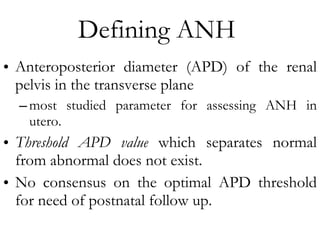
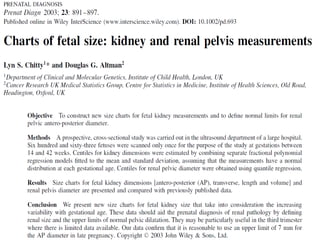
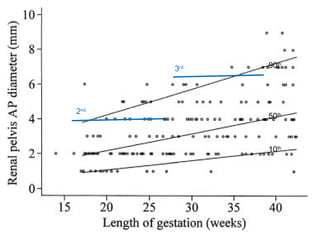
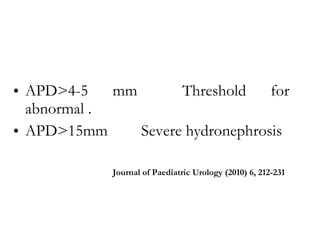
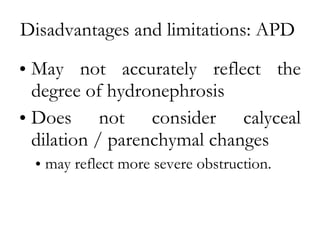
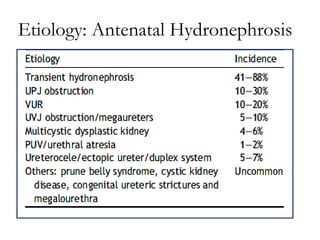
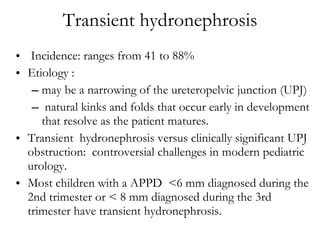
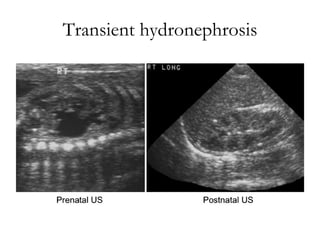
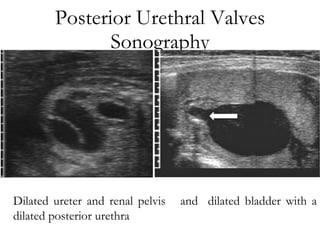
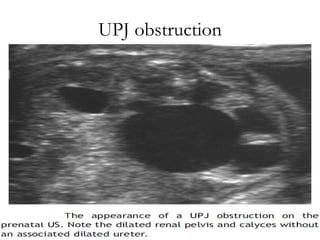
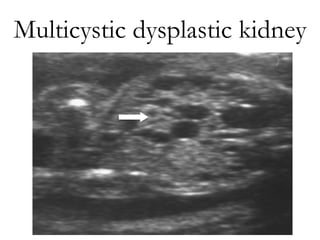
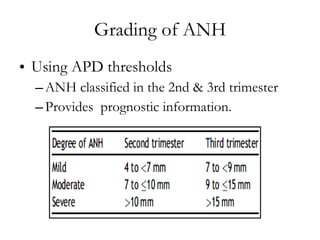
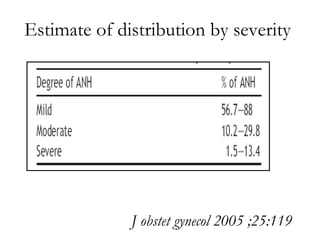
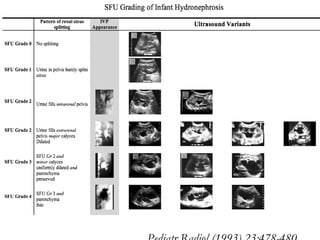
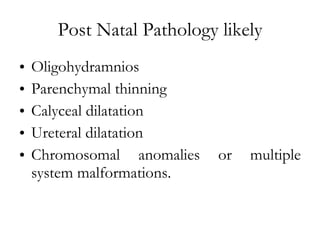
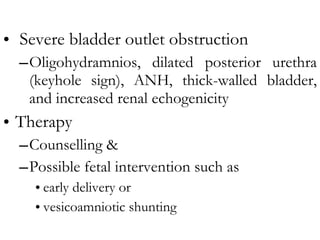
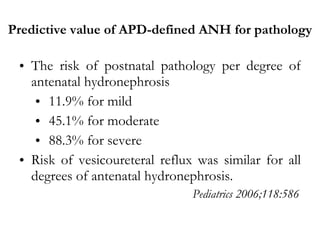
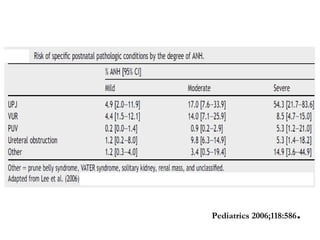
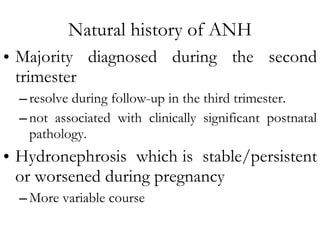
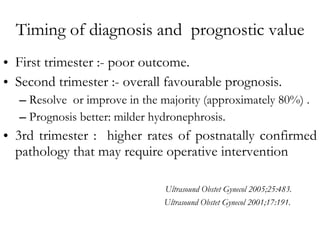
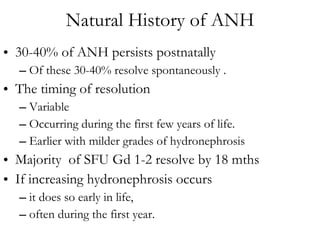
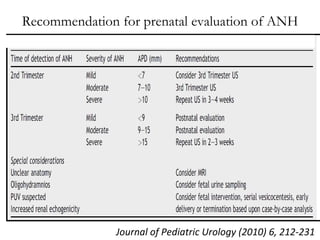
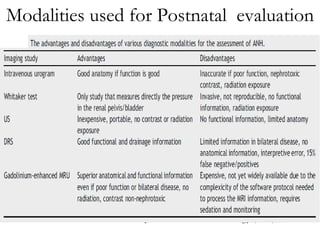
