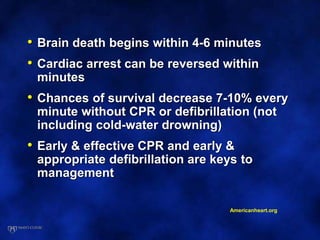
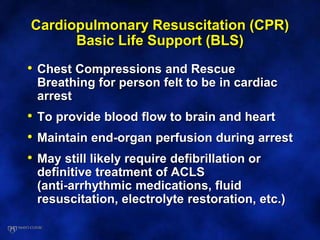
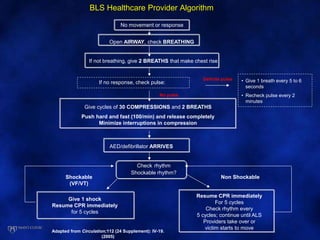
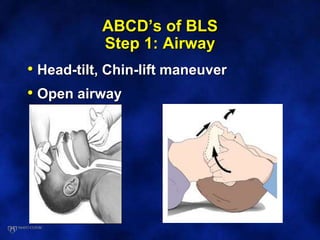
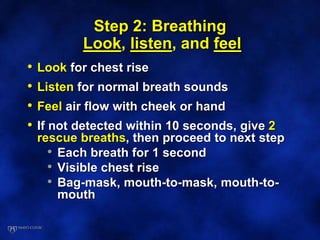
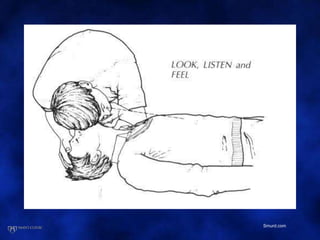
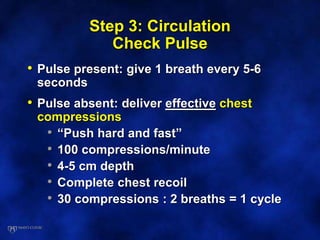
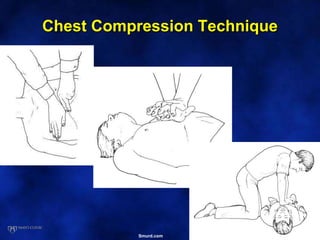
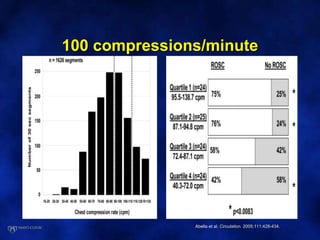
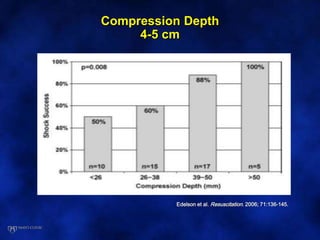
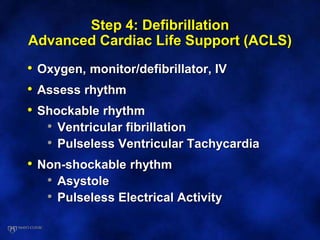
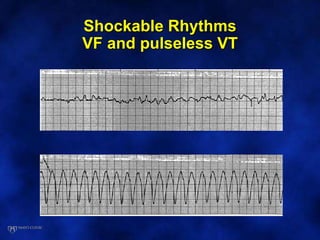
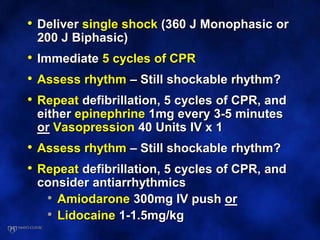
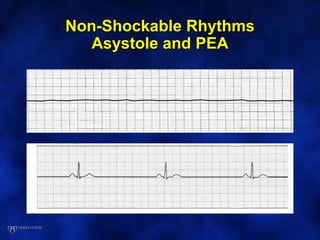
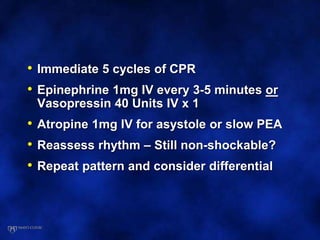
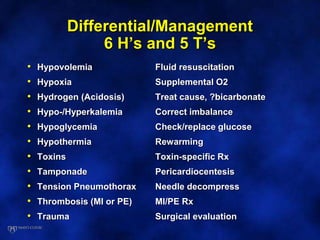
This document discusses cardiopulmonary resuscitation (CPR) and basic life support (BLS) for cardiac arrest. It outlines the key steps of BLS which are the ABCs - airway, breathing, and circulation. Chest compressions and rescue breathing are used to provide blood flow and oxygen to the heart and brain. For cardiac arrest due to shockable rhythms like ventricular fibrillation, defibrillation is needed along with CPR. Advanced cardiac life support (ACLS) protocols are described for shockable and non-shockable rhythms. The document emphasizes that early CPR and defibrillation are critical to survival from cardiac arrest.