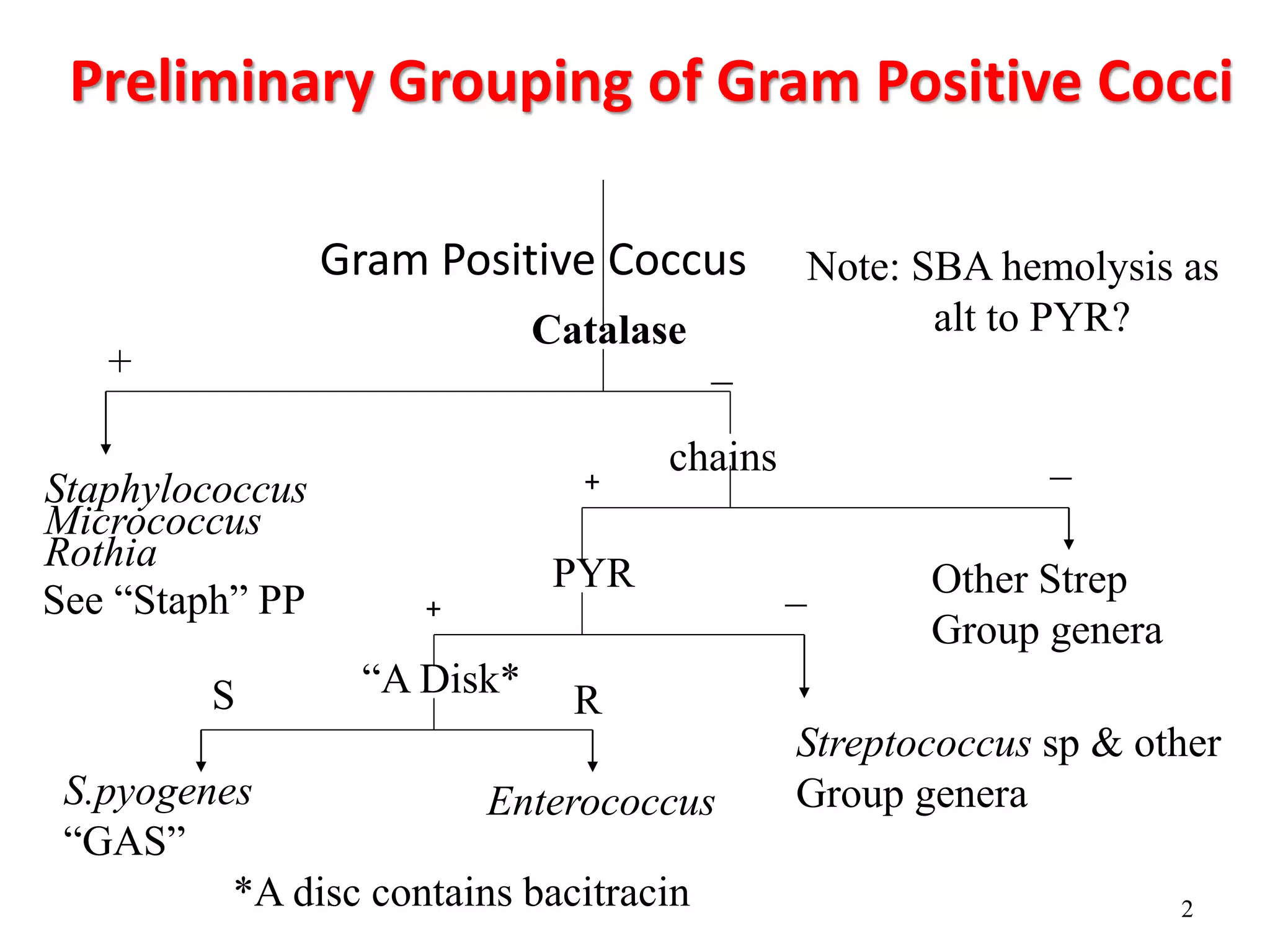
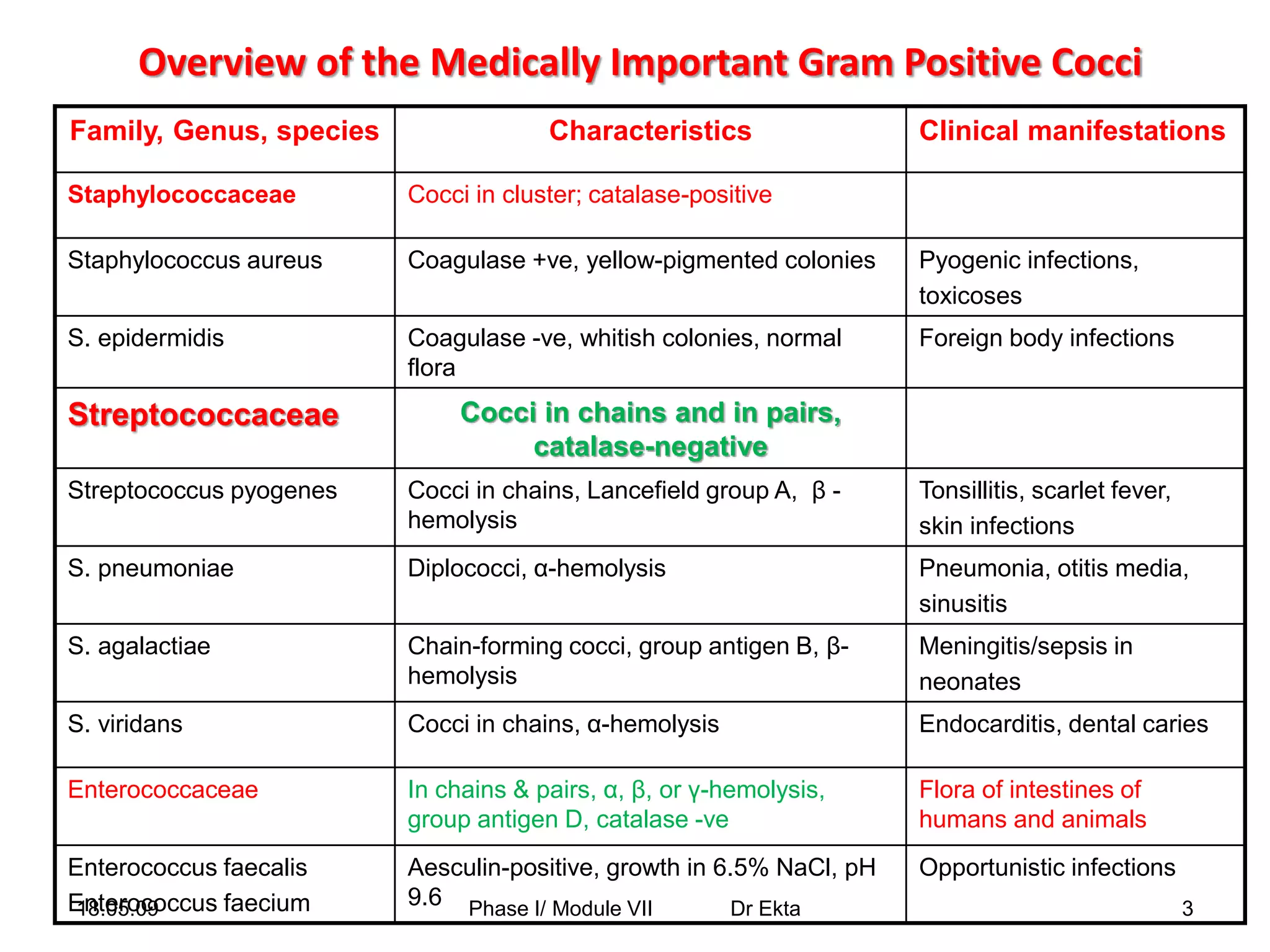
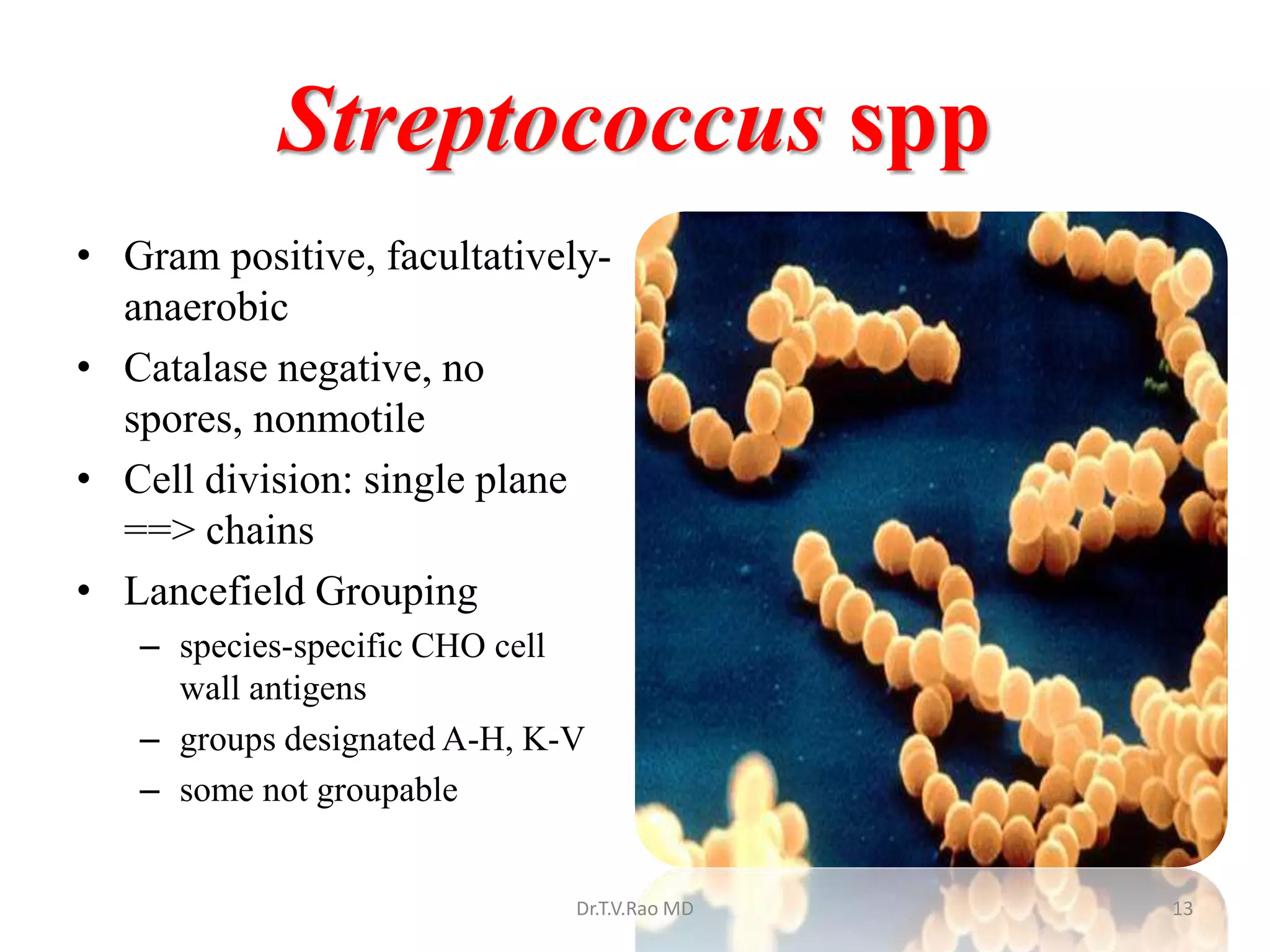
