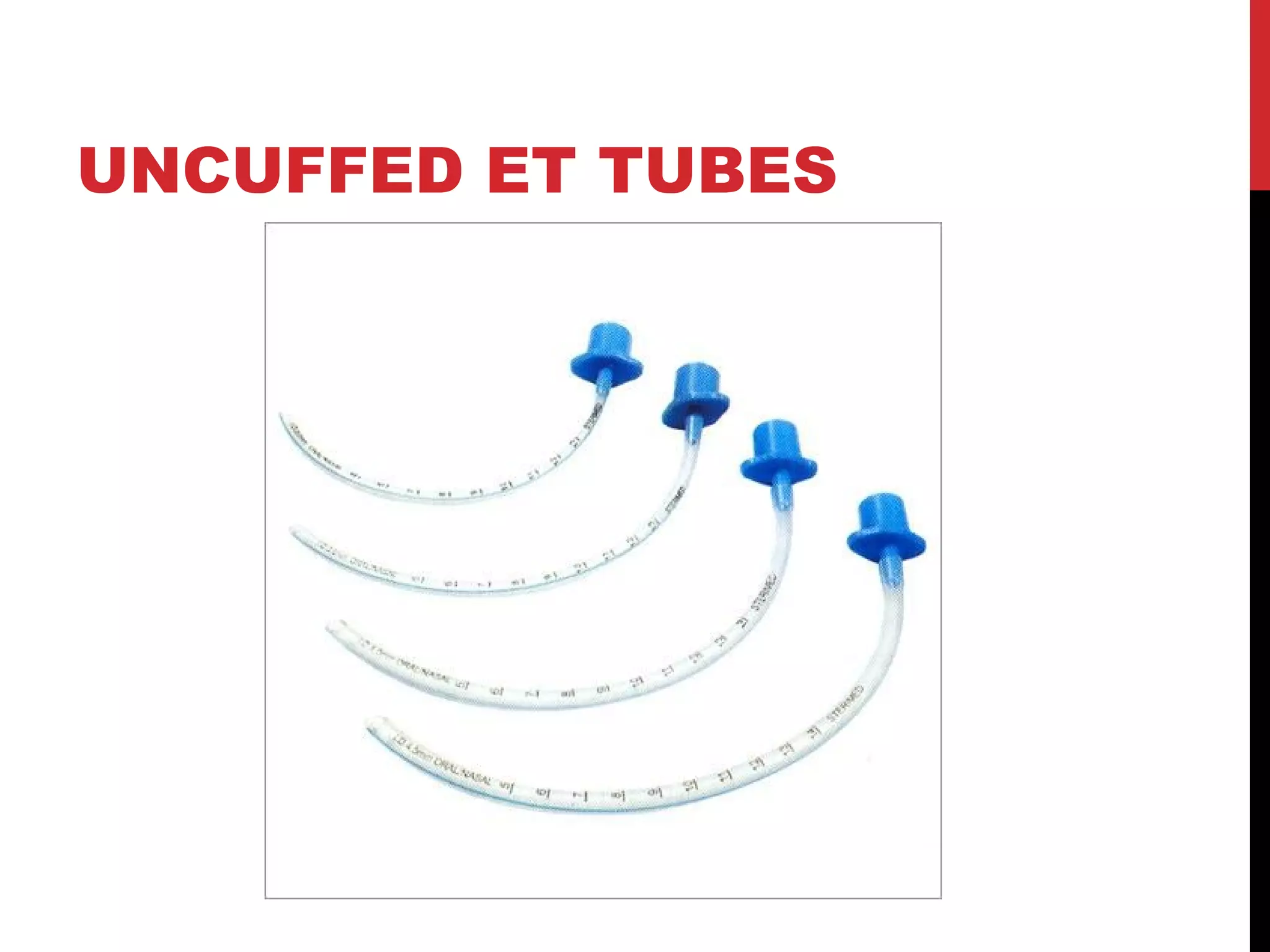
This document provides guidance on pediatric advanced life support (PALS). It discusses respiratory and circulatory failure, which often lead to cardiac arrest in children. Asphyxial cardiac arrest caused by lack of oxygen is more common than primary cardiac issues. Shock is also a common precursor and progresses from compensated to decompensated states. Foreign body airway obstruction, drowning, and hypothermia/hyperthermia are covered. The document provides detailed guidance on airway management, ventilation, vascular access, defibrillation, and the management of arrhythmias like tachycardia and bradycardia in a pediatric setting.