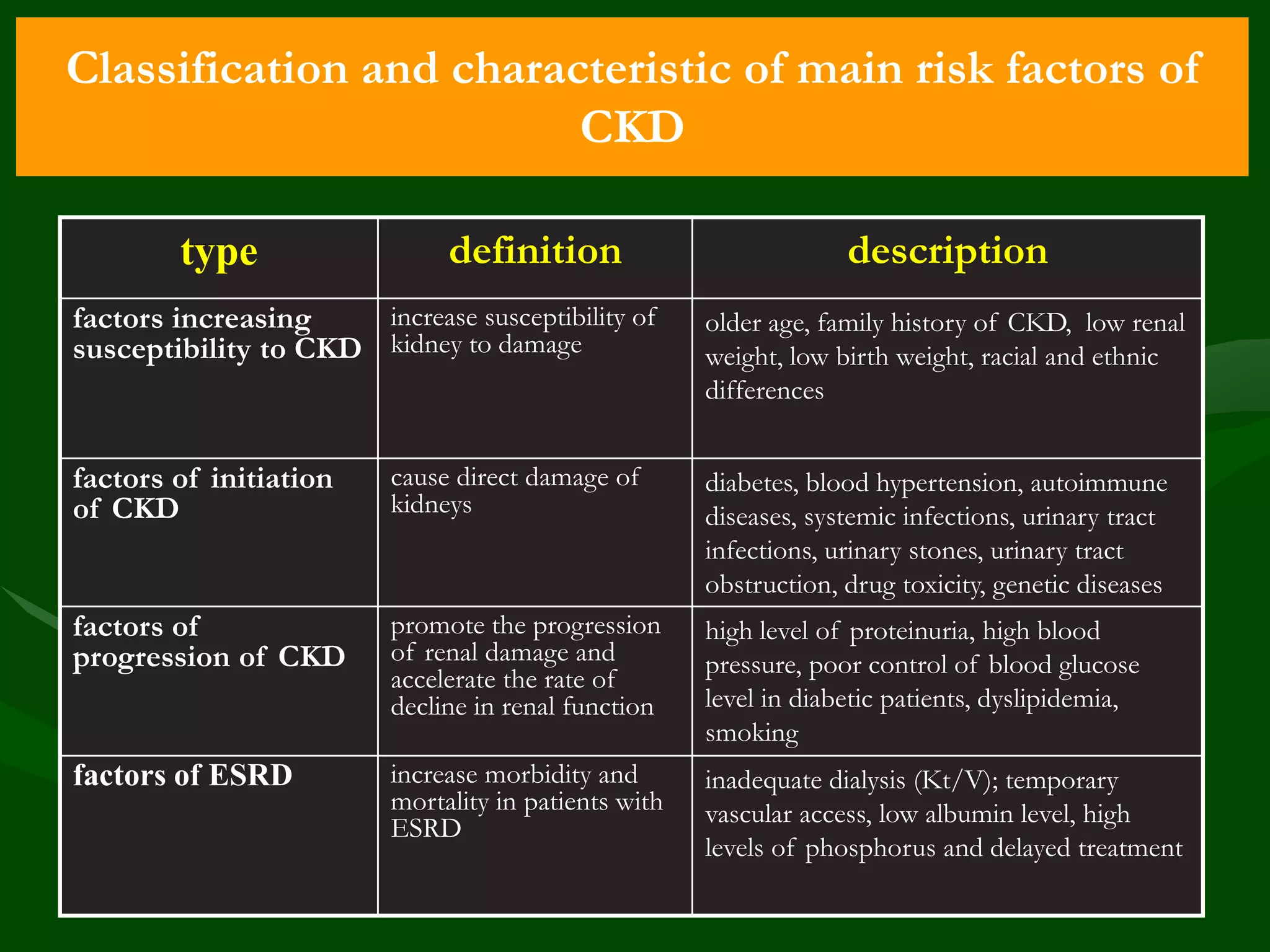
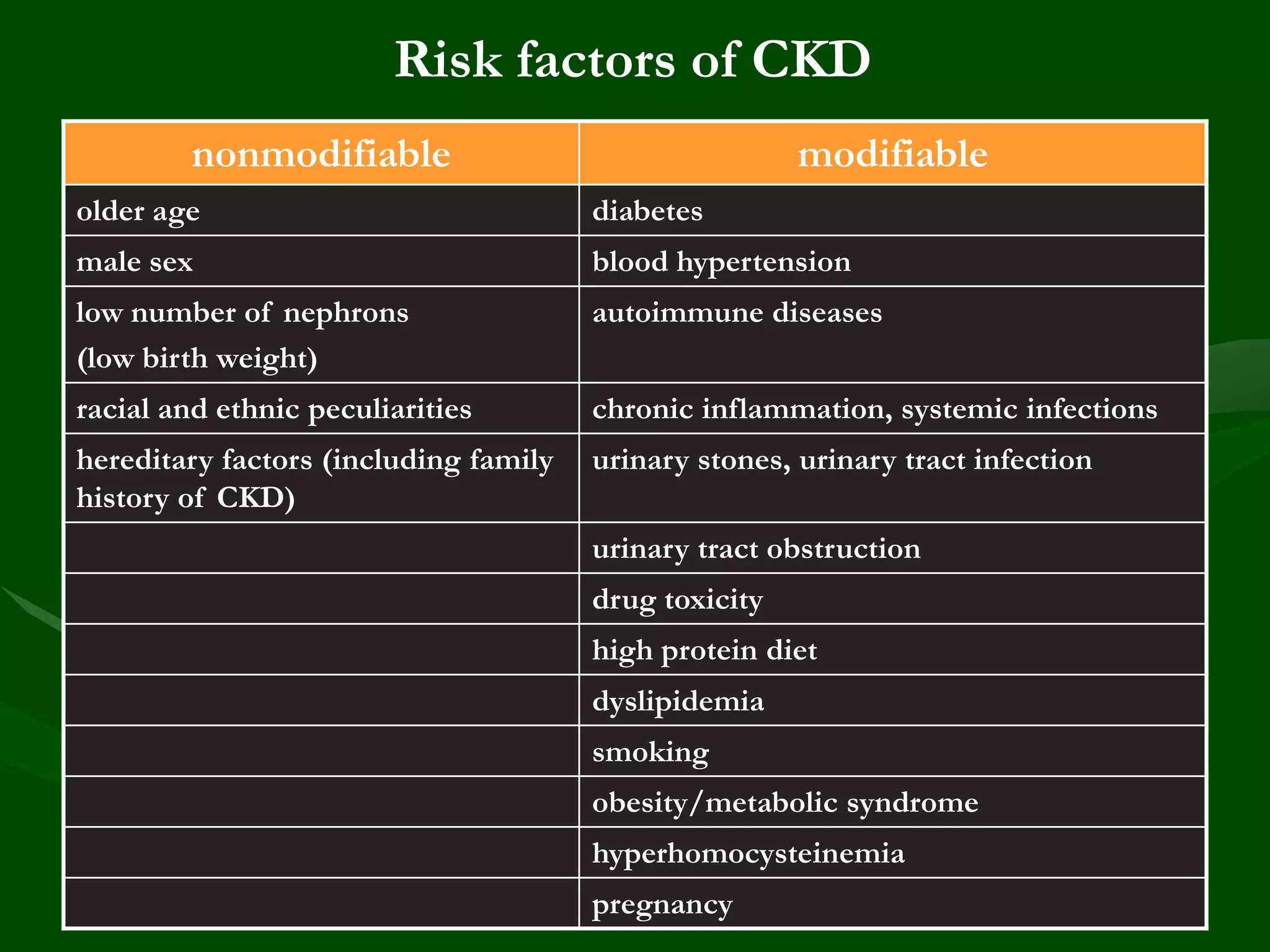
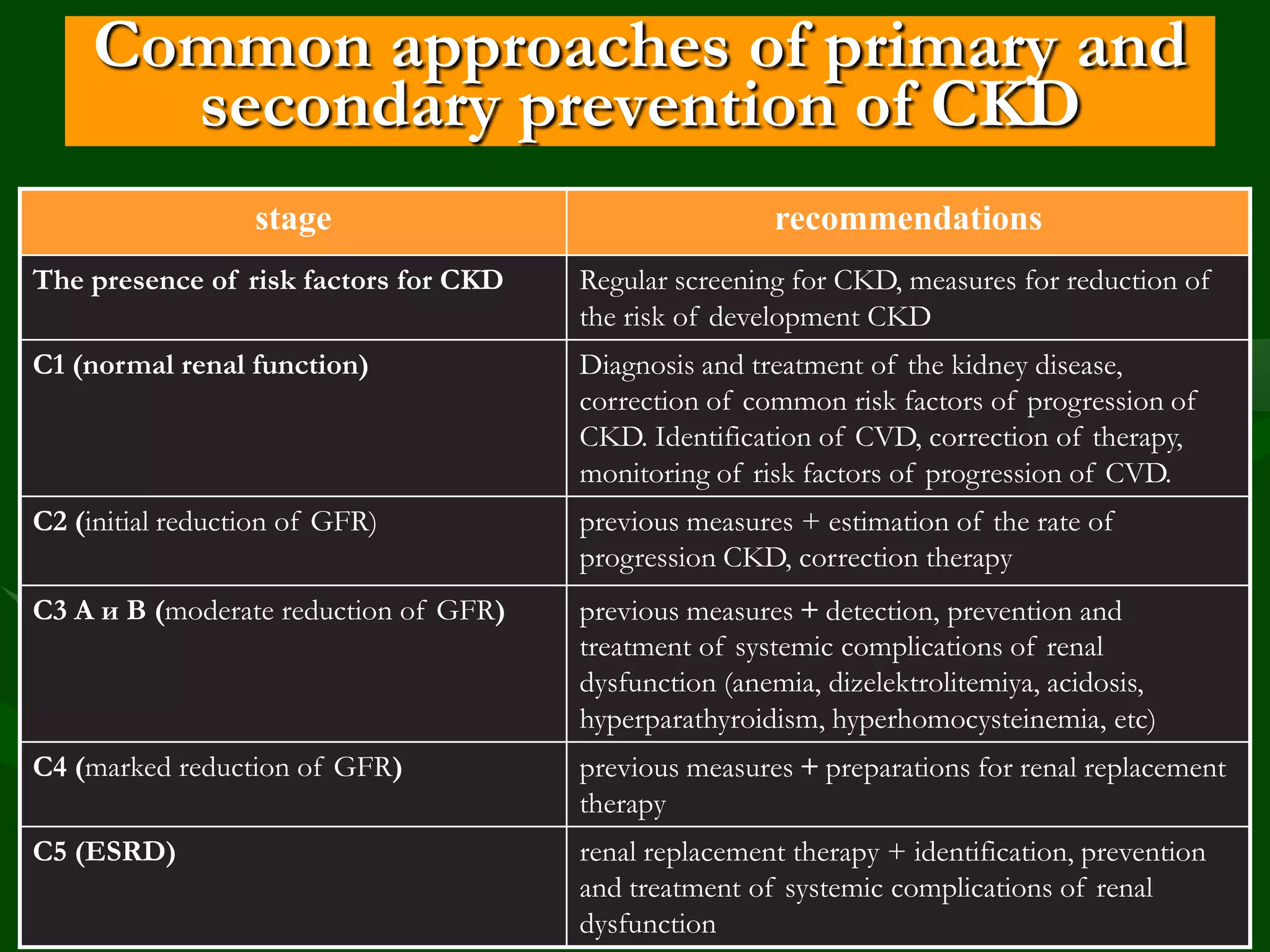
This document discusses chronic kidney disease (CKD), including its history, importance, risk factors, progression, and relationship to cardiovascular disease. Some key points:
- CKD concepts were developed in 2002 to standardize criteria, classification, and terminology. Goals include early detection, slowing progression, and reducing cardiovascular risk.