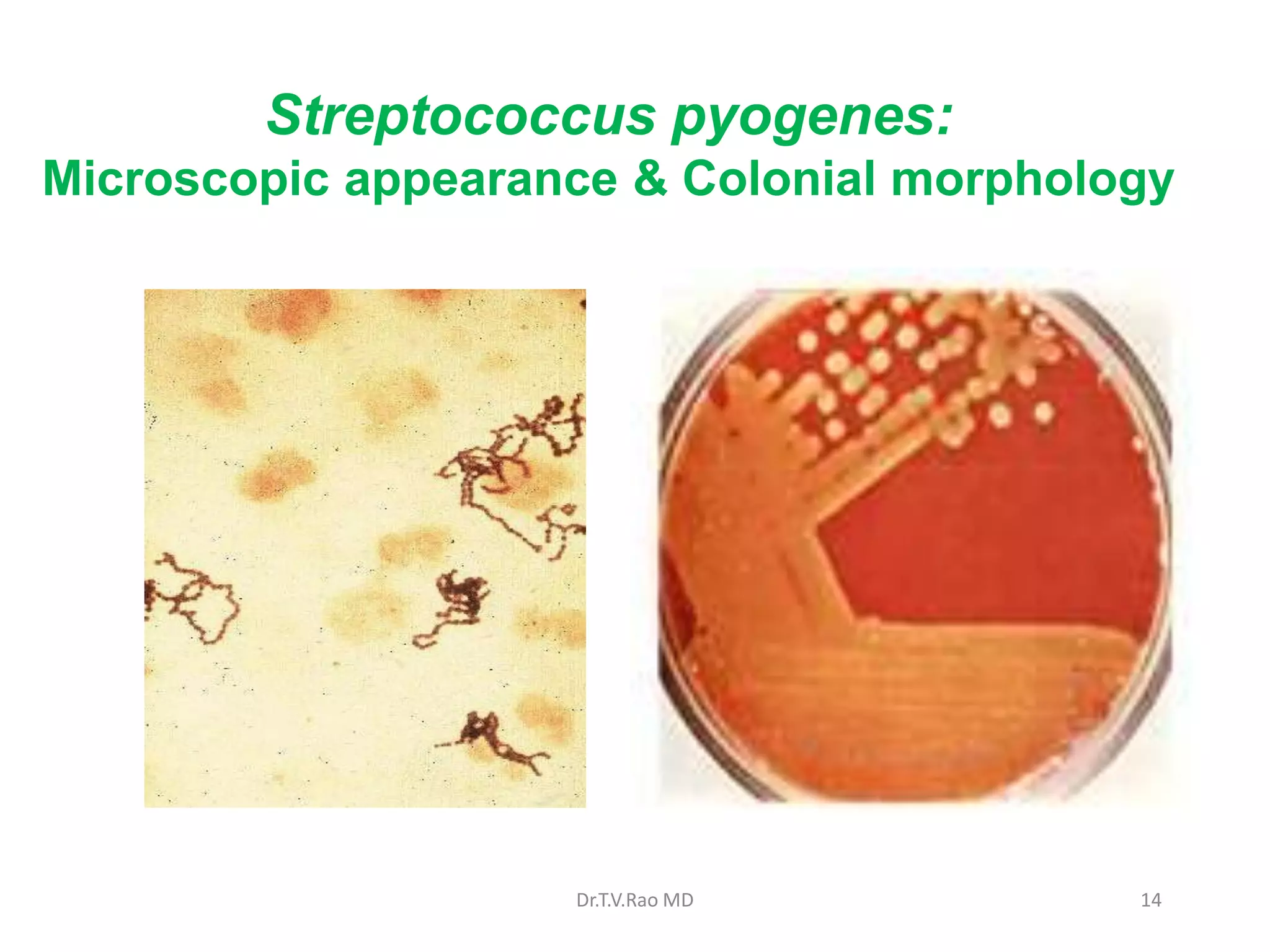
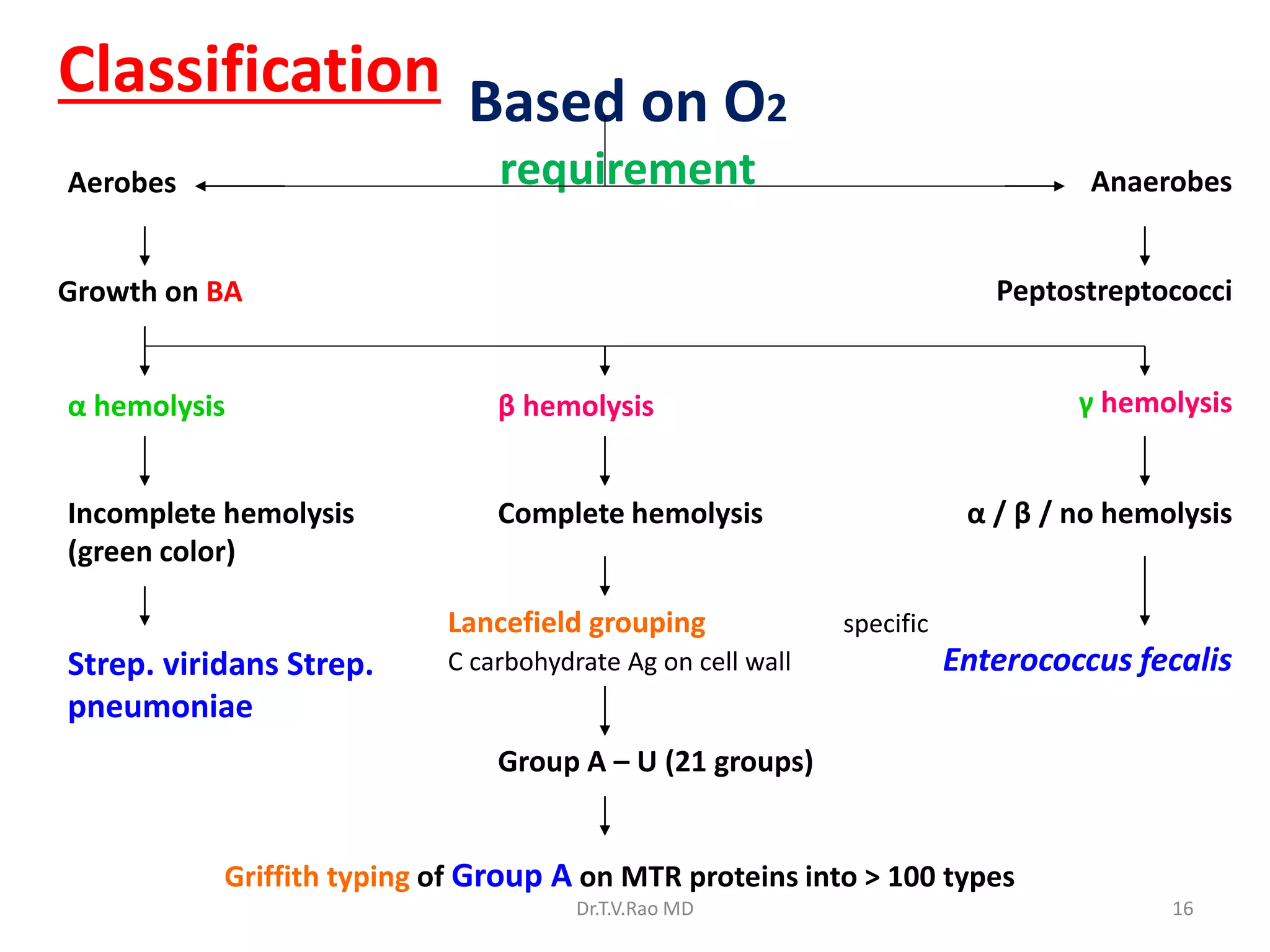
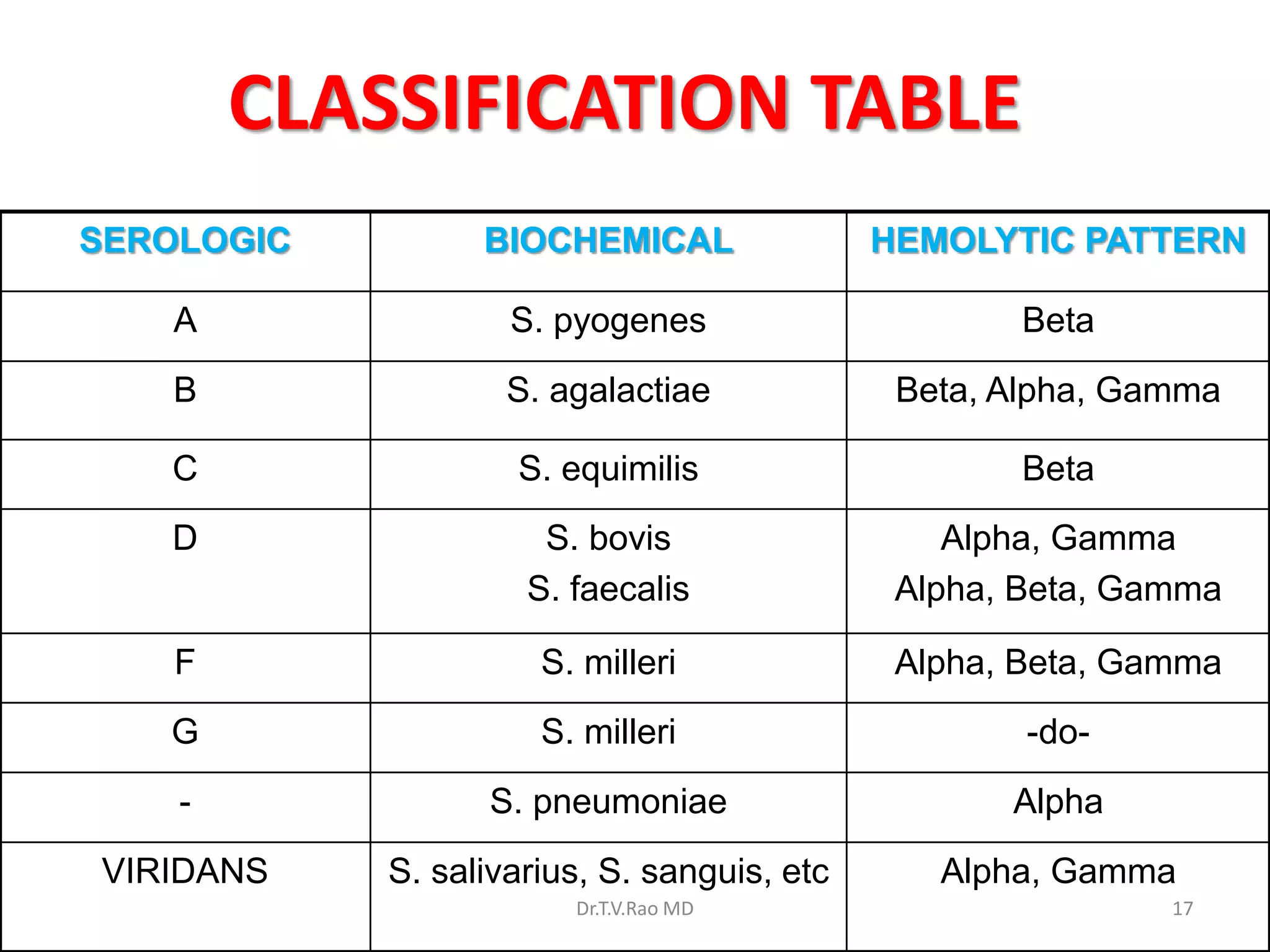
