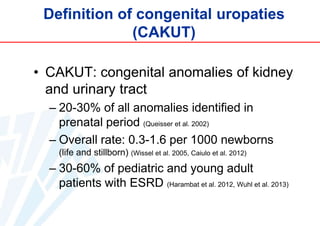
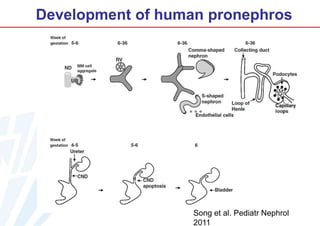
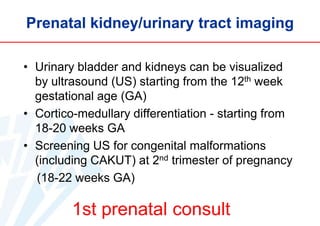
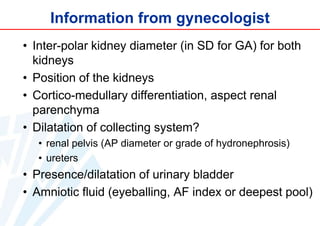
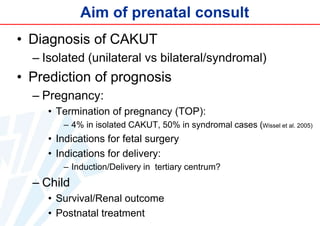
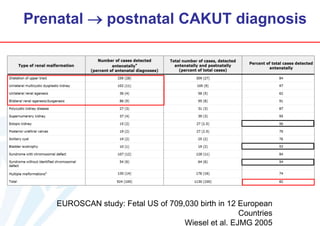
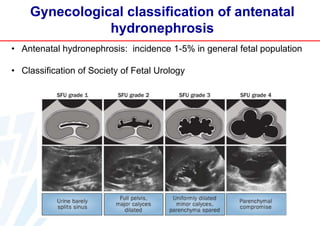
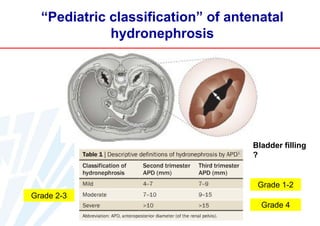
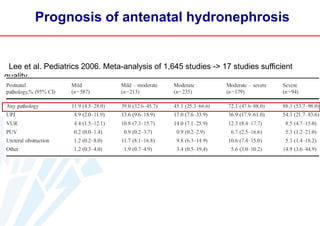
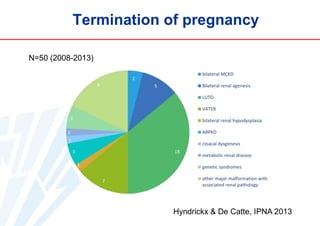
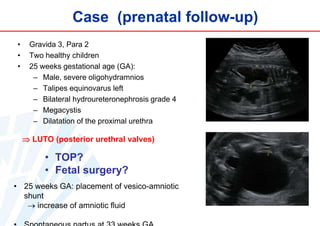
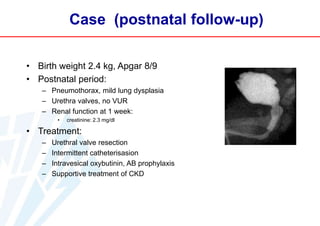
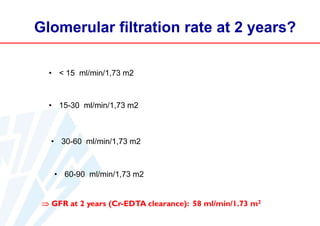
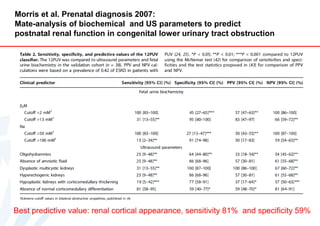
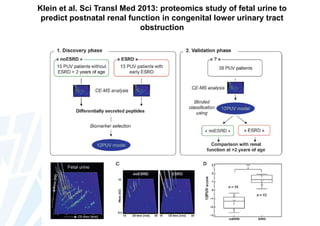
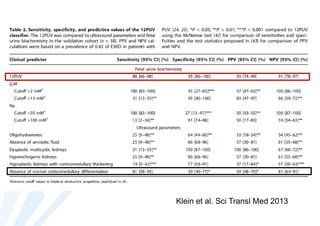
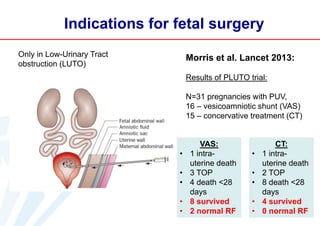
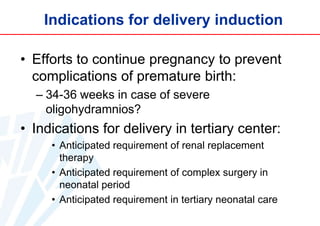
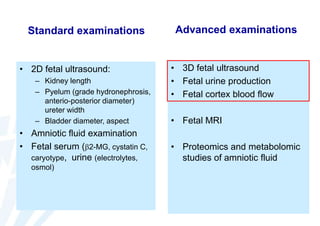
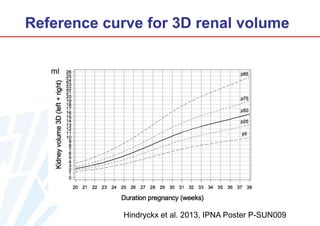
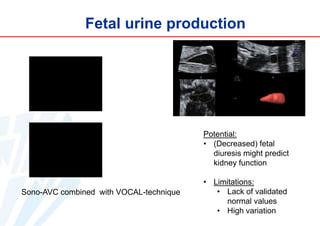
