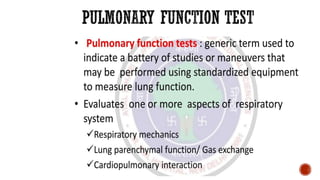
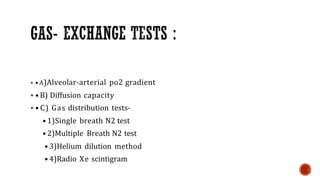
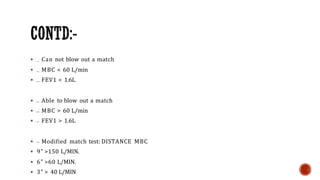
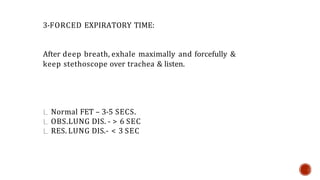
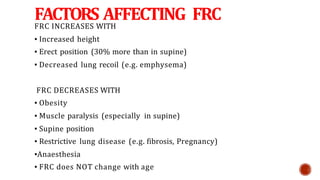
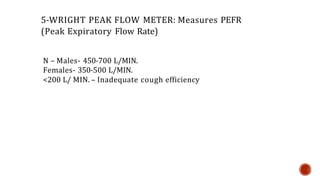
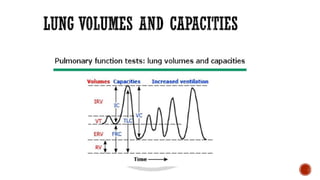
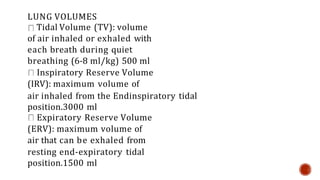
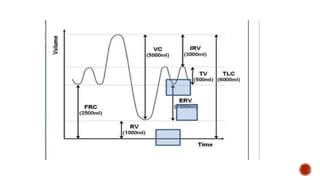
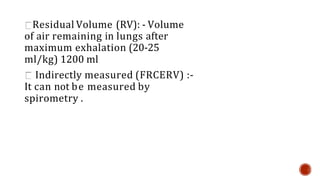
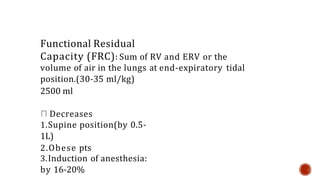
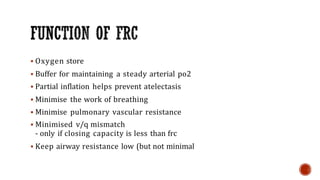
This document provides guidelines for ordering preoperative pulmonary function tests and describes various tests used to evaluate pulmonary function. It recommends ordering PFTs for patients over 70, obese patients, or those undergoing thoracic, upper abdominal, or lung surgery. Accepted PFTs include tests of static and dynamic lung volumes, diffusion capacity, and gas distribution. Bedside tests like breath-holding, forced expiratory time, peak flow, and pulse oximetry can also provide useful information. PFT tracings show lung volumes and capacities, and factors that impact the functional residual capacity are described.