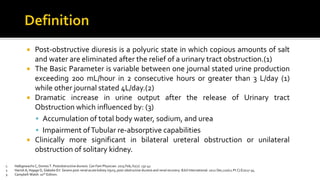
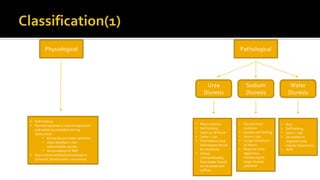
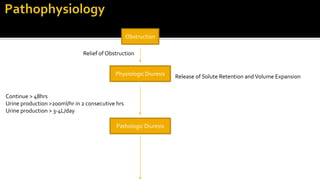
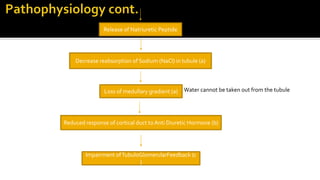
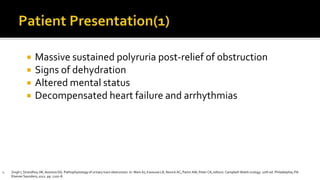
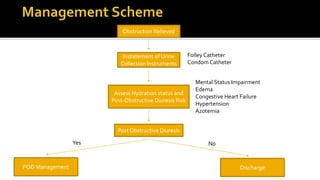
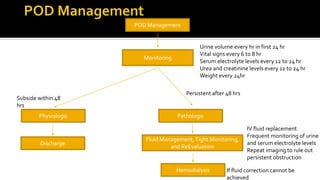
Post-obstructive diuresis is defined as a large urine output of over 200mL/hour for 2 consecutive hours or over 3-4L per day that occurs after relief of a urinary tract obstruction. It results from the accumulation of water, sodium, and urea during the obstruction and impaired renal reabsorption capabilities. If not properly managed, it can lead to complications like volume depletion, electrolyte imbalances, and even shock. Treatment involves complete relief of obstruction, fluid replacement, monitoring urine output and electrolyte levels, and managing any complications.