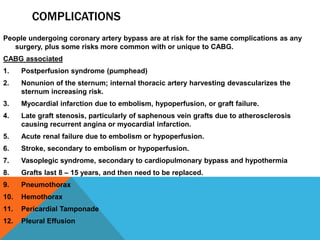
Coronary artery bypass graft (CABG) surgery is performed to relieve symptoms of coronary artery disease such as angina by grafting blood vessels around blockages in the coronary arteries. The document outlines the indications for CABG, including disease involving multiple vessels or the main left coronary artery. It then describes the procedure, which involves harvesting vessels such as the internal mammary artery to graft around blockages, as well as post-operative precautions to avoid straining the sternum. Complications can include issues related to bypass such as reduced kidney function or stroke, as well as general risks of surgery like infection.