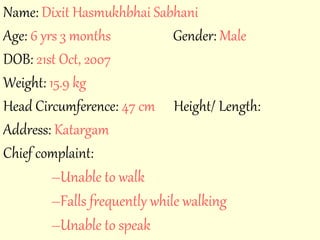
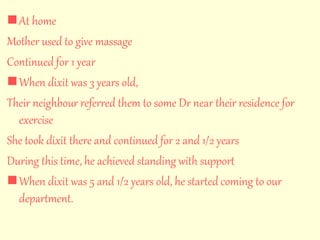
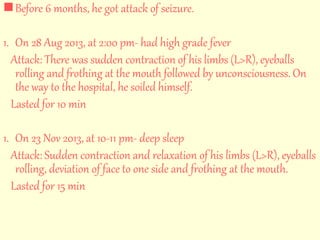
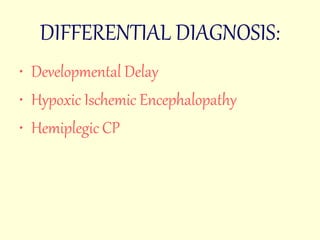
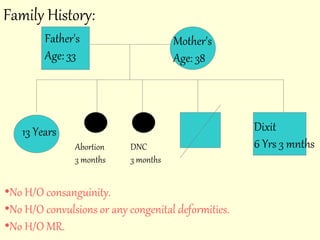
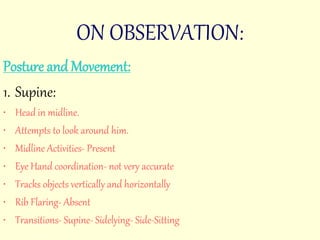
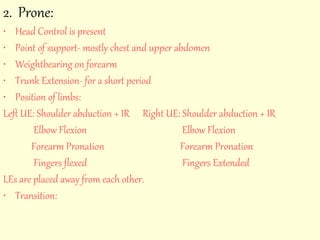
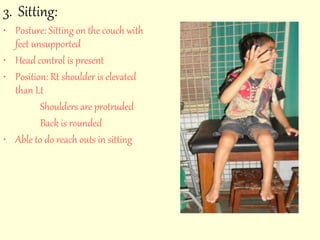
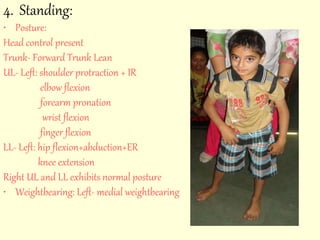
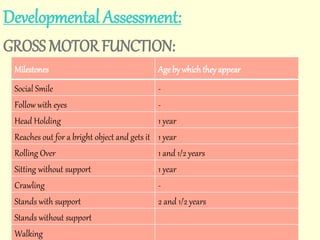
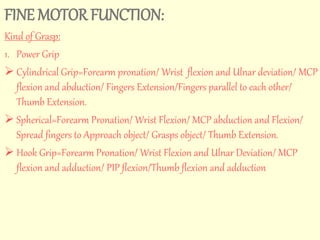
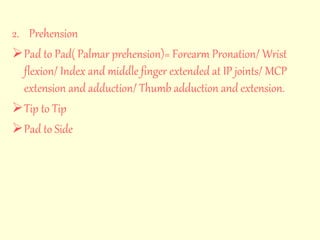
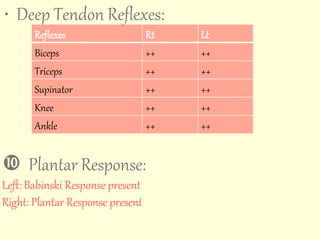
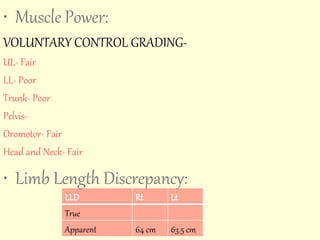
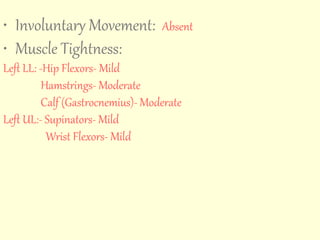
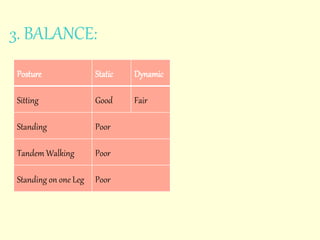
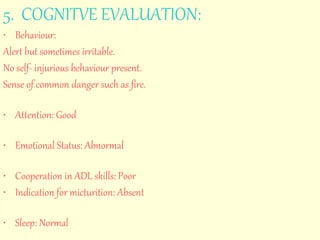
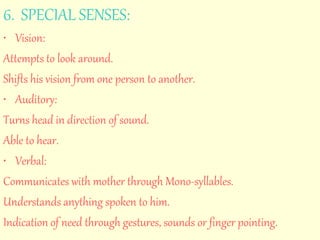
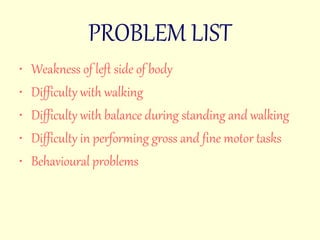
The case presentation involves a 6-year-old boy named Dixit who has developmental delays, difficulty walking, and seizures. His prenatal and birth history indicated complications, including delayed cry and NICU admission. Current assessments reveal muscle weakness, motor skill difficulties, and a plan for treatment focused on muscle re-education and improvement of functional skills.