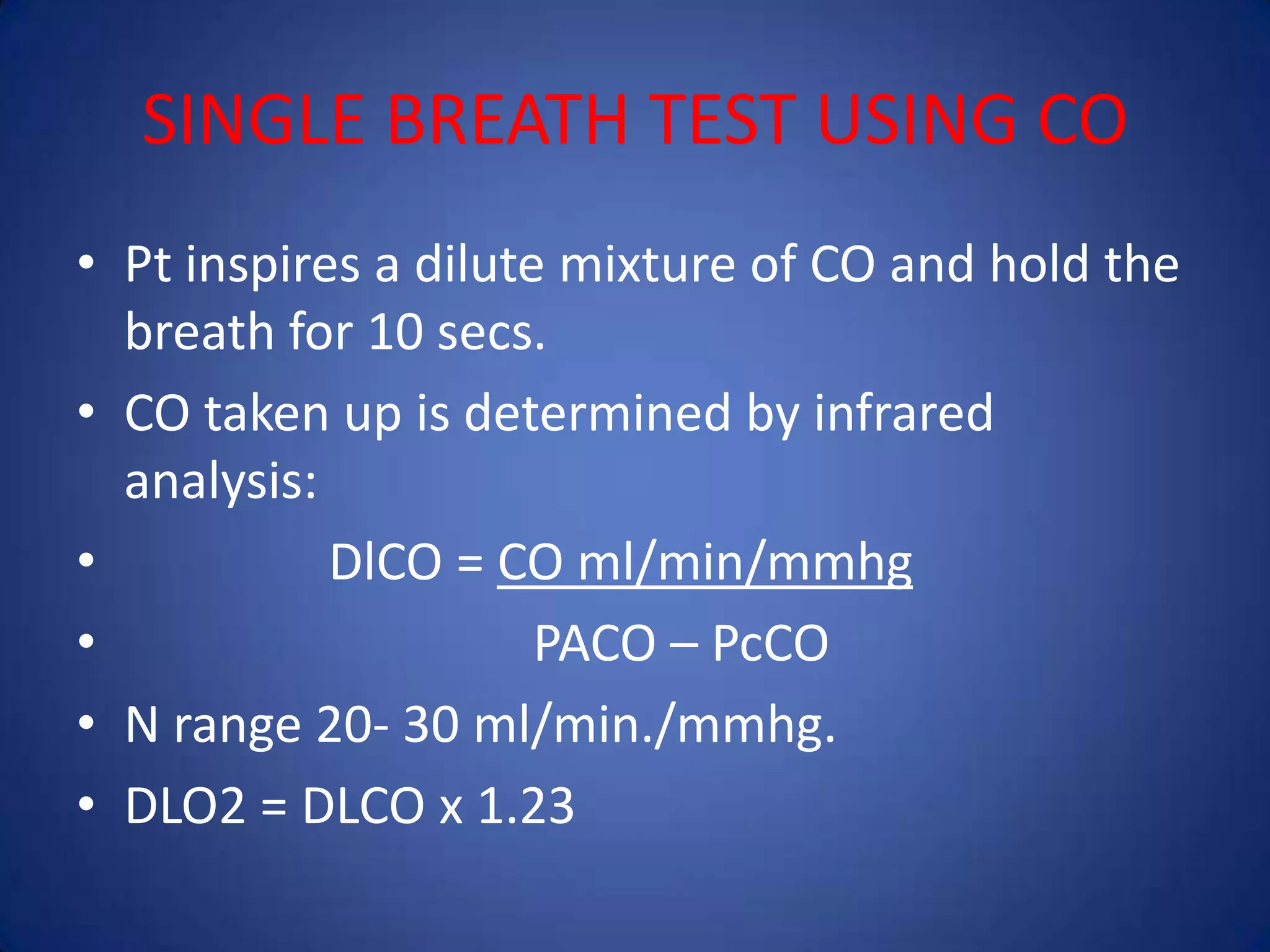
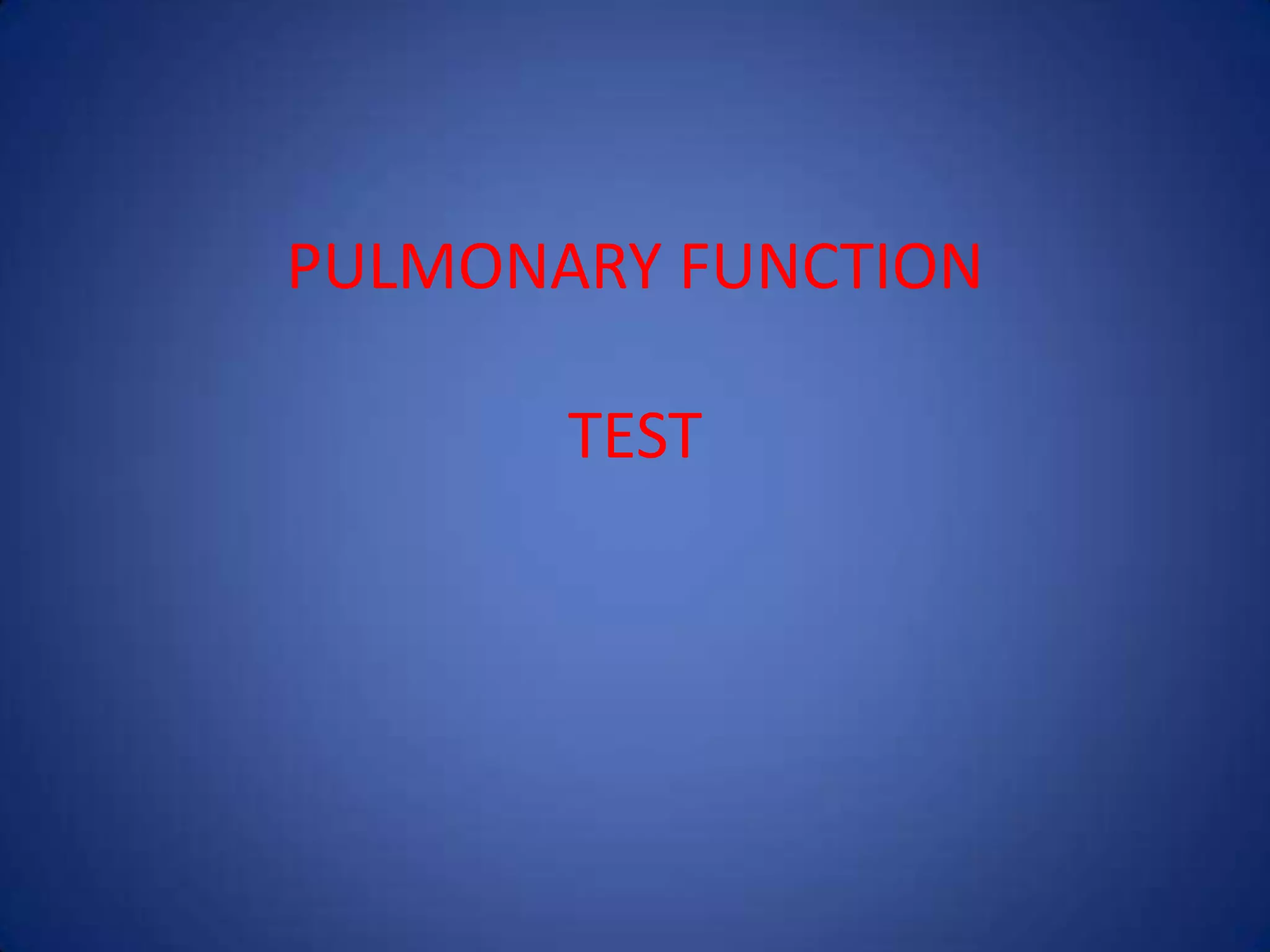
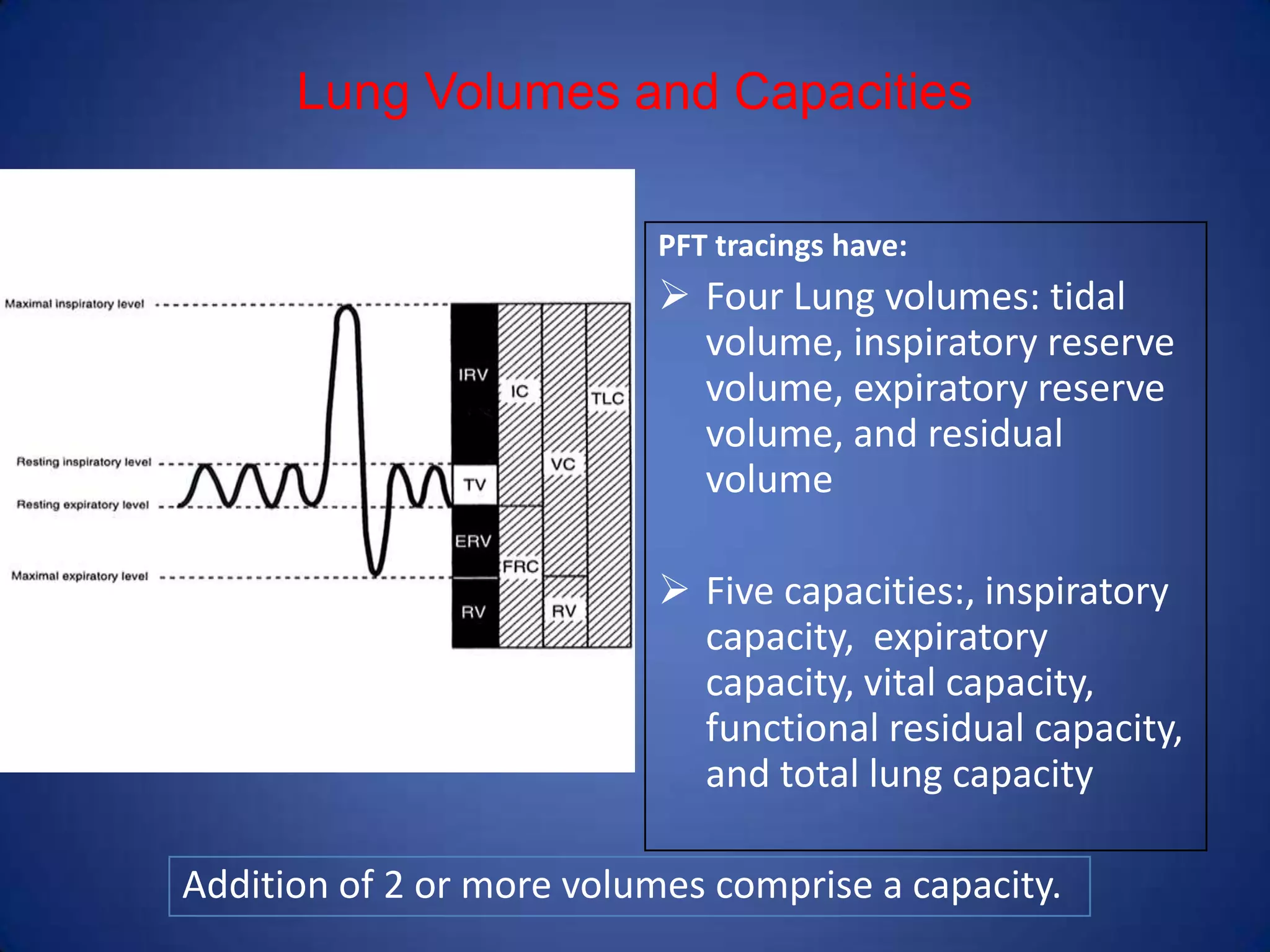
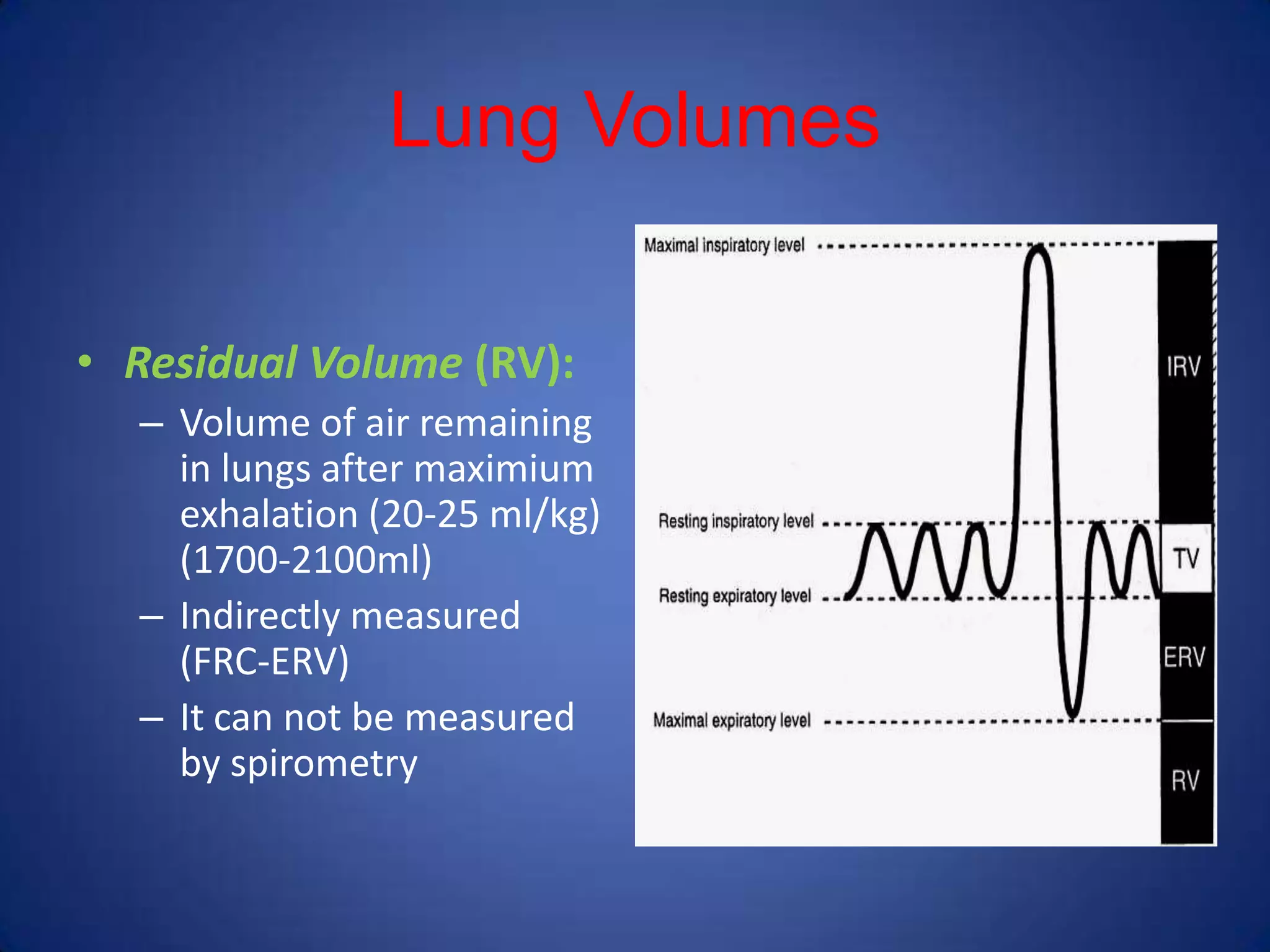
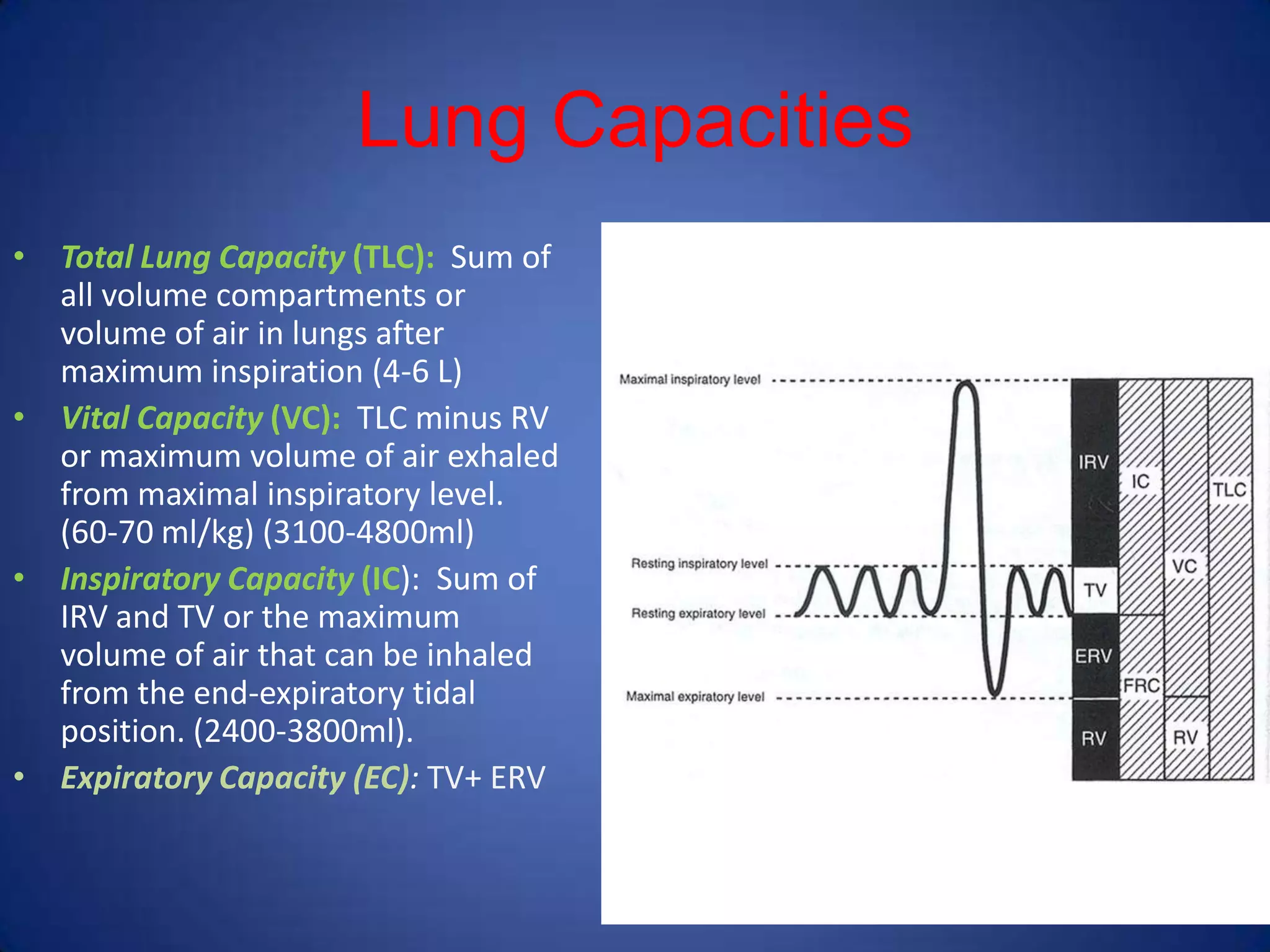