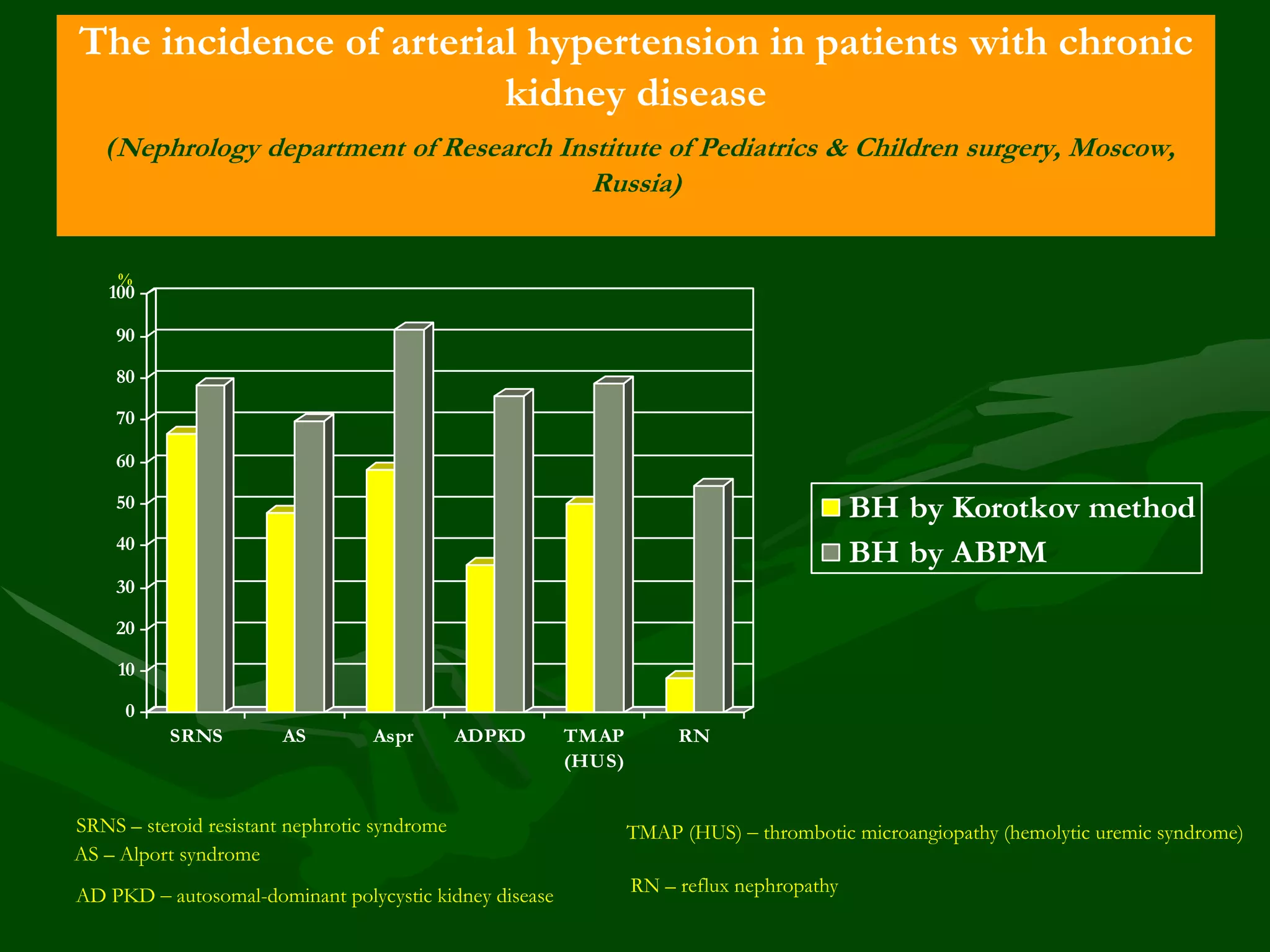
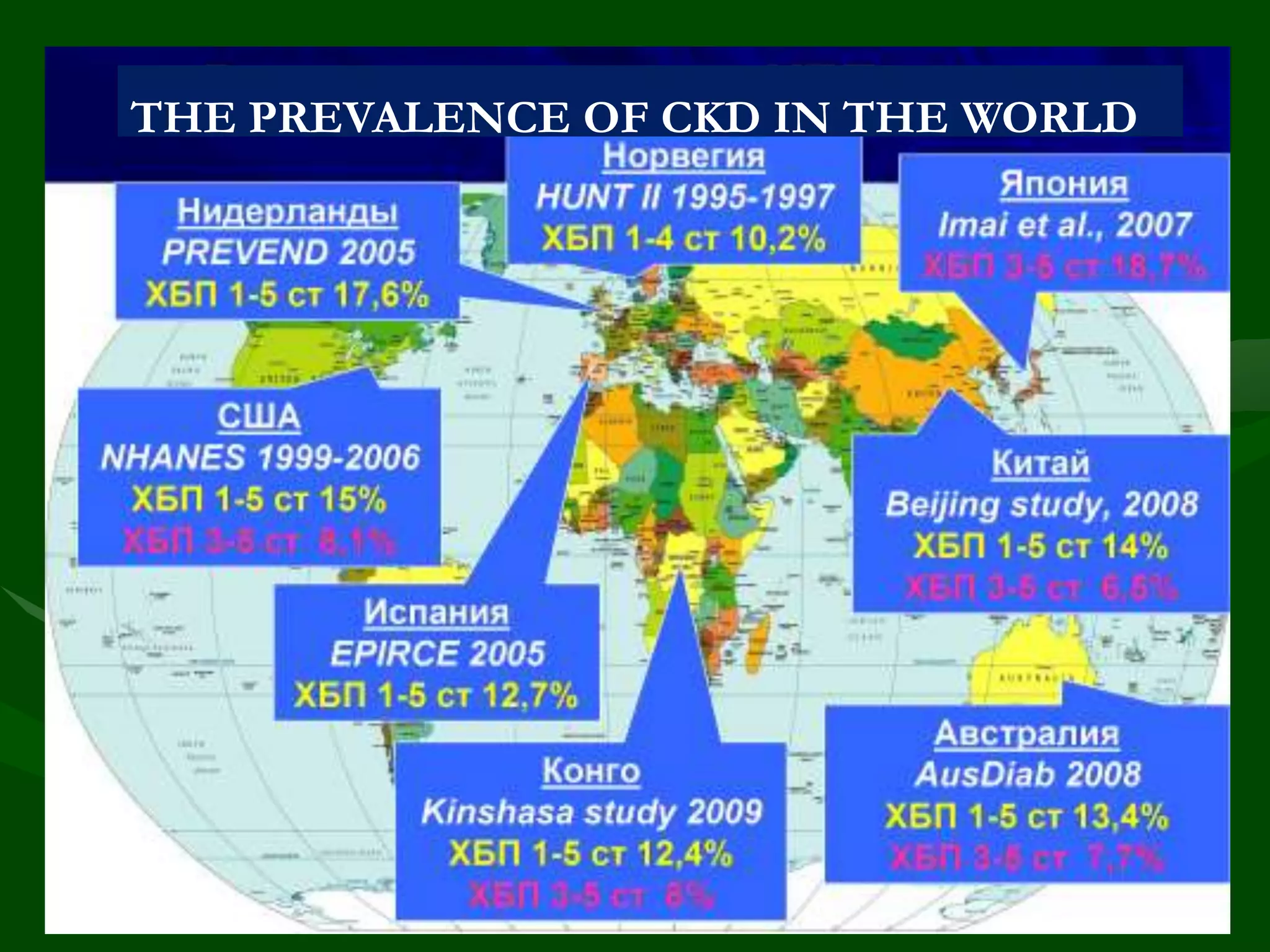
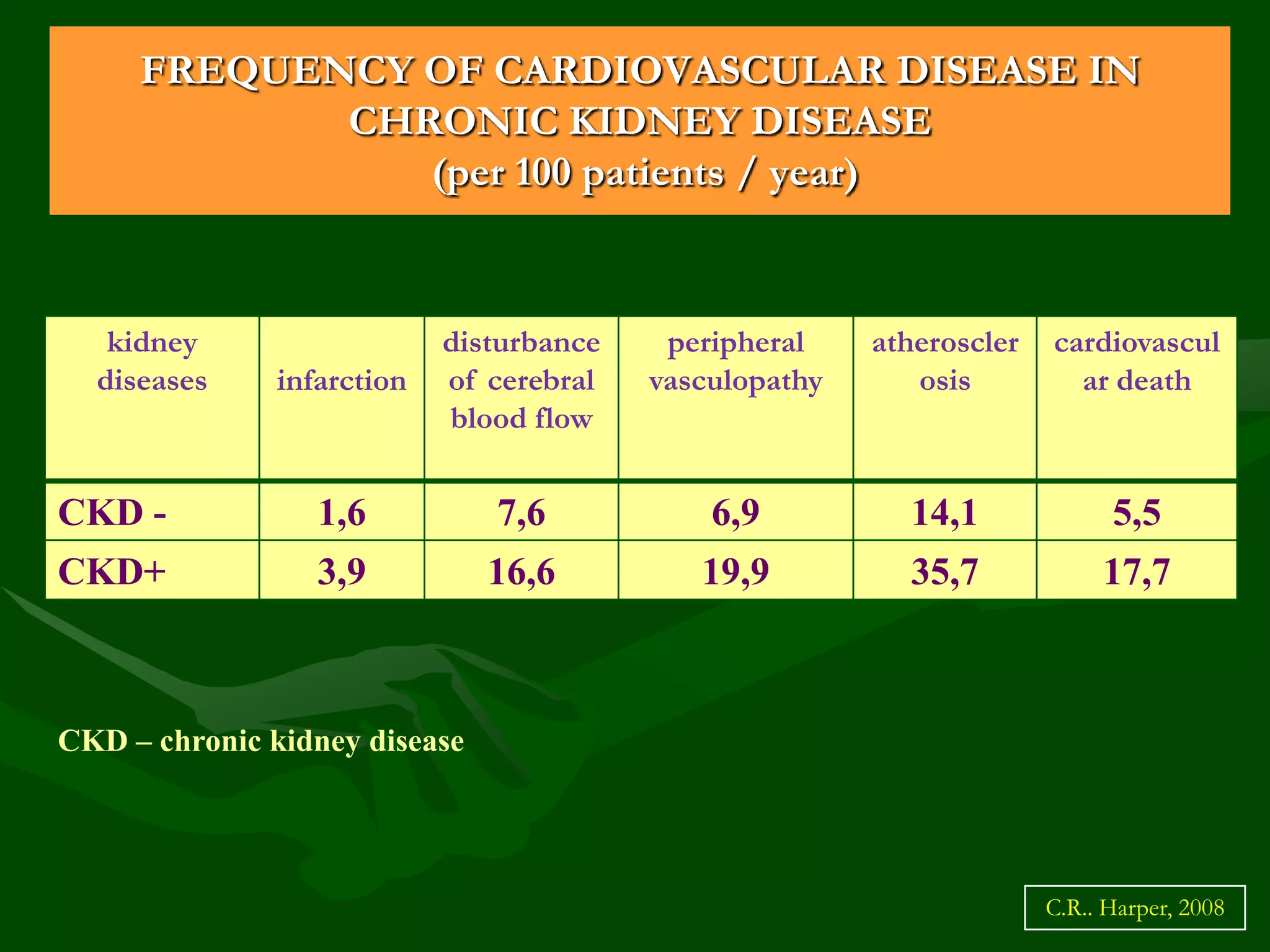
