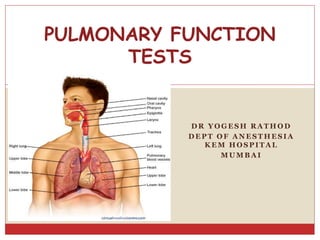
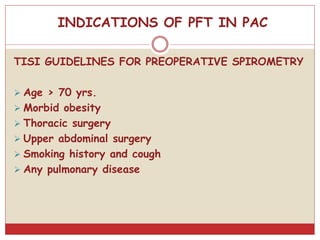
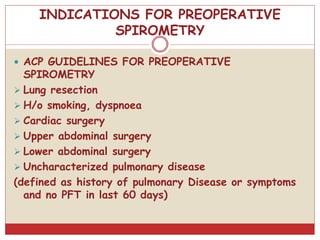
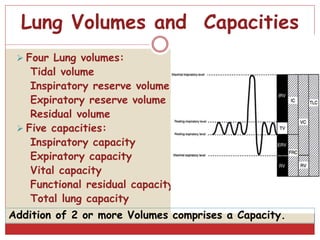
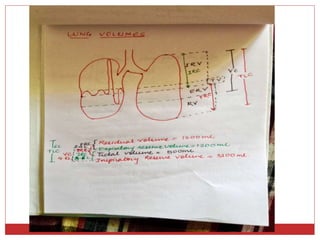
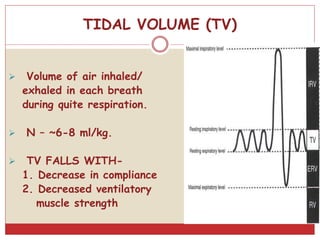
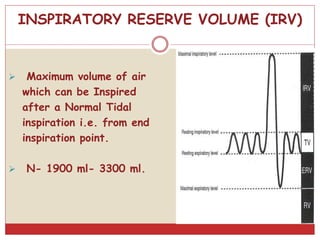
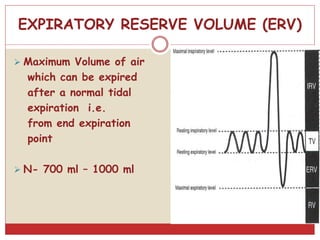
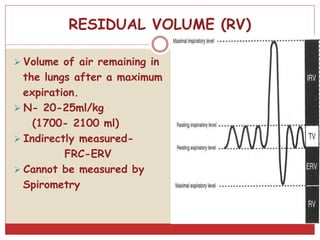
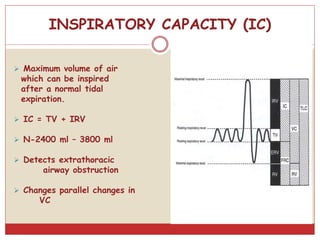
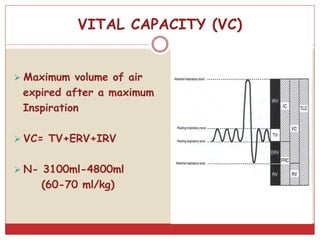
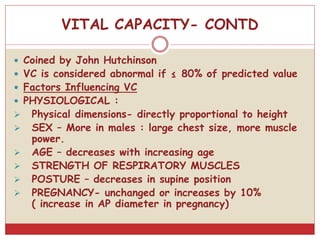
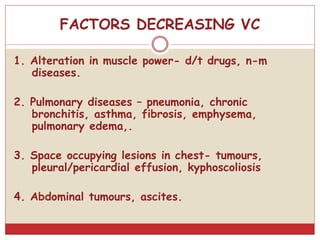
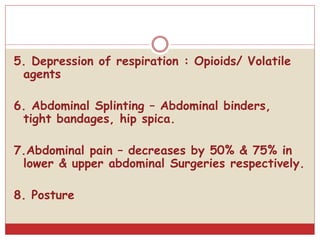
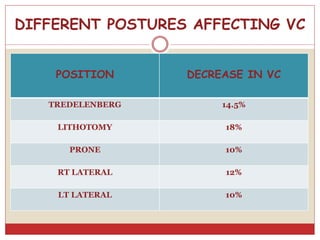
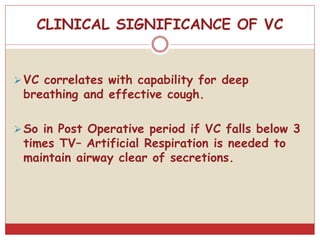
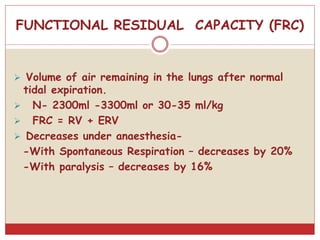
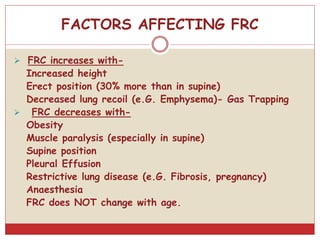