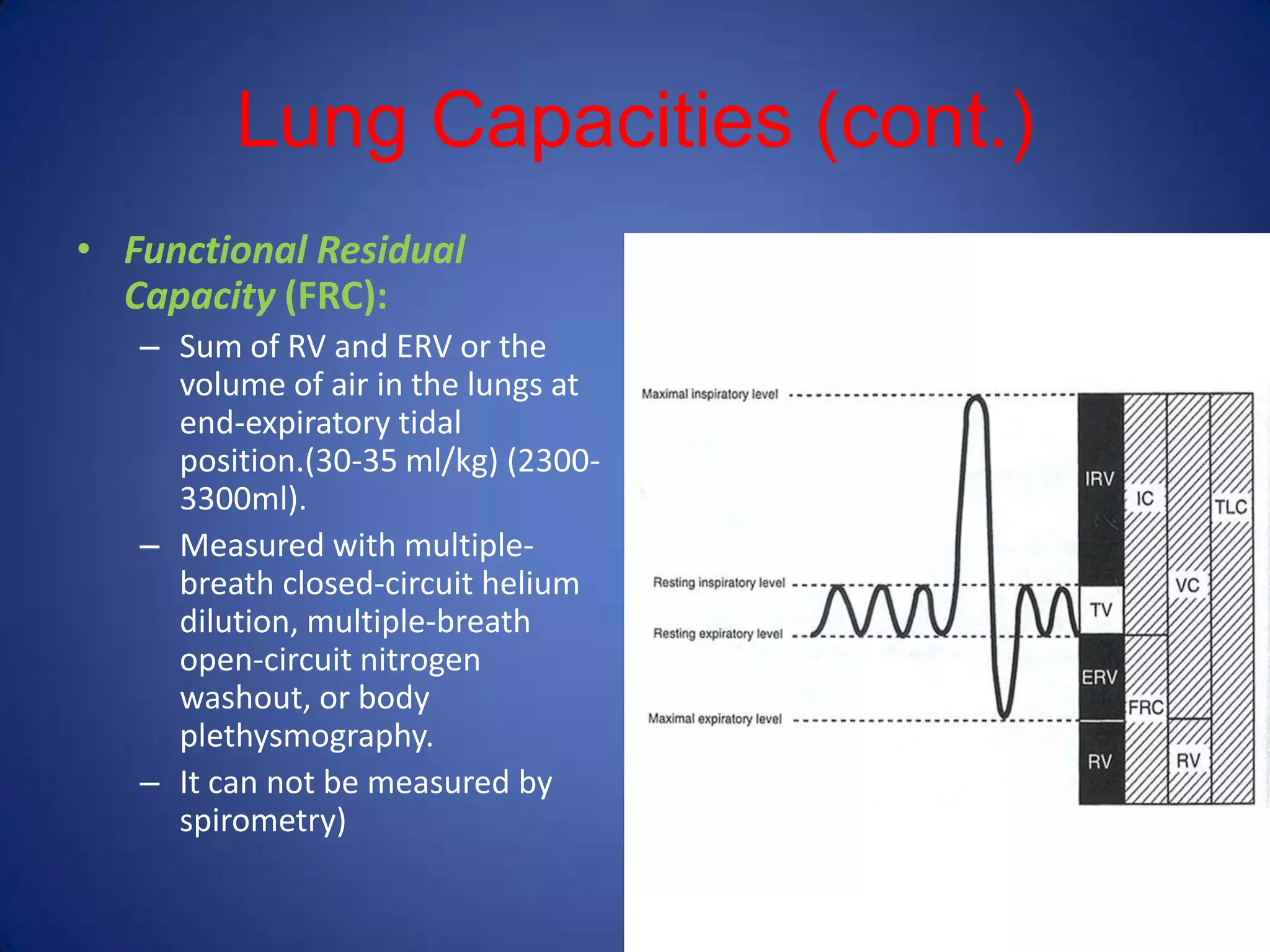
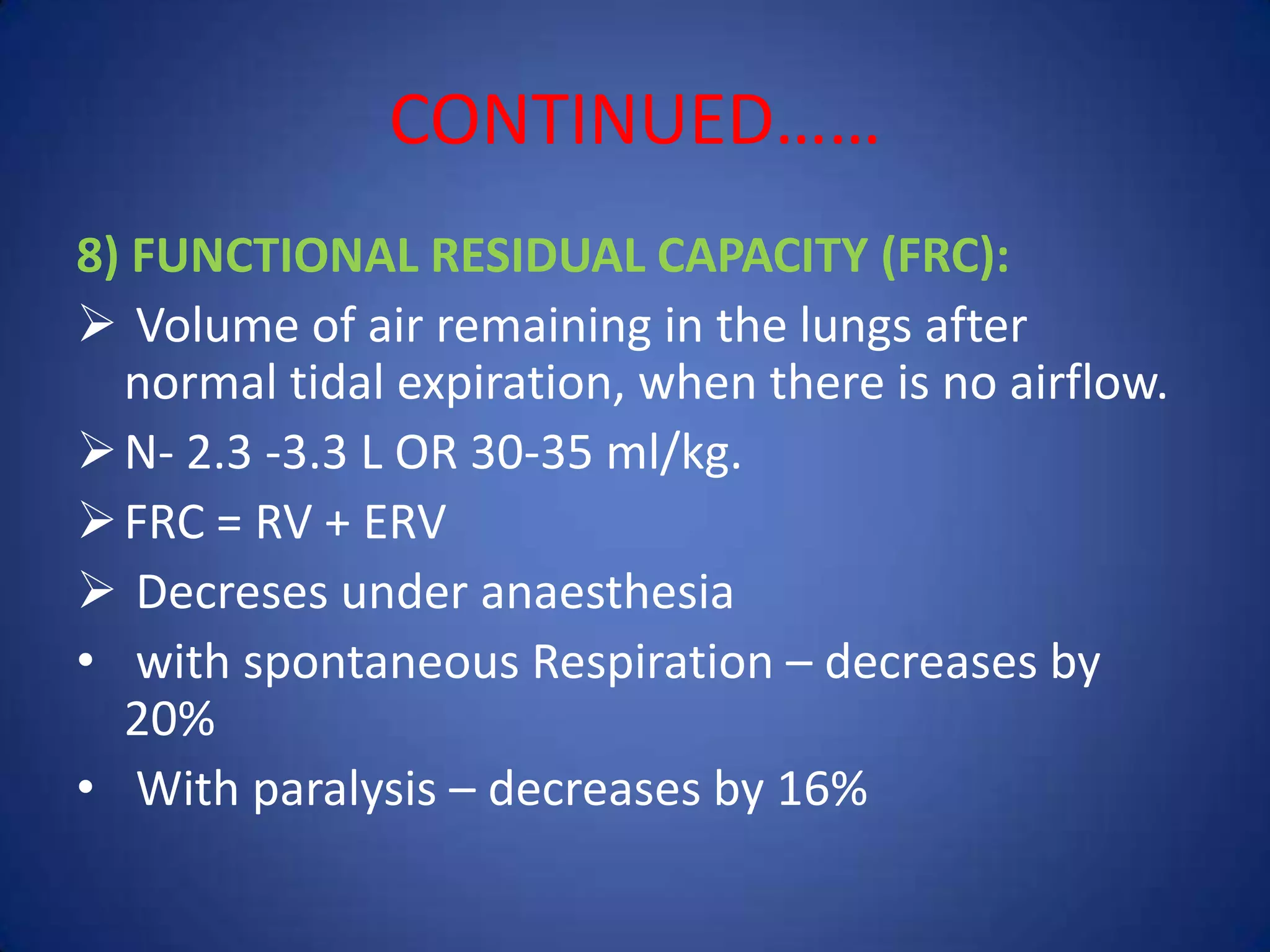
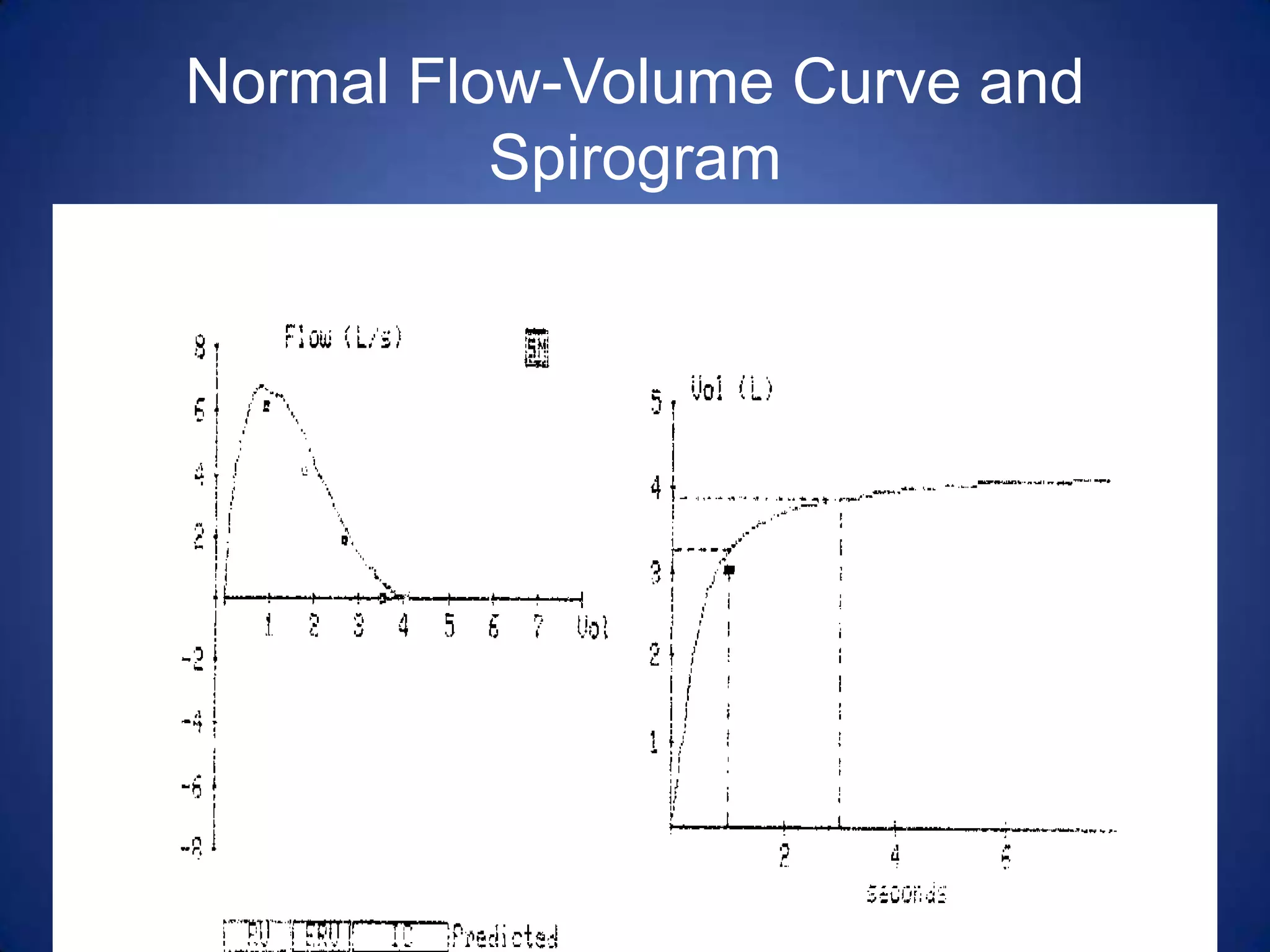
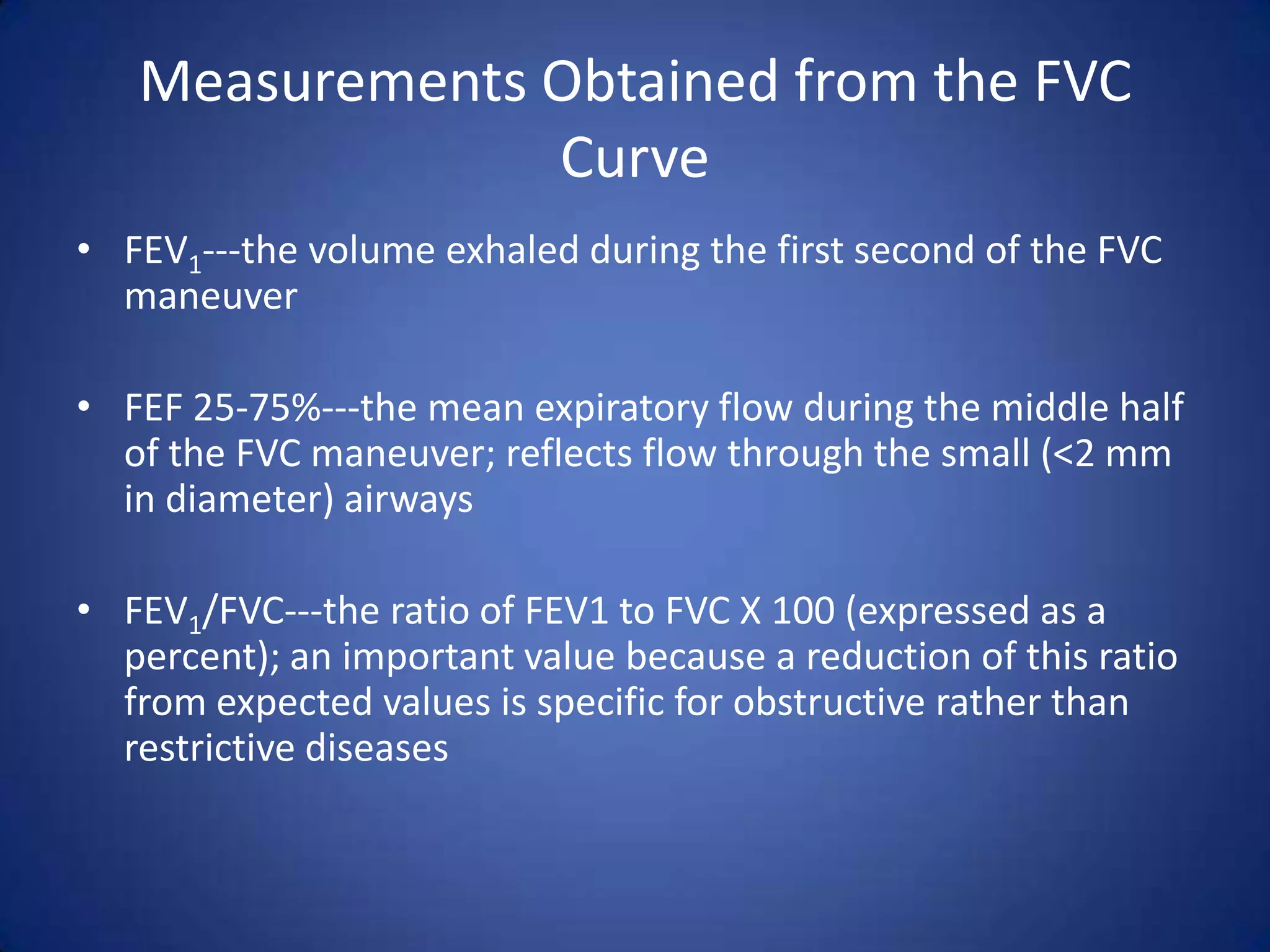