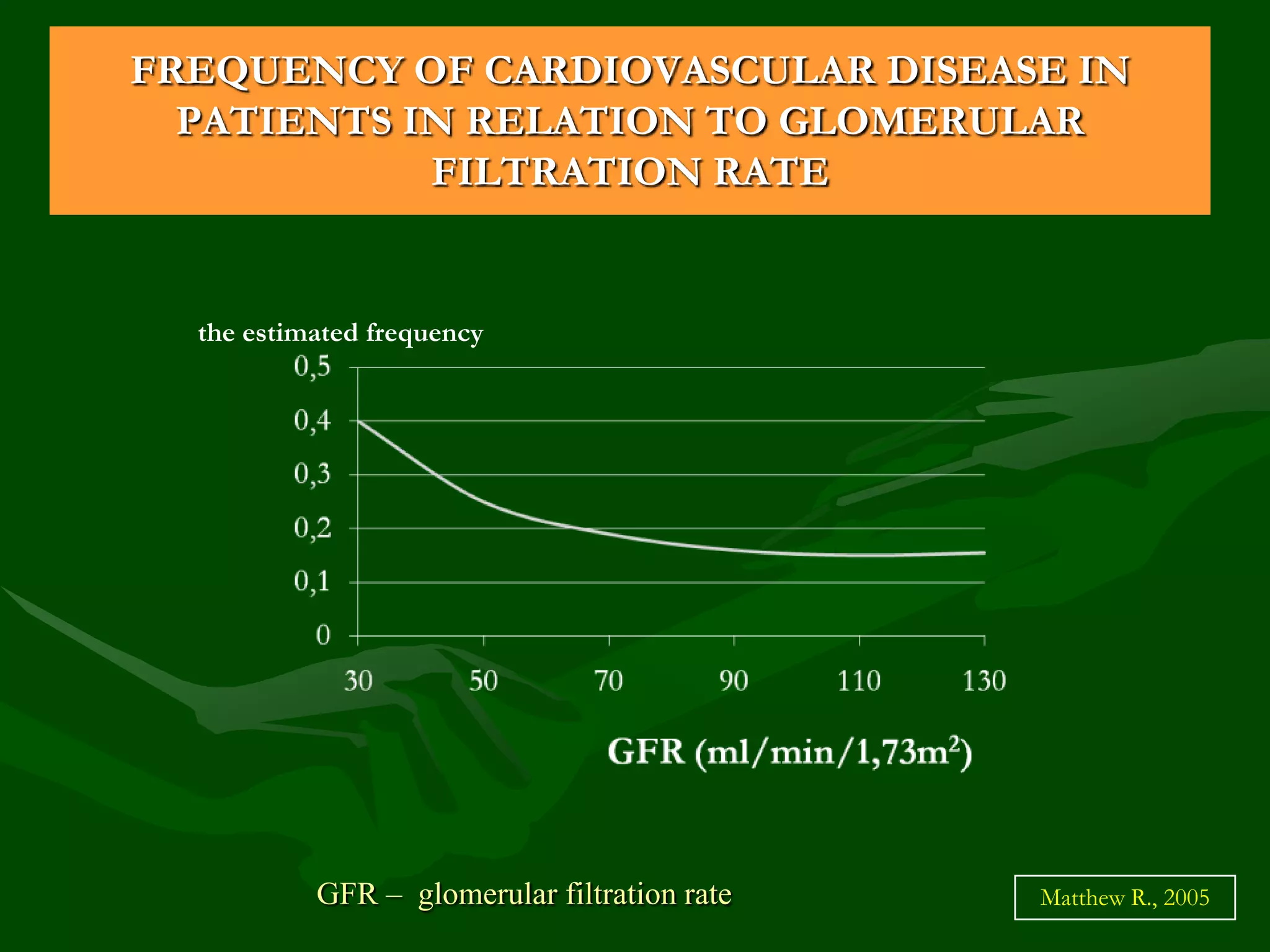
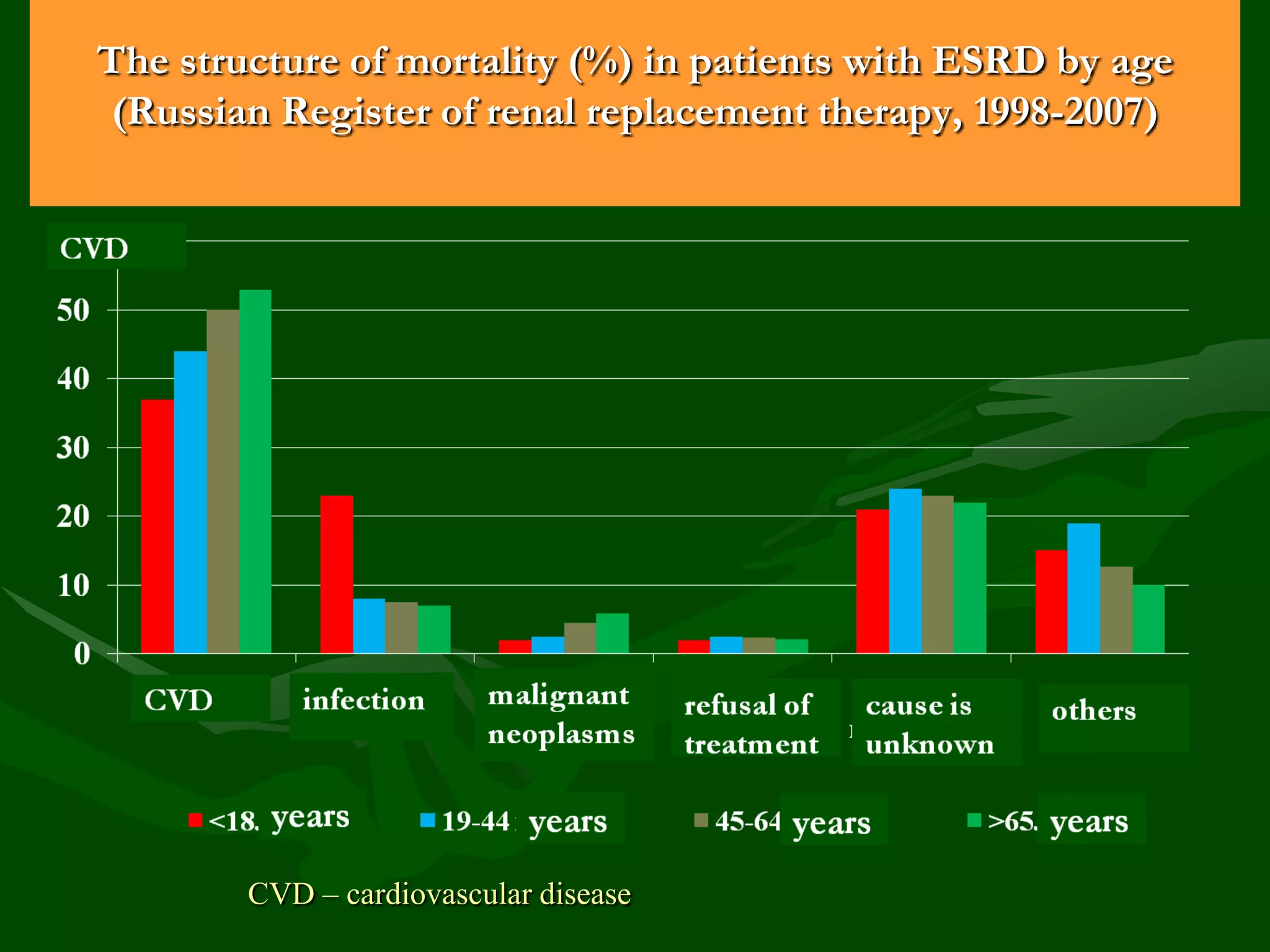
- CKD prevalence is 12-15% for stages 1-5 and 6-8% for stages 3-5. Renal mortality is low but cardiovascular disease is a major cause of death.