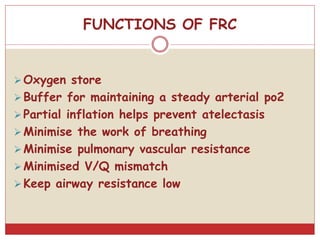
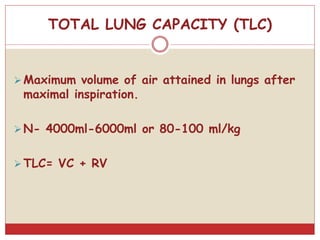
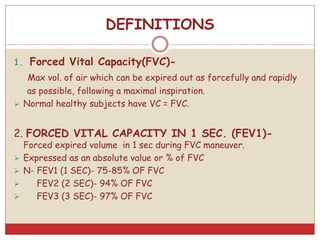
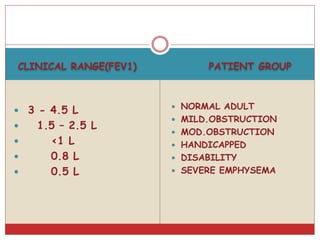
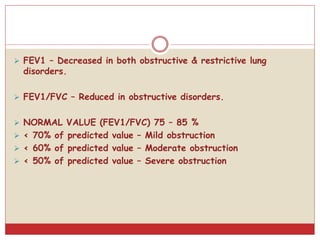
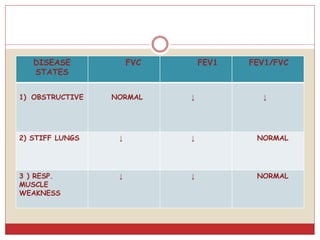
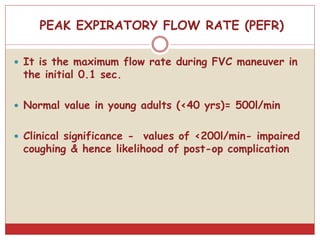
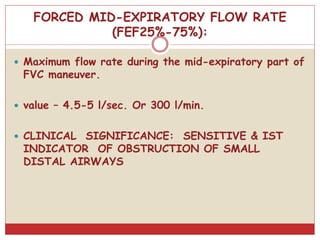
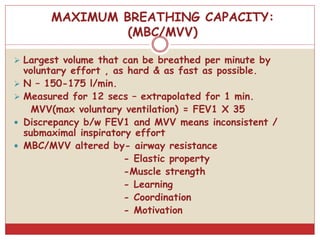
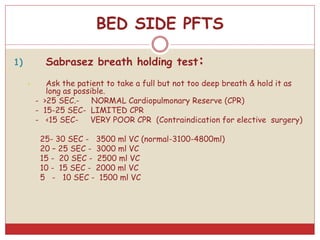
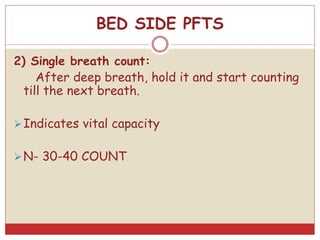
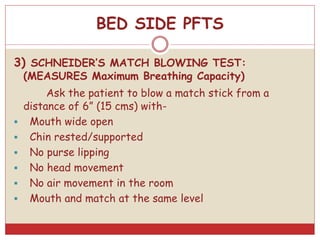
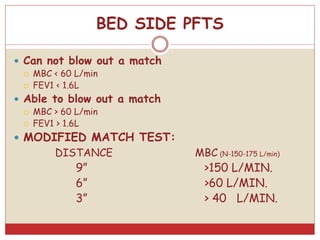
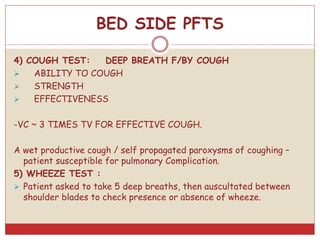
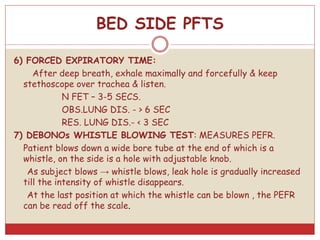
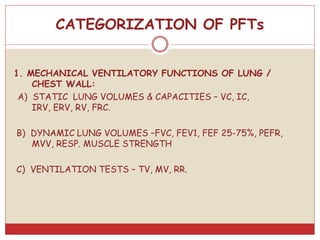
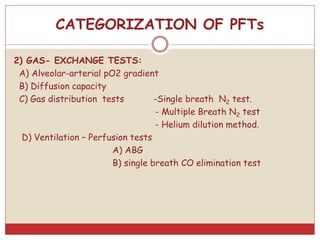
