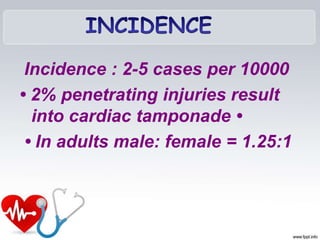
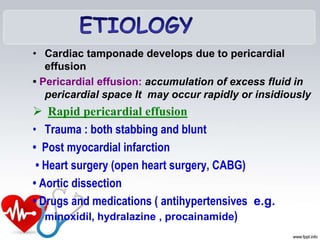
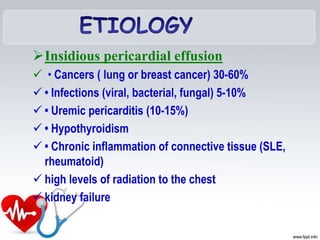
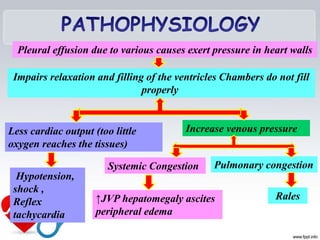
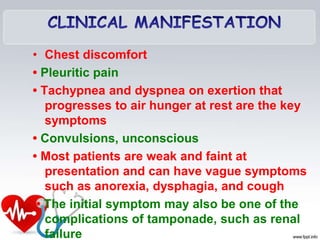
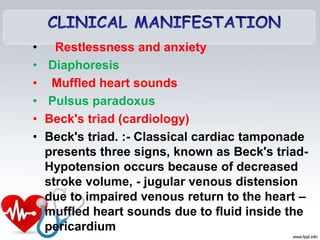
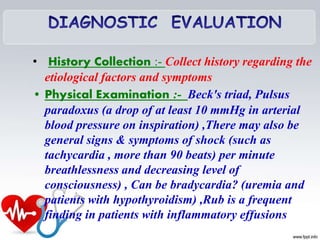
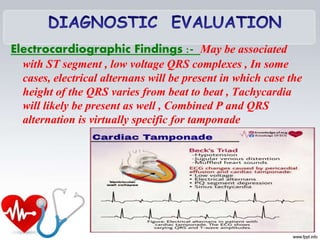
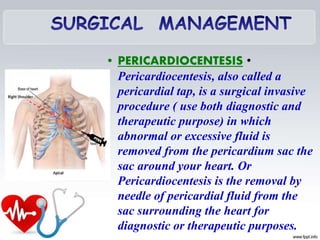
Cardiac tamponade is a serious medical condition caused by fluid accumulating in the pericardial sac surrounding the heart, putting pressure on the heart and preventing it from filling properly. Symptoms include chest pain, difficulty breathing, and low blood pressure. Diagnosis involves echocardiogram, electrocardiogram, chest x-ray or CT scan. Treatment is pericardiocentesis to drain the fluid via needle, with careful monitoring of vital signs.