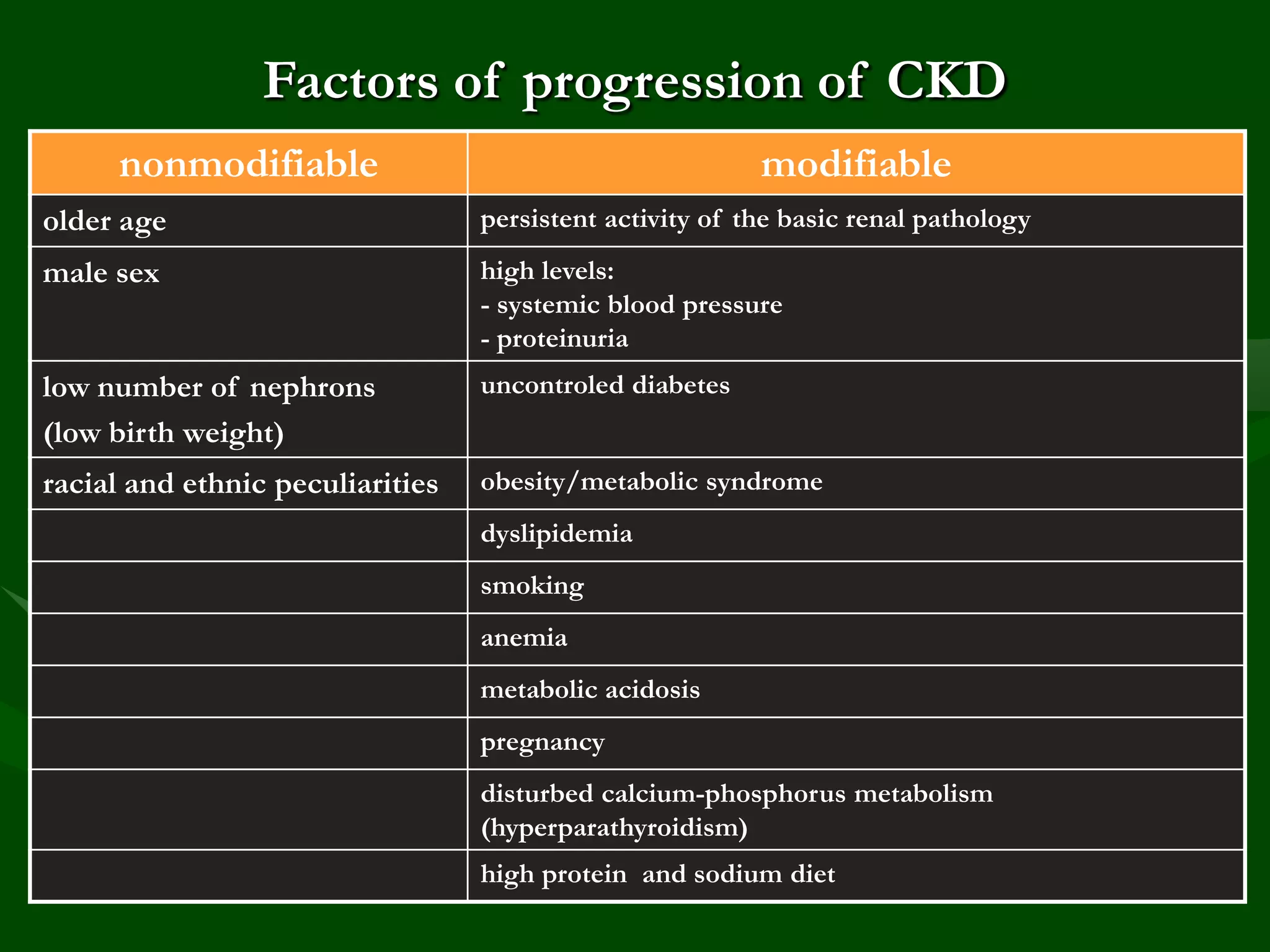
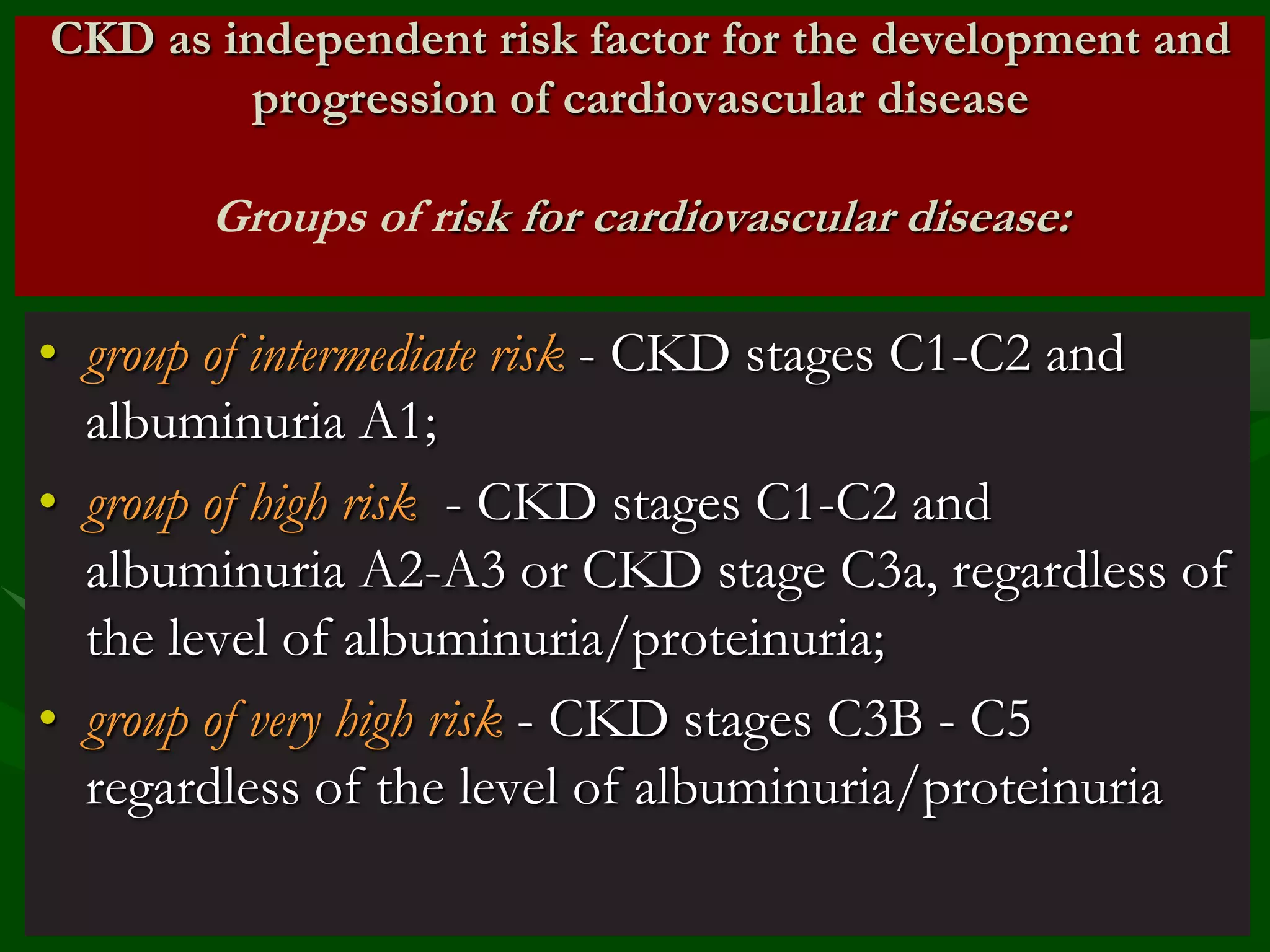
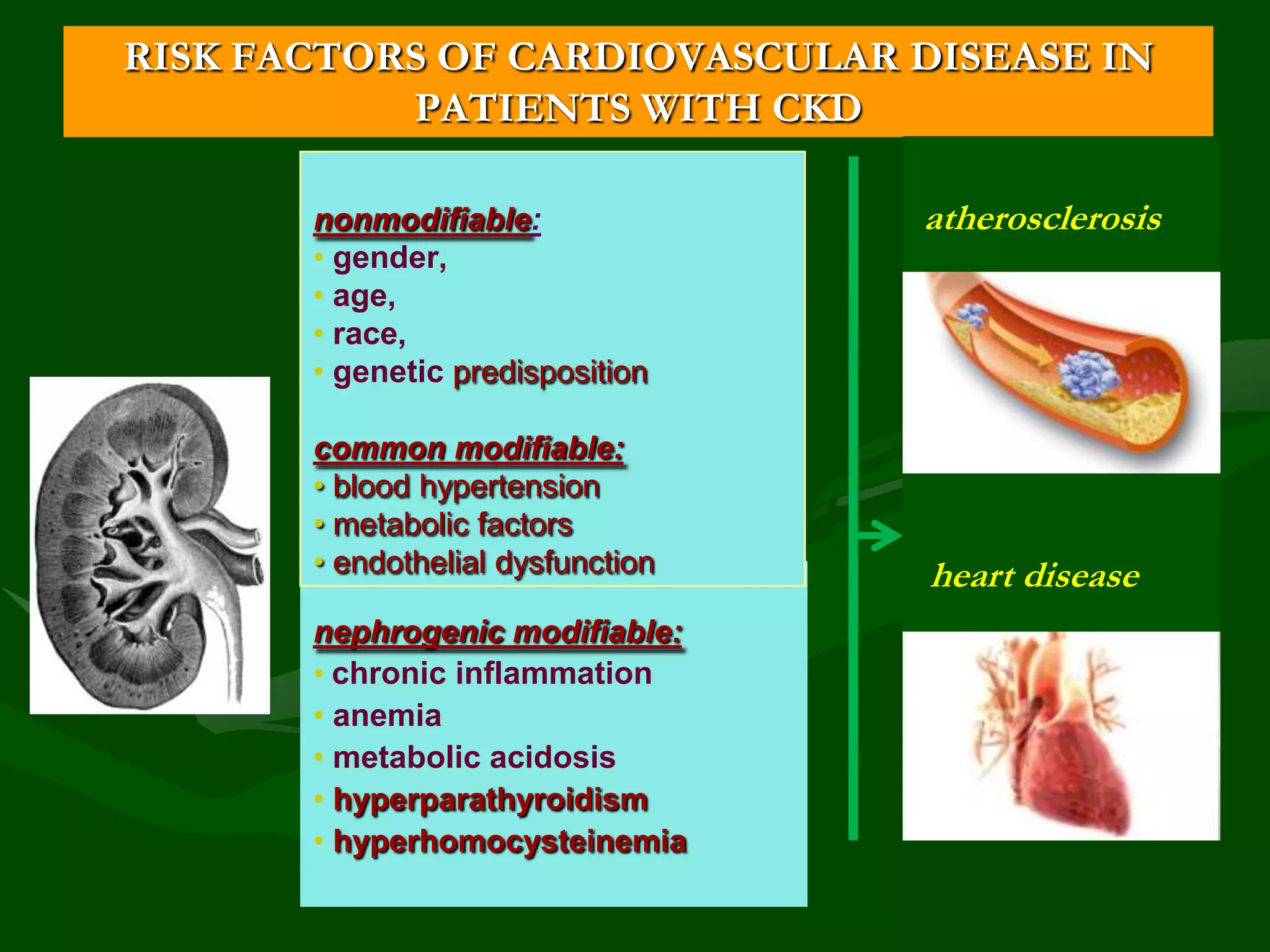
- Risk factors include diabetes, hypertension, smoking, obesity, dyslipidemia, proteinuria, inflammation, and others. CKD itself is an independent risk factor for cardiovascular disease.

