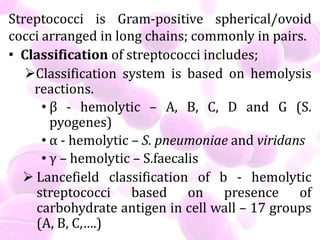
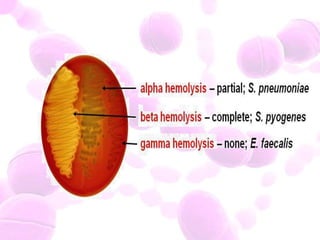
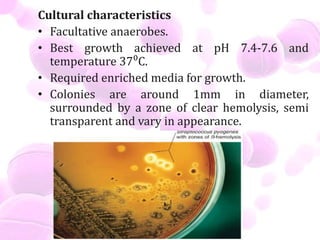
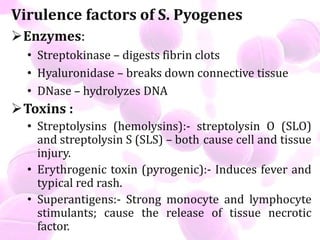
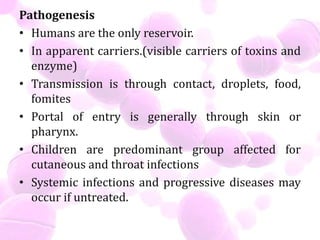
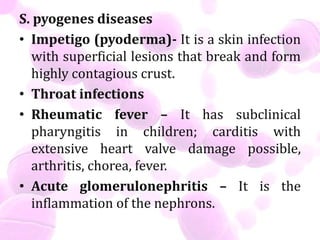
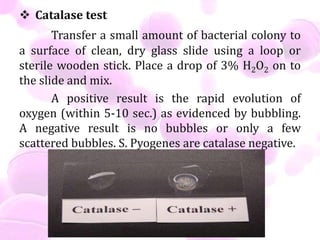
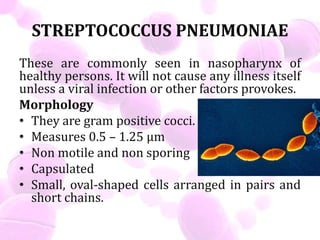
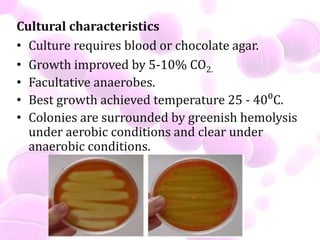
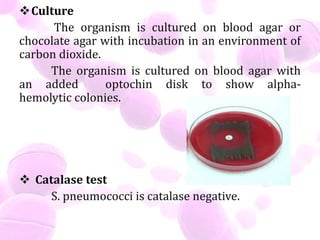
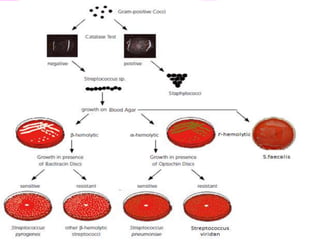
Streptococci are classified based on their hemolysis reactions. S. pyogenes causes serious infections like impetigo, pharyngitis, rheumatic fever and glomerulonephritis. It produces enzymes and toxins as virulence factors. S. pneumoniae commonly resides in the nasopharynx and can cause pneumonia and otitis media. It is diagnosed using gram stain, culture and catalase test. S. viridans and S. faecalis can also cause infections and are treated with appropriate antibiotics.