1. Anorectal malformations are congenital anomalies of the anus and rectum that occur in approximately 1 in 5,000 live births.
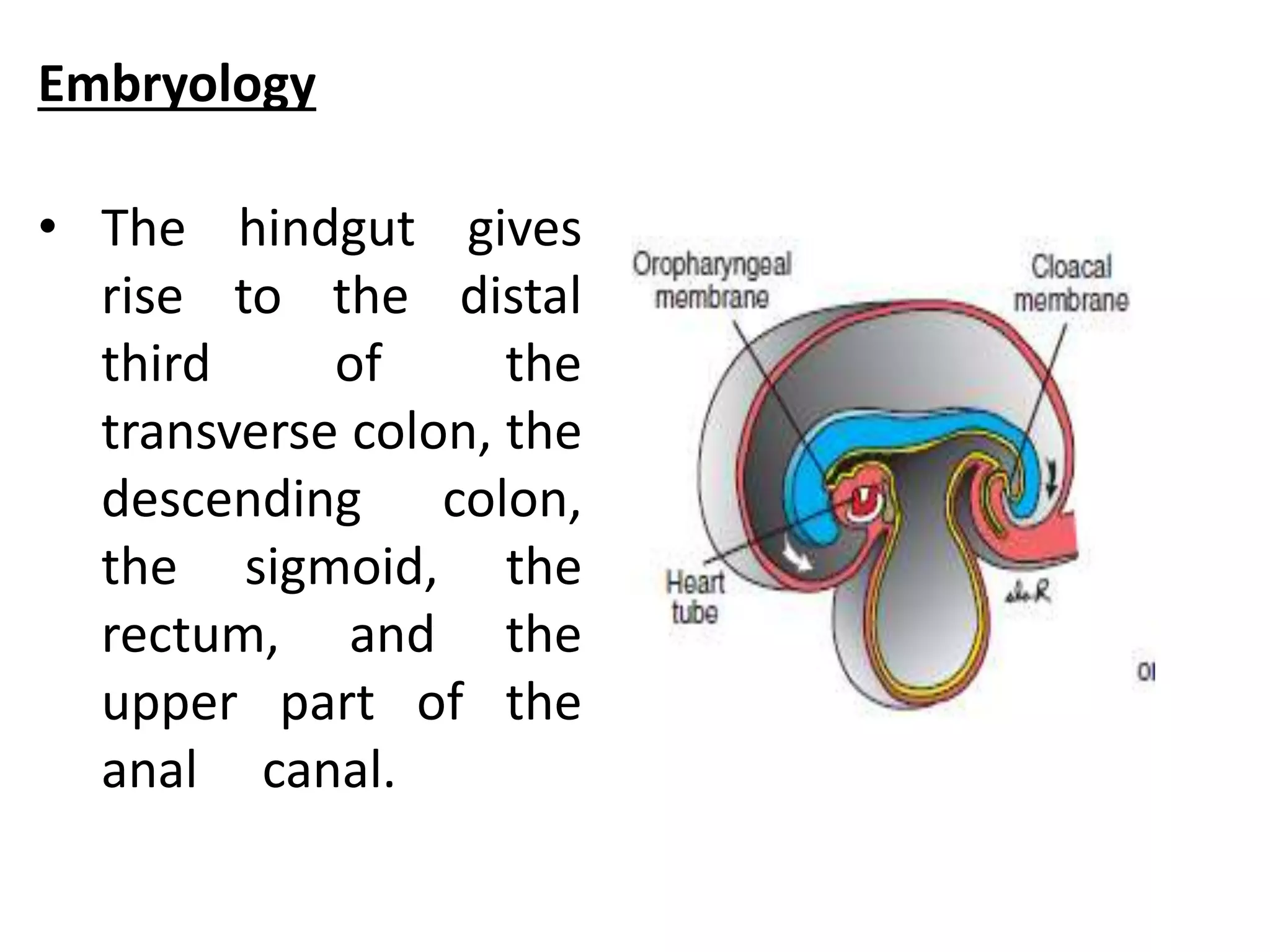
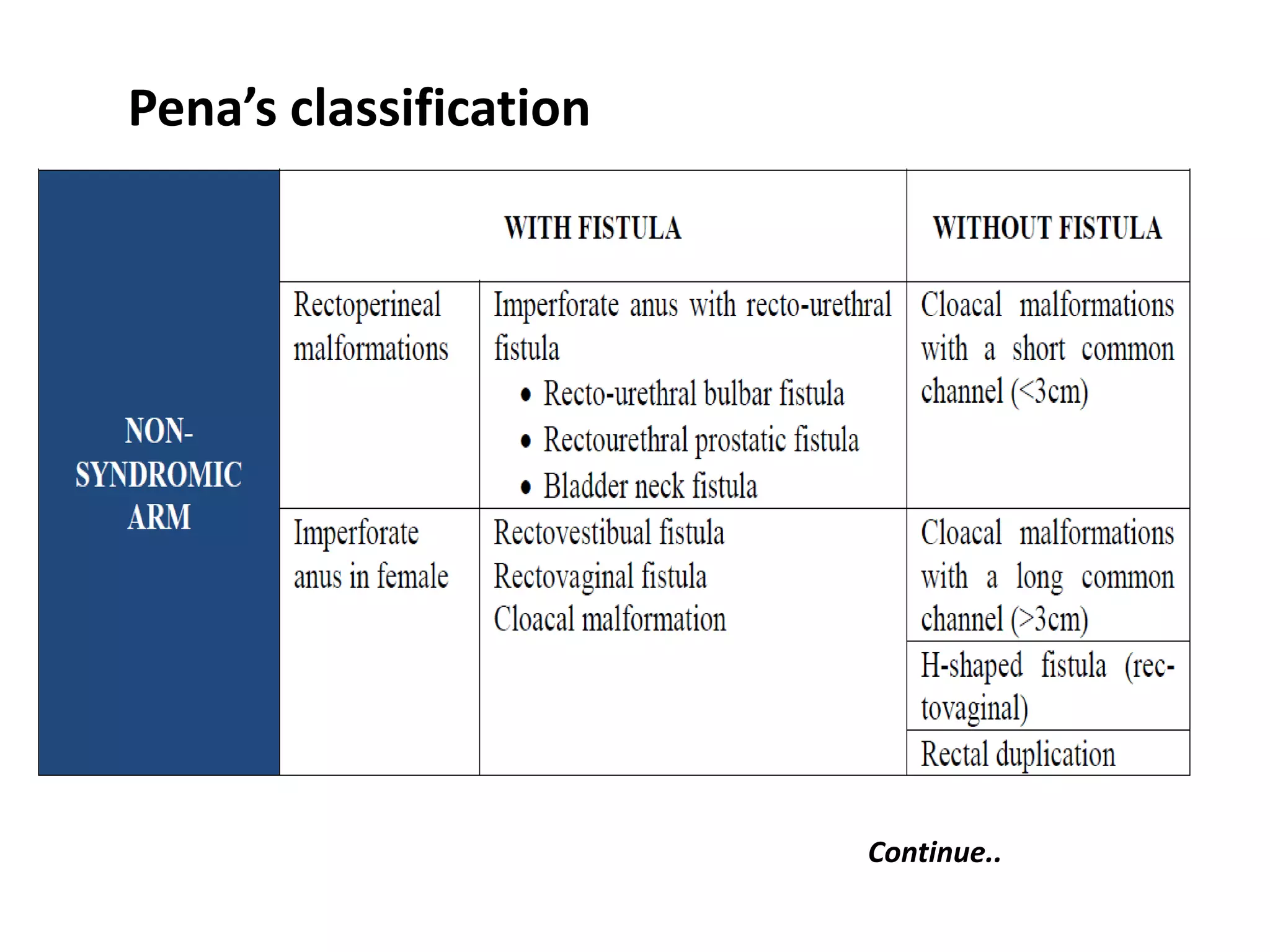
2. The document describes various classifications of anorectal malformations and discusses the embryological development of the condition.
3. Key surgical procedures for repair of anorectal malformations are described, including colostomy, posterior sagittal anorectoplasty, and pull-through operations. The repair approaches are discussed depending on the specific type of malformation.