![eGFR in children on the basis of serum creatinine
and growth (according to Schwartz)
• GFR (ml/min/1,73m2)= [0,0484*х Height
(сm)]/Scr (mmol/l)
*k= 0,0616 for boys >13 years](https://image.slidesharecdn.com/8-1-131107145955-phpapp01/75/8-1-Progression-of-CKD-to-CRF-Vladimir-Dlin-eng-15-2048.jpg)
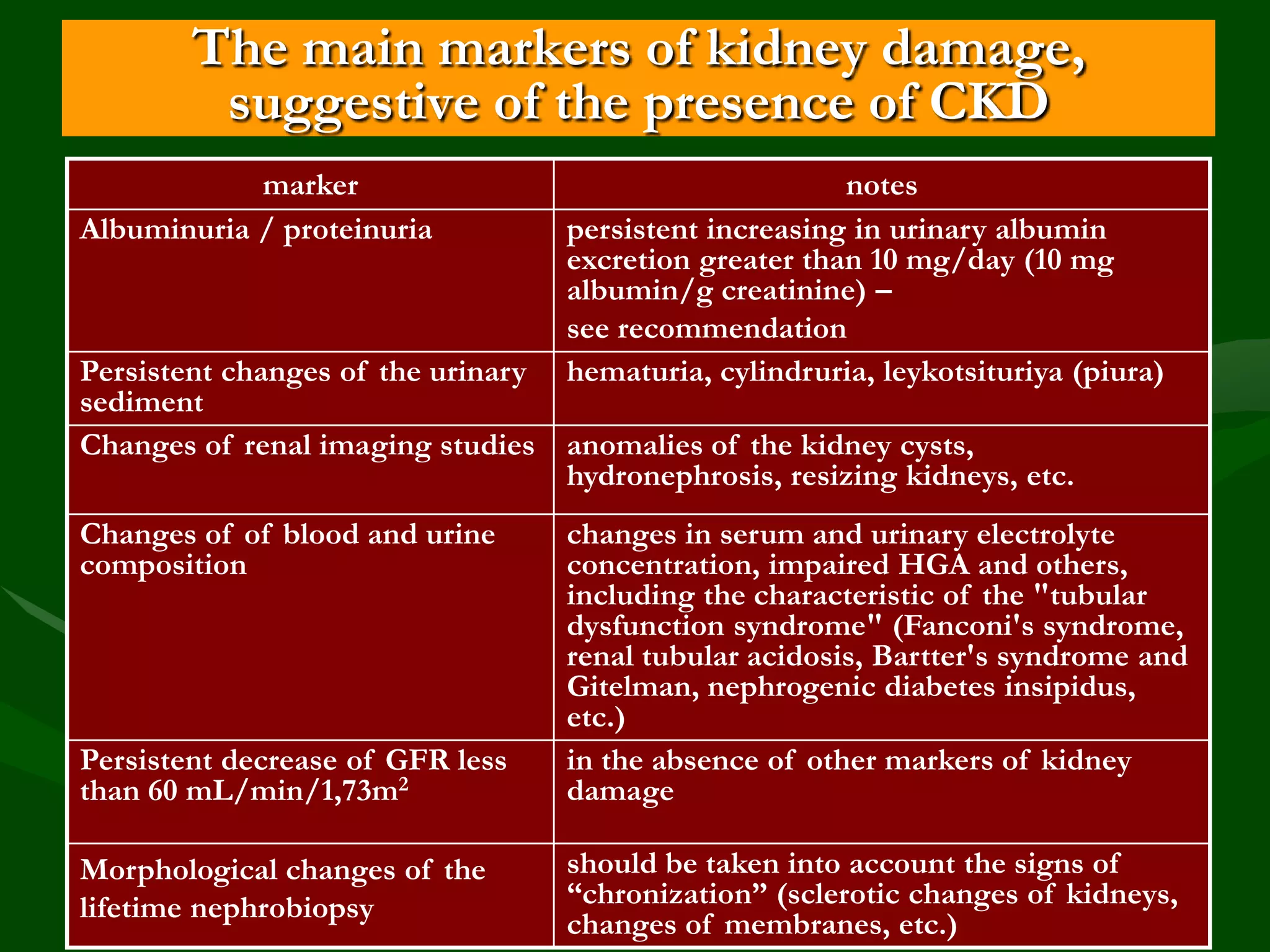
![Albuminuria
• Albuminuria (normal < 10 mg/day) – integral sign of CKD
[A. Smirnov et al., 2010] and represents:
- increased permeability of cell membranes (size-selectivity, the chargeselectivity);
- transport changes in the proximal tubule;
- increased hemodynamic burden on the glomerules;
- presence of systemic and renal endothelial dysfunction;
- the degree of glomerular/interstitial sclerosis due to glomerular and
tubular transport protein disturbances and subsequent activation of
profibrotic cytokines
• Albuminuria – risk factor of total and cardiovascular mortality,
ESRD, acute kidney injury and progression of CKD](https://image.slidesharecdn.com/8-1-131107145955-phpapp01/75/8-1-Progression-of-CKD-to-CRF-Vladimir-Dlin-eng-18-2048.jpg)