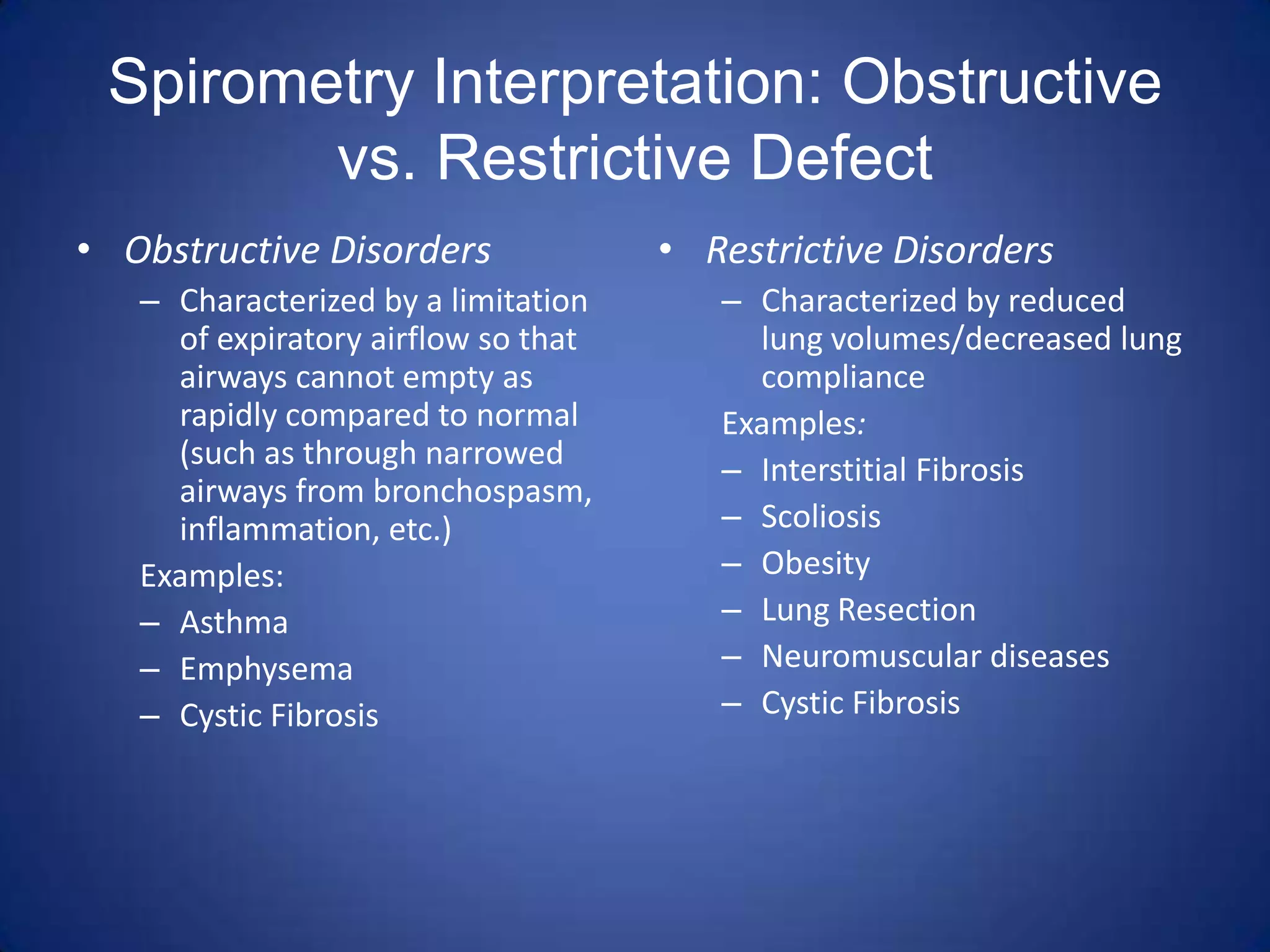
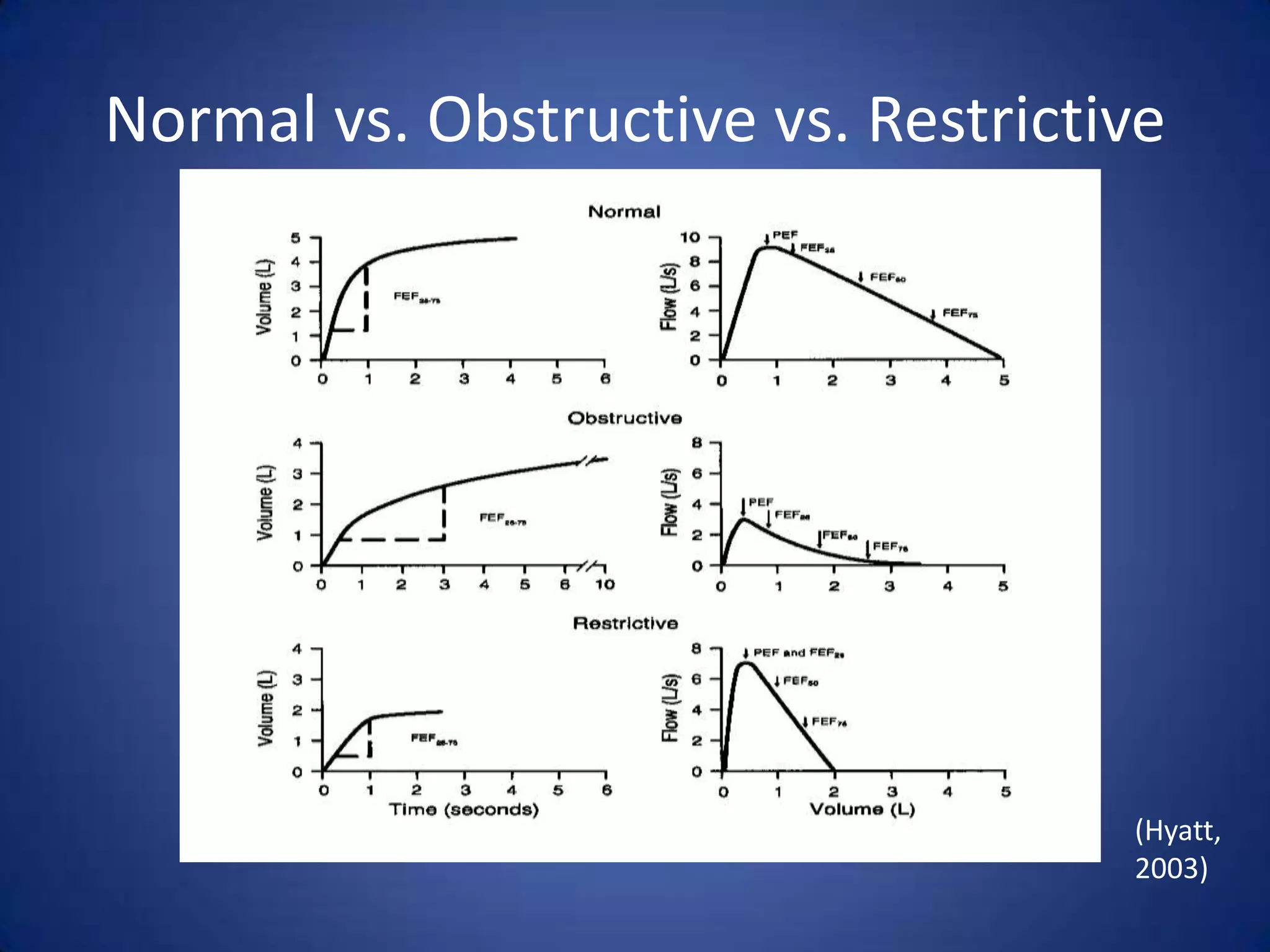
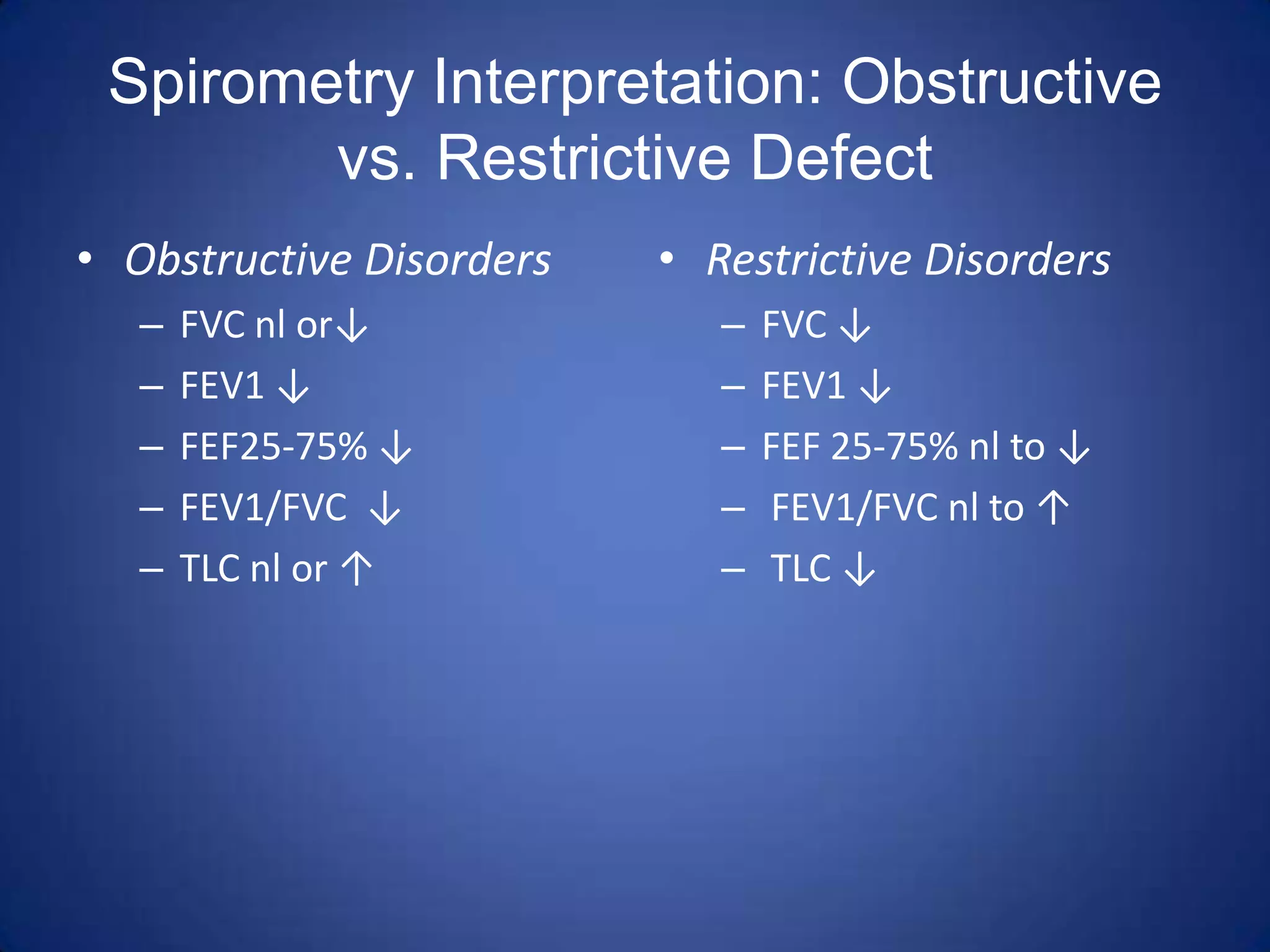
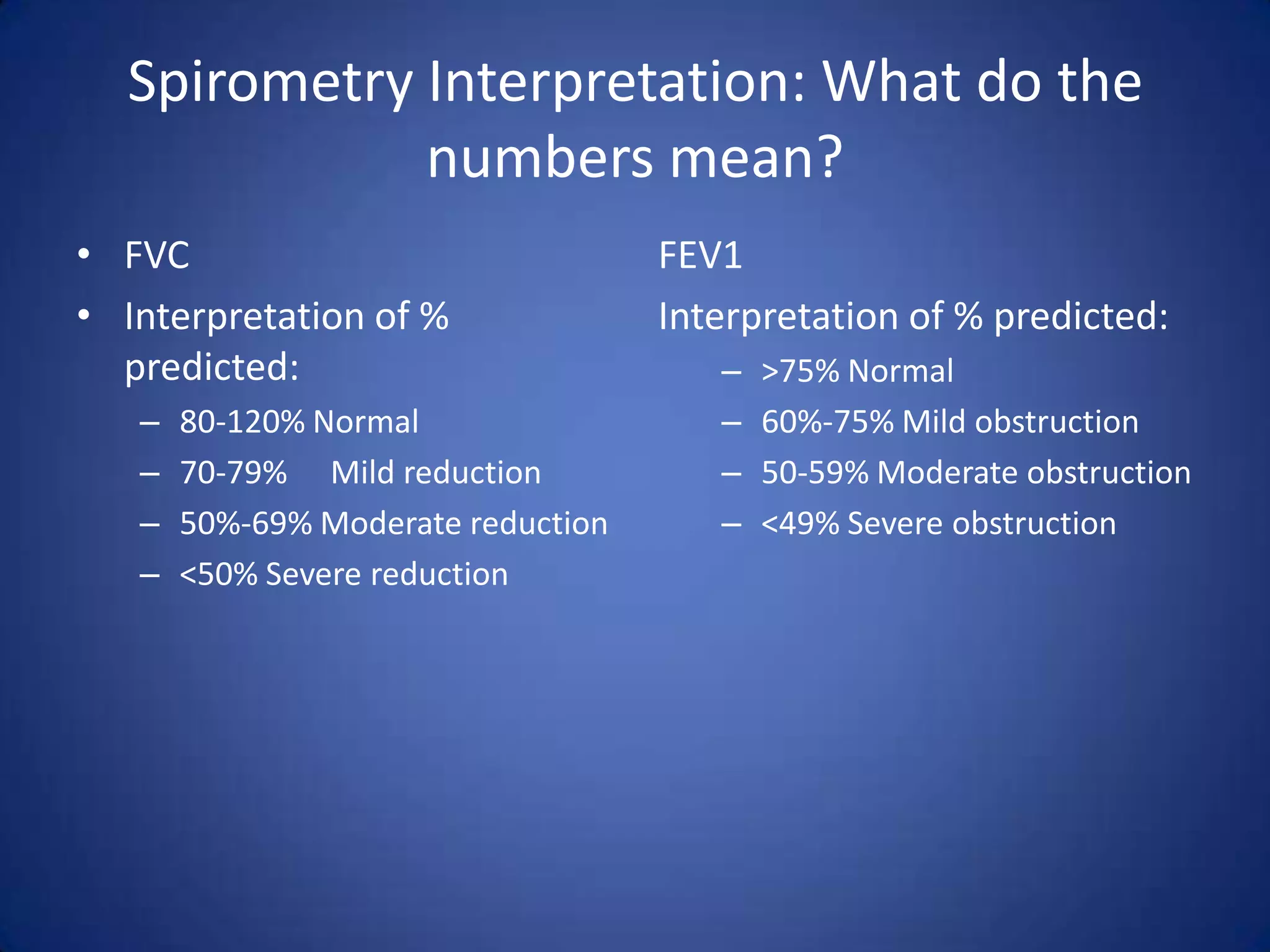
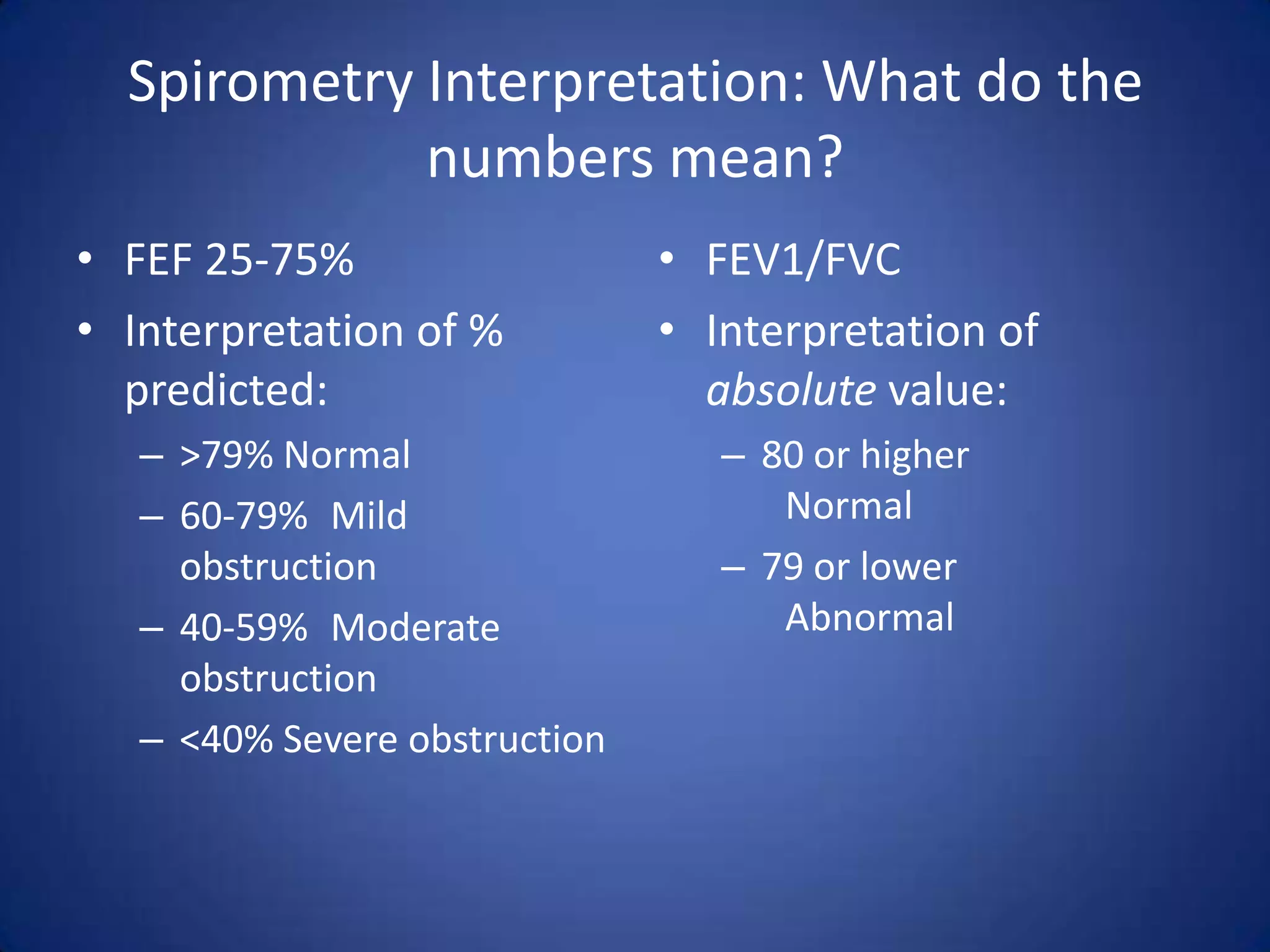
