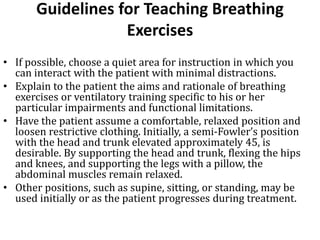
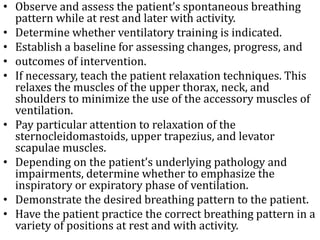
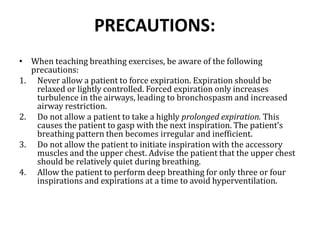
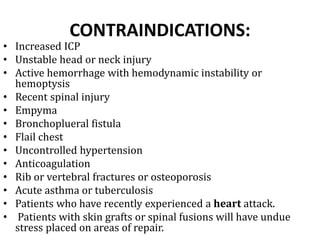
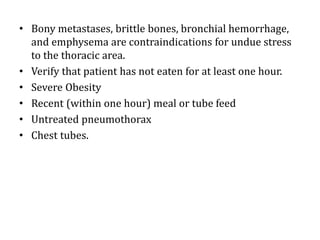
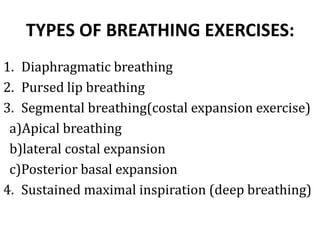
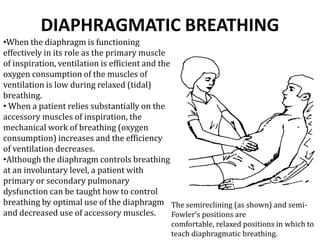
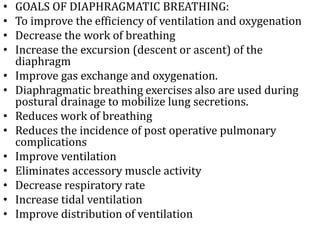
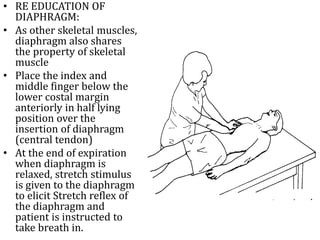
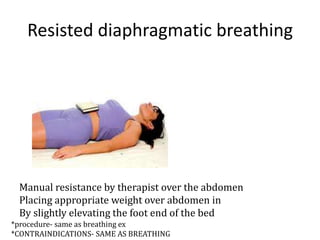
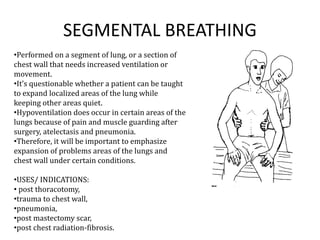
Breathing exercises, also called ventilatory training, are interventions used to improve pulmonary function and endurance. They work to retrain respiratory muscles, improve ventilation, lessen the work of breathing, and enhance gas exchange. Common breathing exercises include diaphragmatic breathing and pursed lip breathing. Diaphragmatic breathing focuses on using the diaphragm as the primary breathing muscle to make breathing more efficient. Precautions are taken to avoid forced exhalation or overbreathing and contraindications exist for certain conditions.