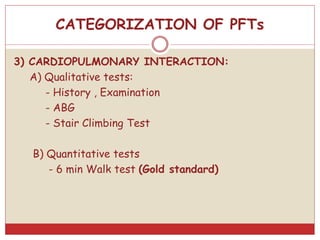
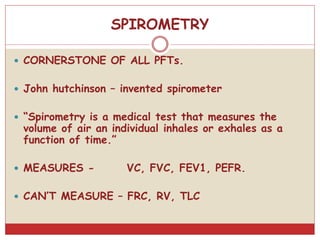
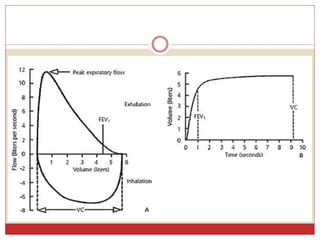
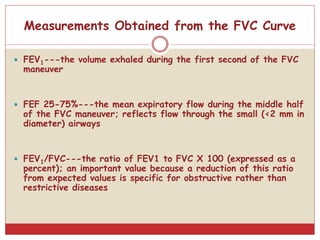
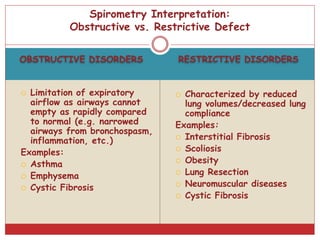
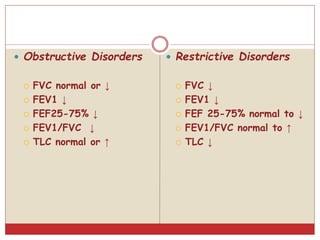
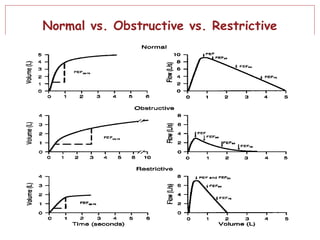
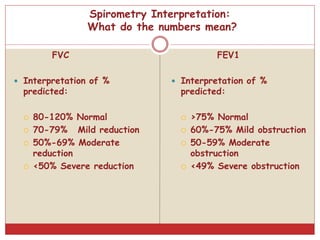
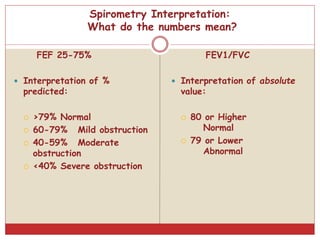
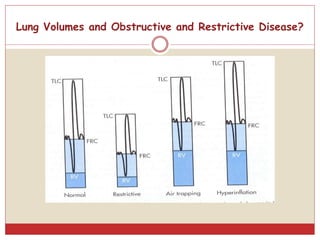
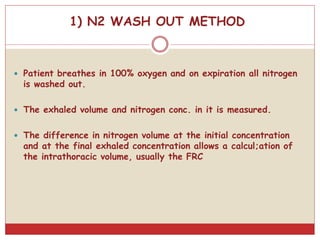
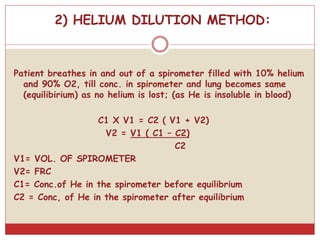
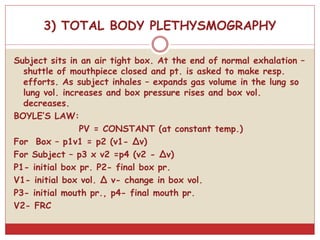
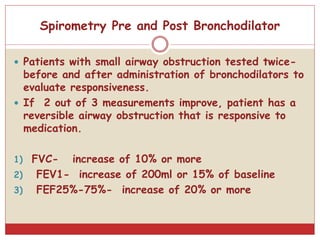
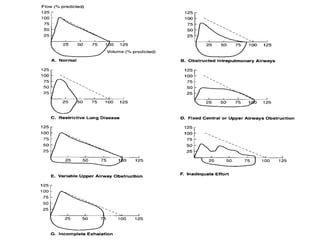
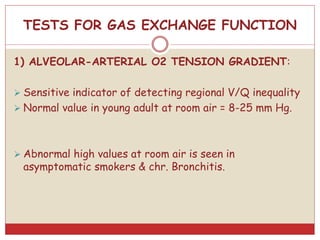
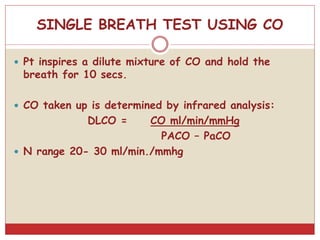
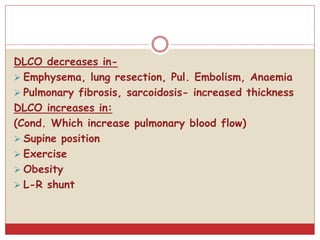
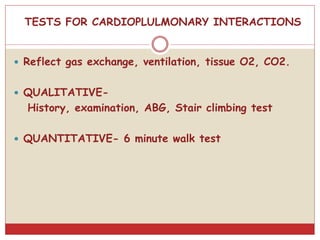
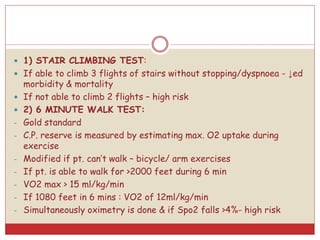
This document provides information on pulmonary function tests (PFTs). It discusses the goals of PFTs which include predicting and assessing pulmonary dysfunction. It outlines various lung volumes and capacities that can be measured through PFTs such as tidal volume, vital capacity, and total lung capacity. The document also discusses indications for preoperative PFTs and provides guidelines from different organizations. It summarizes different PFT measurements and their clinical significance. Overall, the document serves as a guide for understanding PFTs and their role in evaluating pulmonary function and perioperative risk.