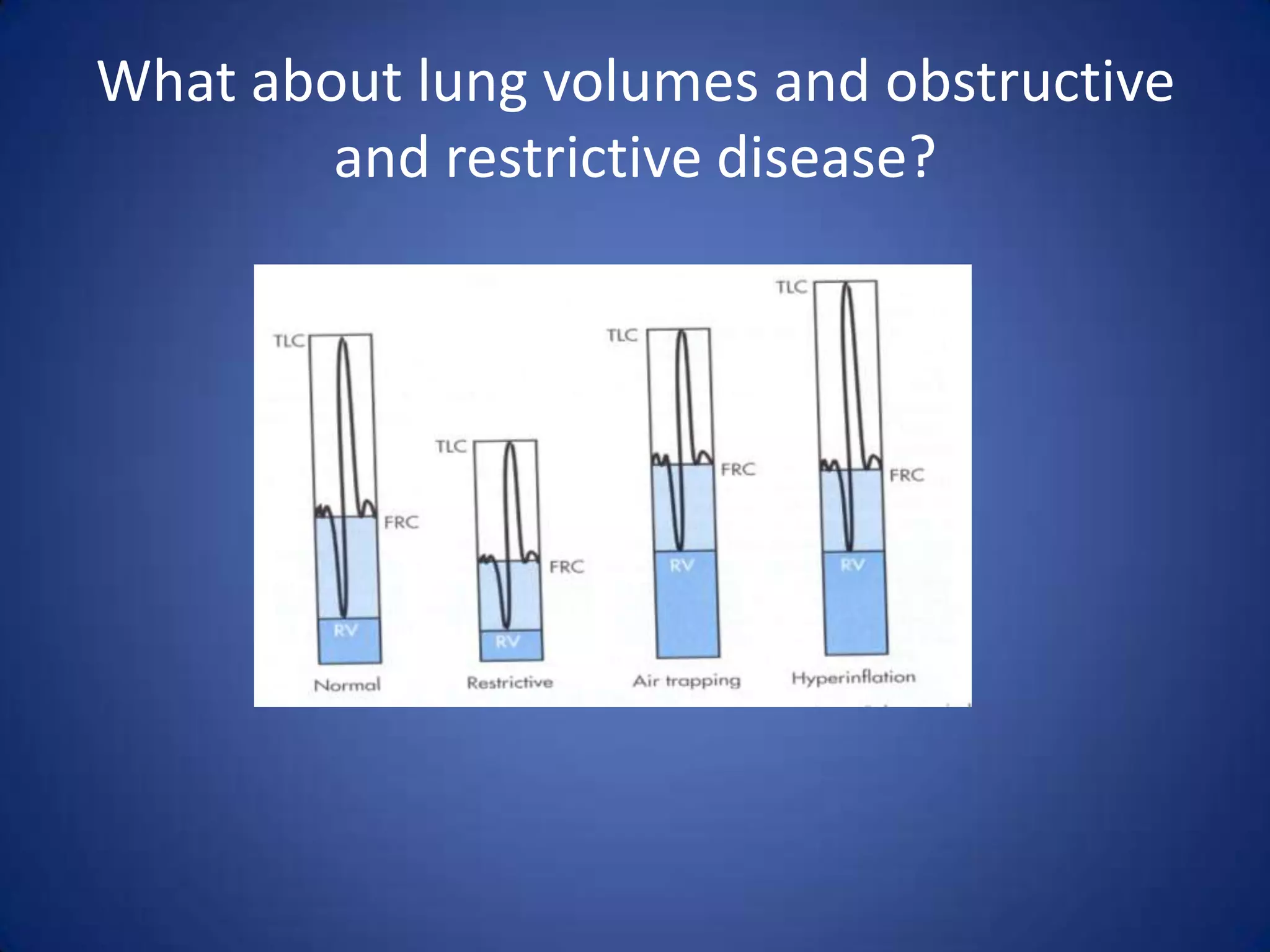
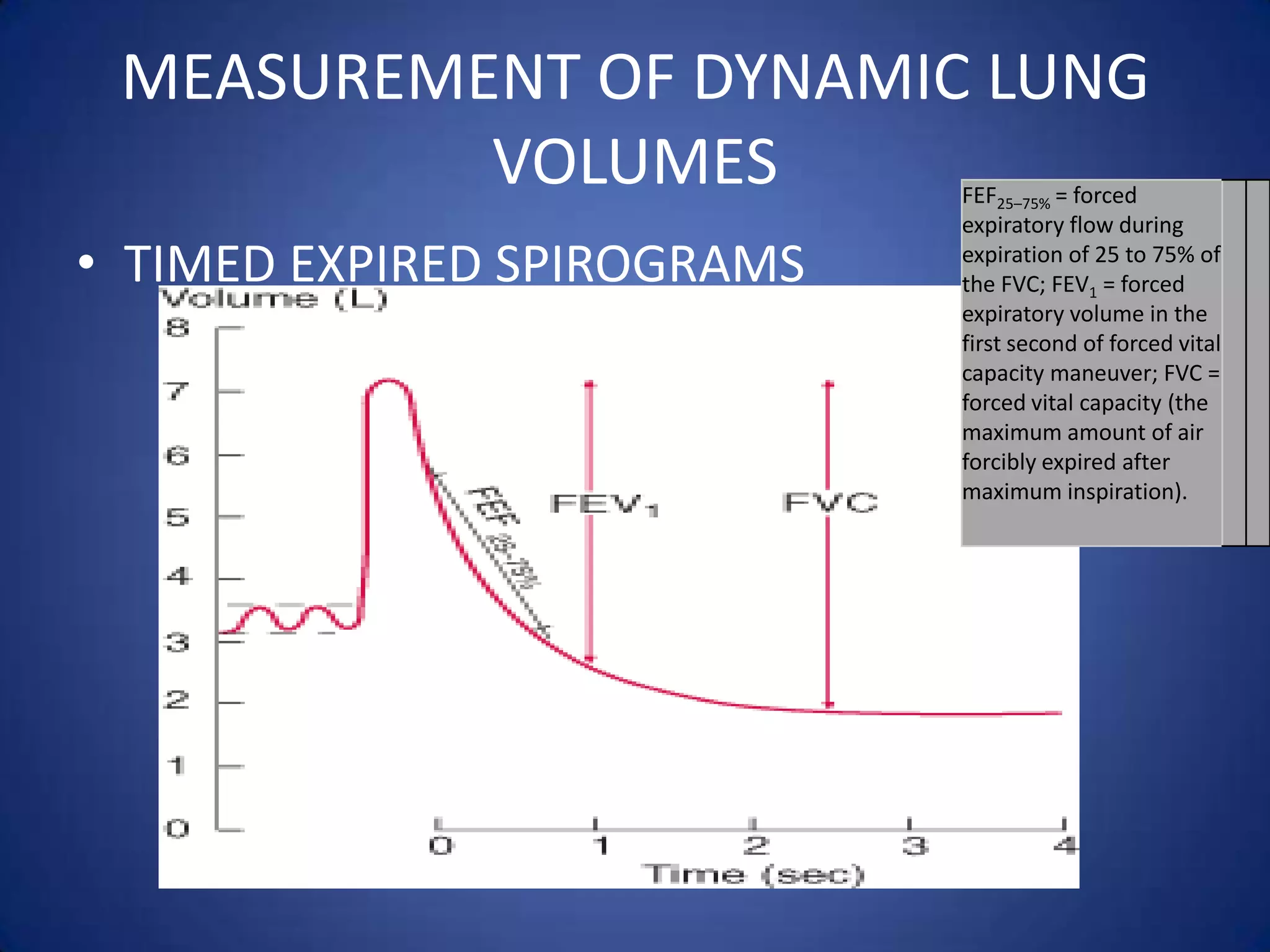
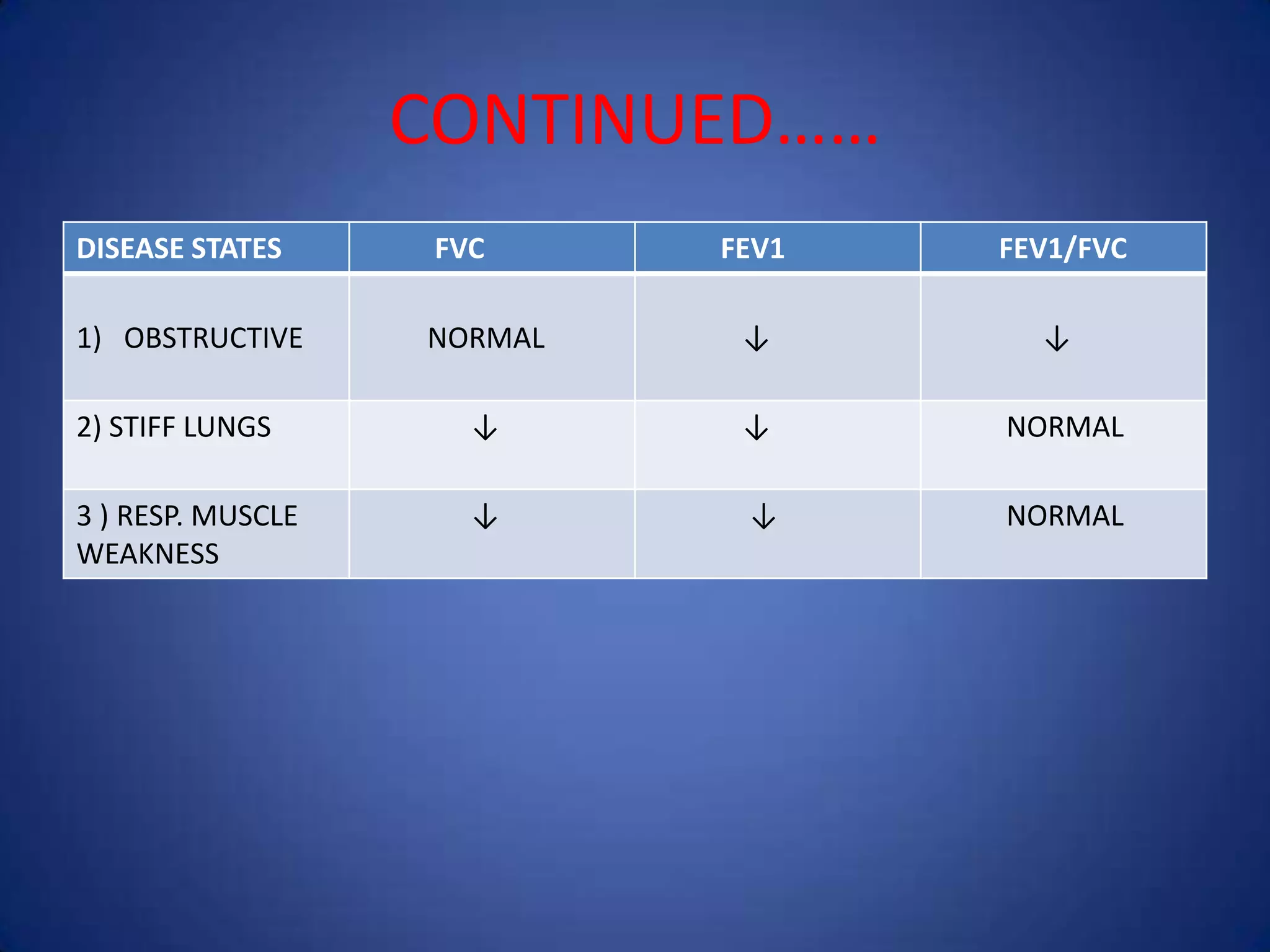
Lung volumes and capacities can be measured using spirometry. There are four lung volumes - tidal volume, inspiratory reserve volume, expiratory reserve volume, and residual volume. There are also five lung capacities, which are combinations of the lung volumes - inspiratory capacity, expiratory capacity, vital capacity, functional residual capacity, and total lung capacity. Spirometry is used to measure the volumes exhaled during a forced vital capacity maneuver, including the forced expiratory volume in 1 second (FEV1) and ratios like FEV1/FVC, to distinguish between obstructive and restrictive lung diseases.