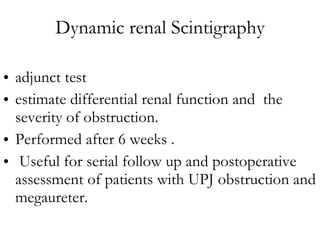
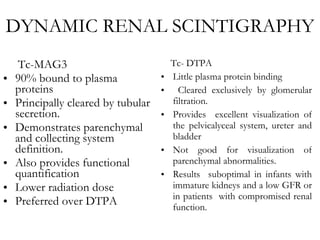
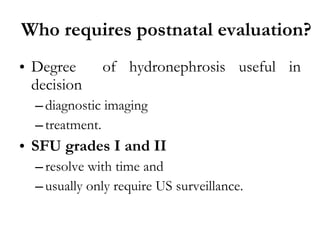
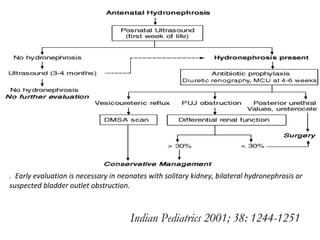
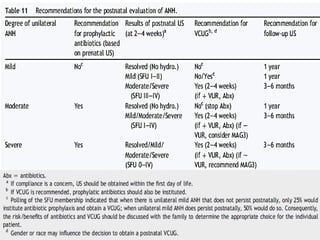
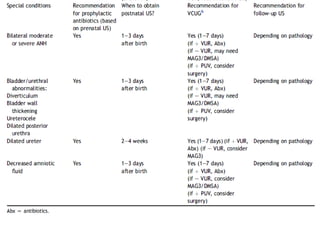
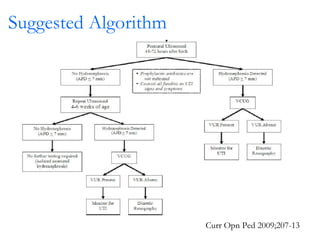
Antenatally detected hydronephrosis is one of the most common abnormalities detected on prenatal ultrasound. It can identify urinary tract obstructions and reflux before complications develop. The degree of hydronephrosis seen on prenatal ultrasound provides prognostic information, with mild cases often resolving and severe cases more likely to require postnatal intervention. Evaluation after birth depends on the severity and laterality of the hydronephrosis seen prenatally, with more severe or bilateral cases warranting earlier and more extensive testing like dynamic renal scintigraphy to assess kidney function and guide management.