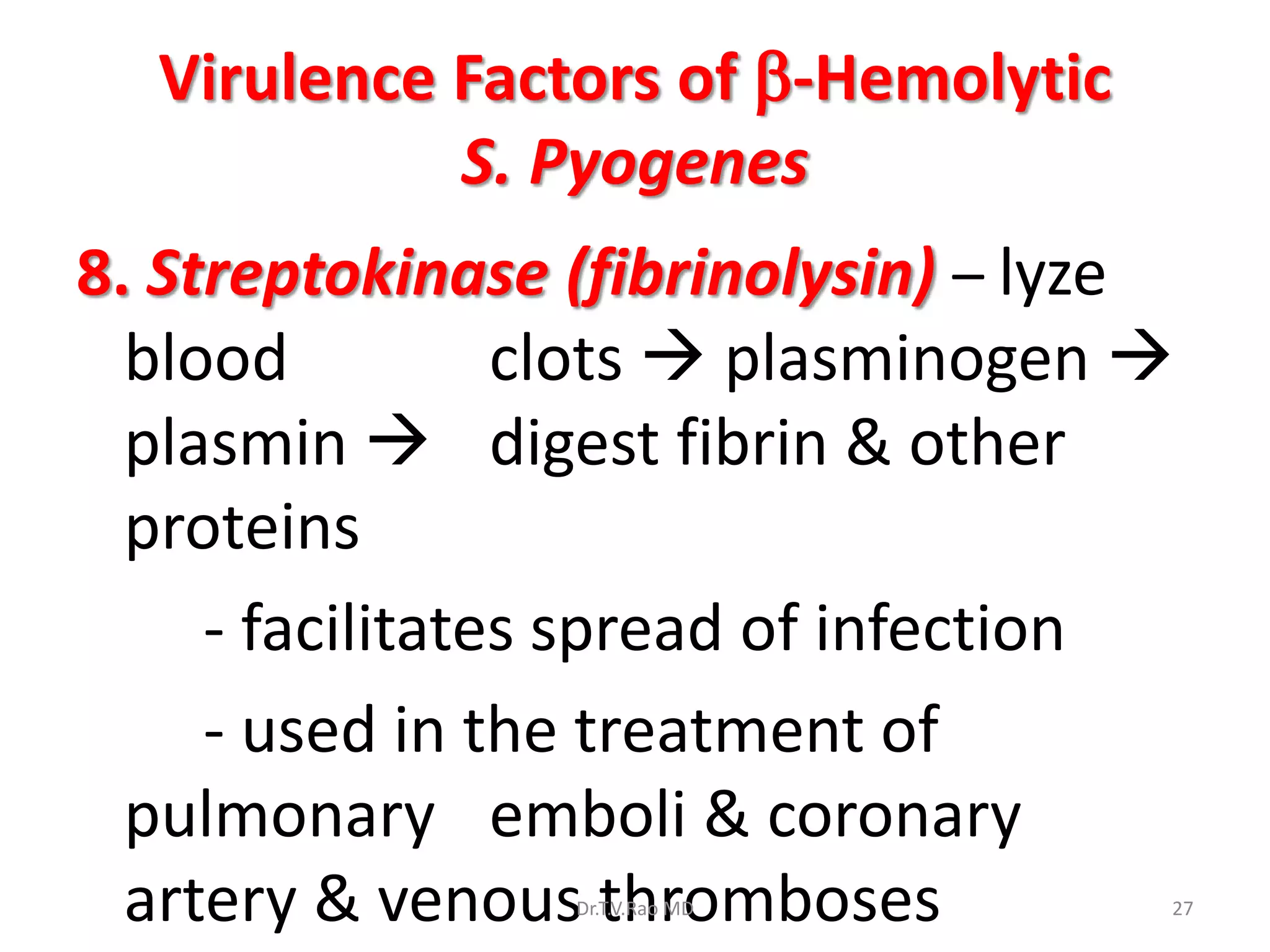
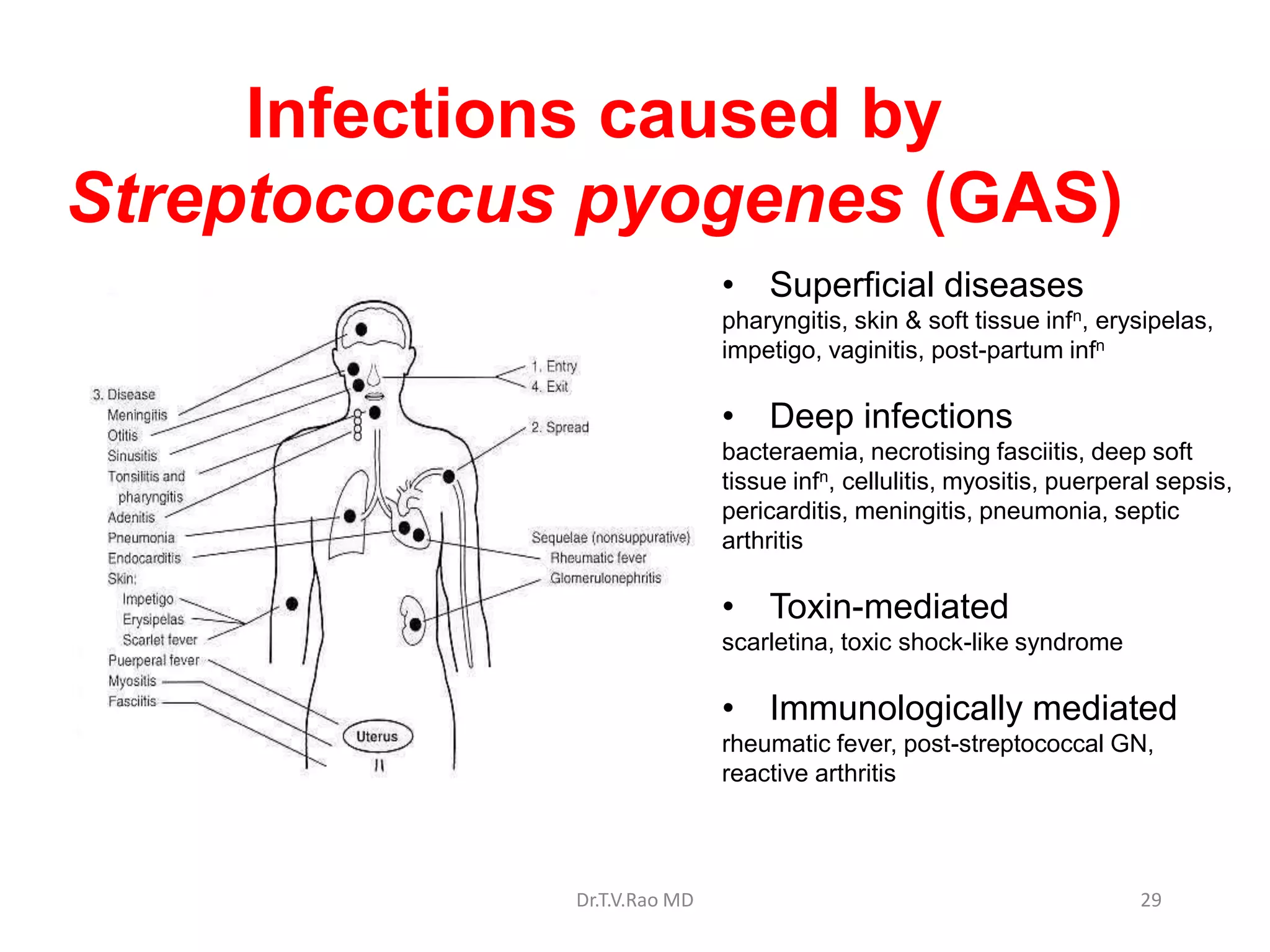
Group A Streptococcus, or Streptococcus pyogenes, is an important human pathogen. It is classified based on Lancefield grouping, which identifies the carbohydrate antigens present in the bacterial cell wall. S. pyogenes is in Lancefield Group A and causes a variety of infections through various virulence factors like M protein, streptolysin toxins, and extracellular enzymes. These virulence factors allow the bacteria to adhere to tissues, resist phagocytosis, damage host cells, and spread infection. Common infections include pharyngitis, impetigo, and potentially life-threatening illnesses like necrotizing fasciitis and toxic shock syndrome.