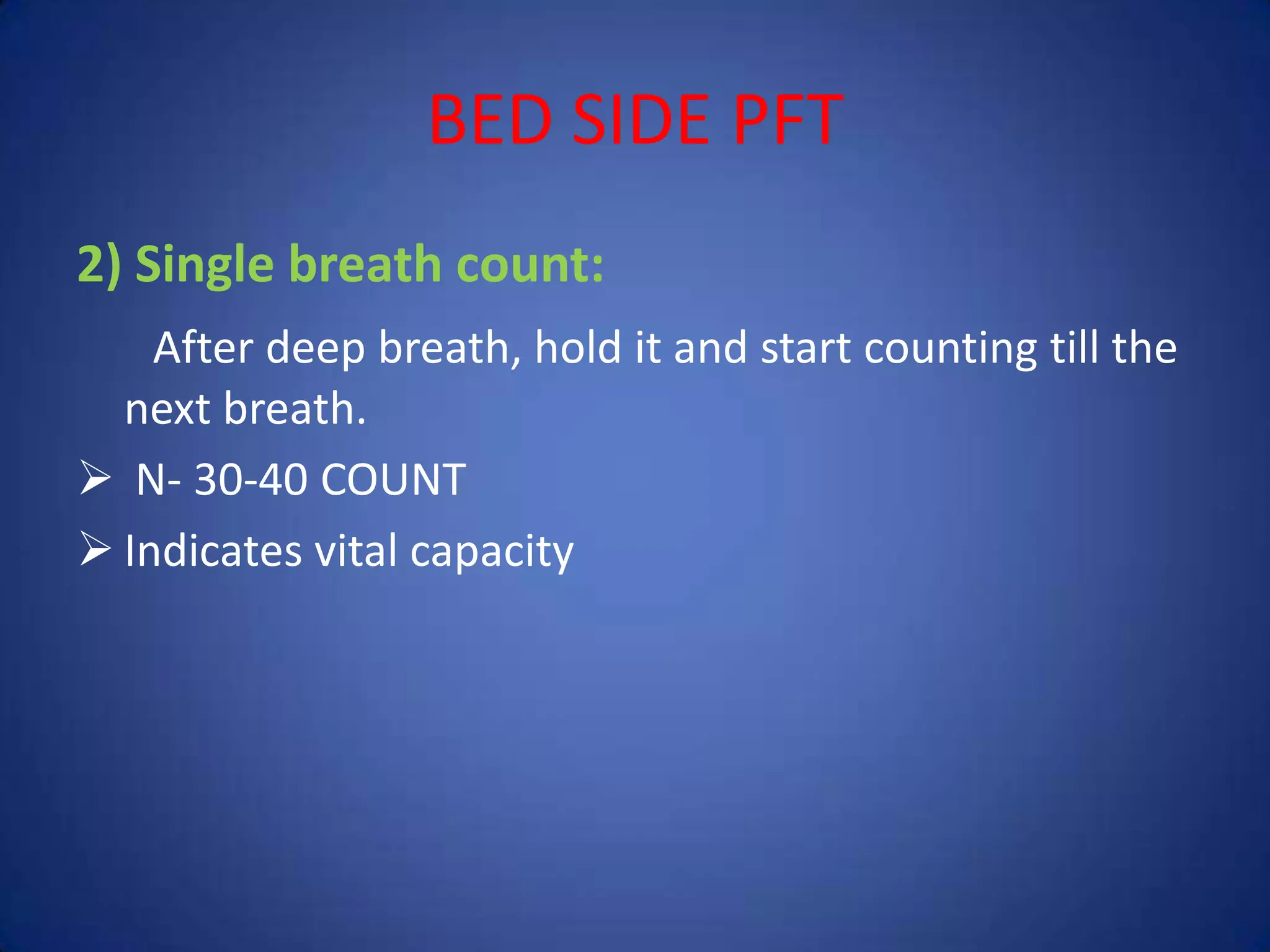
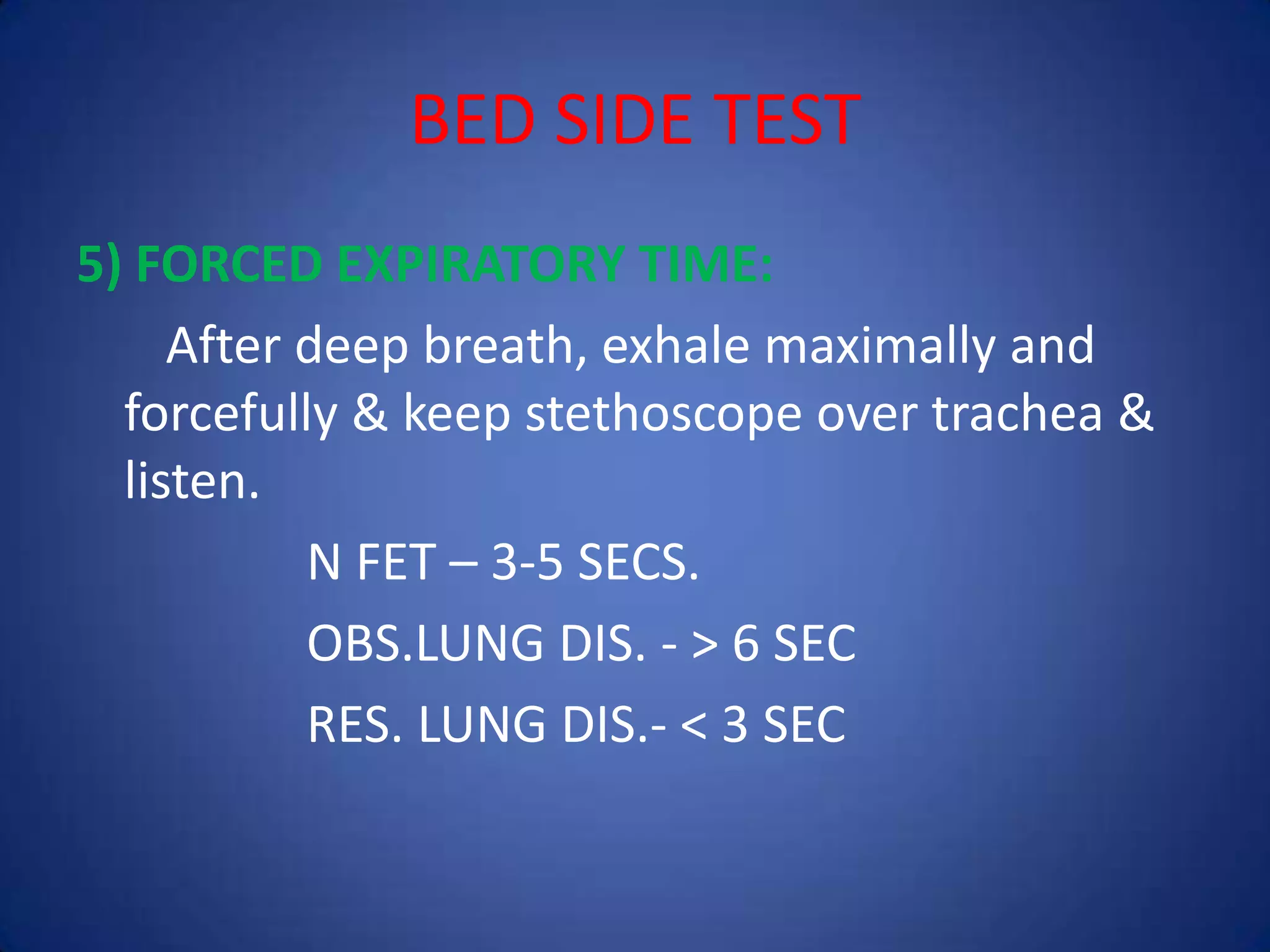


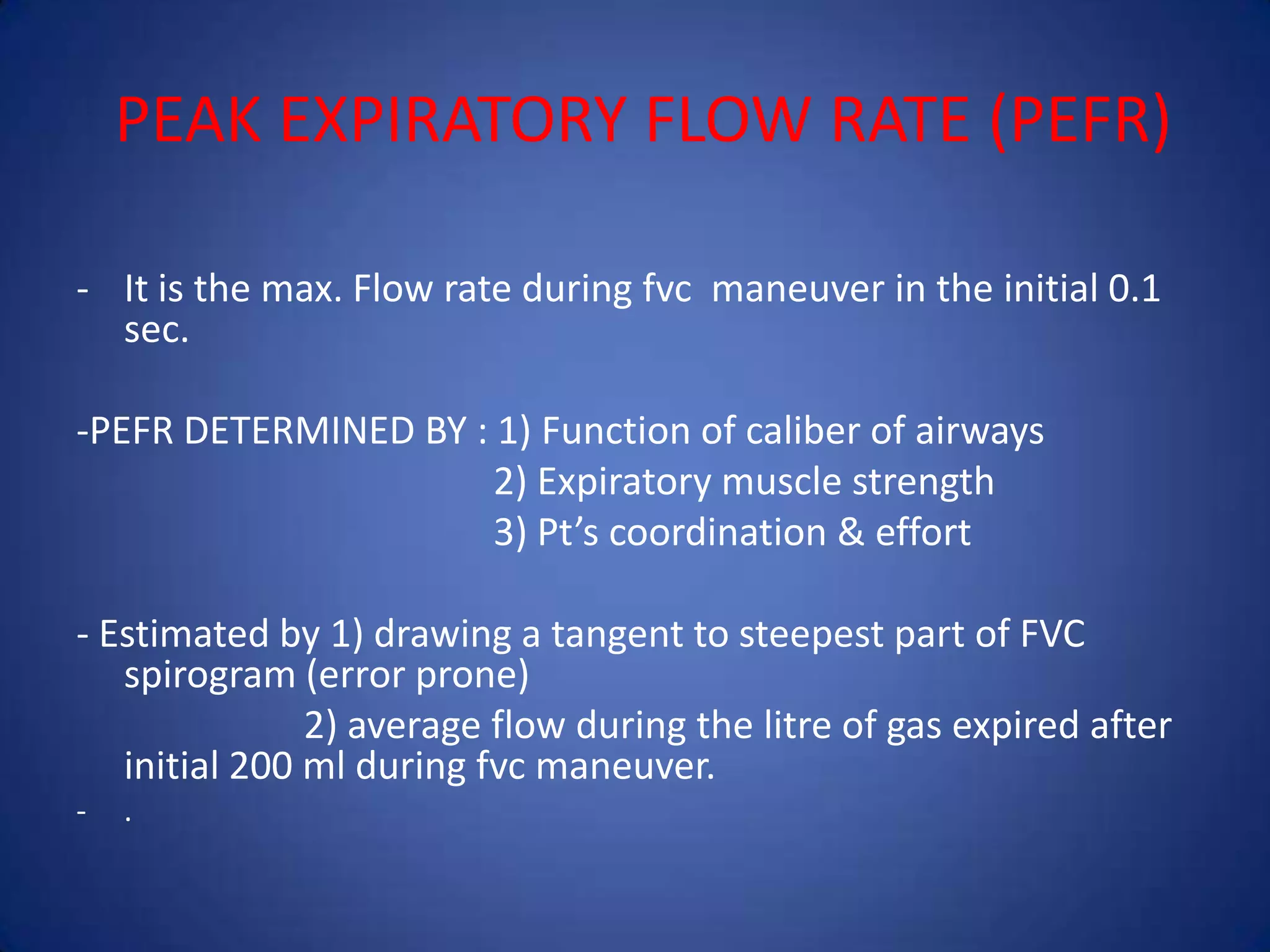
![Spirometry Pre and Post Bronchodilator
• Obtain a flow-volume loop.
• Administer a bronchodilator.
• Obtain the flow-volume loop again a minimum of 15
minutes after administration of the bronchodilator.
• Calculate percent change (FEV1 most commonly
used---so % change FEV 1= [(FEV1 Post-FEV1
Pre)/FEV1 Pre] X 100).
• Reversibility is with 12% or greater change.](https://image.slidesharecdn.com/14-140401014041-phpapp02/75/14-pulmonary-function-tests-67-2048.jpg)