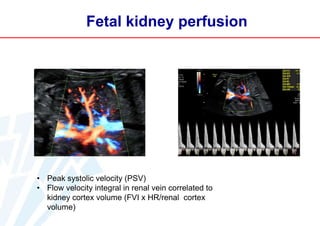
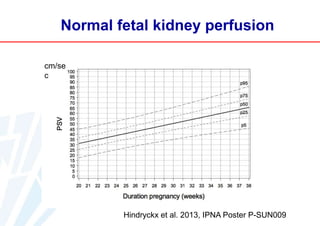
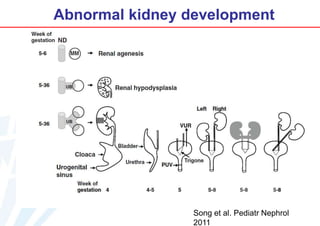
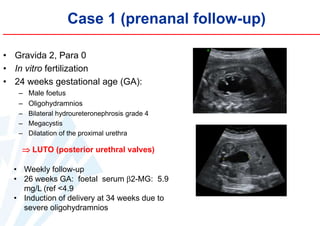
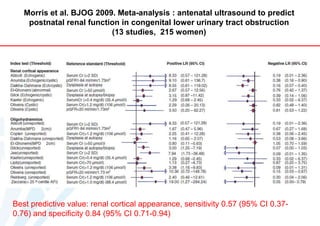
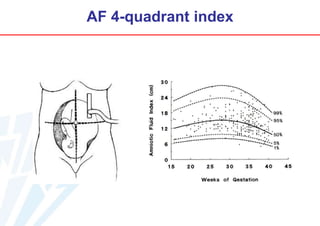
The document discusses prenatal diagnosis of congenital uropathies. It defines congenital anomalies of the kidney and urinary tract (CAKUT) and notes they can be identified prenatally in ultrasound scans starting at 12 weeks gestation. The goal of prenatal consultation is to diagnose CAKUT, predict prognosis for pregnancy and child, and determine indications for termination of pregnancy, fetal surgery, or delivery. Standard prenatal exams can provide useful information but have limitations in predicting postnatal renal outcome, and advanced imaging techniques are being studied to improve prognosis.