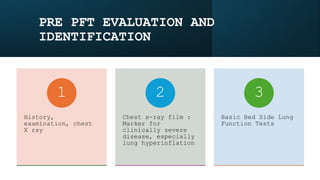
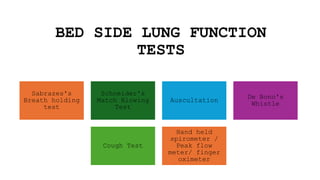
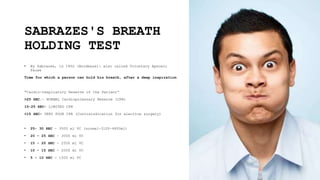
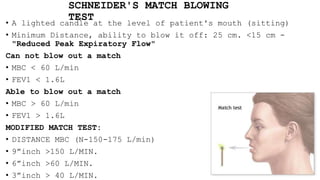
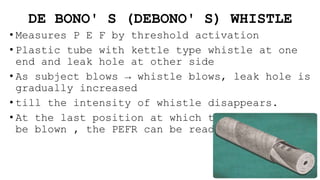
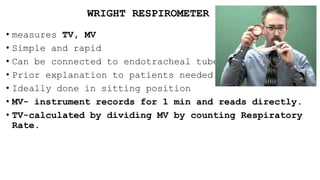
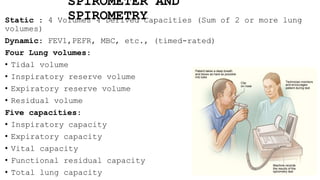
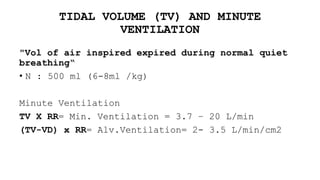
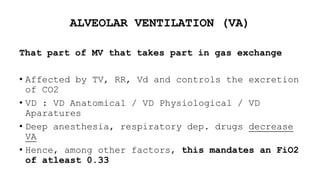
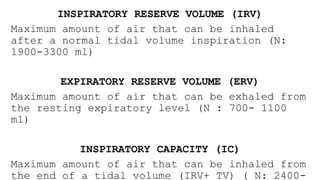
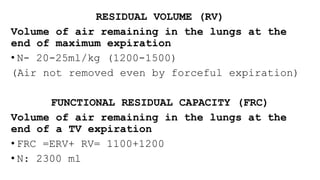
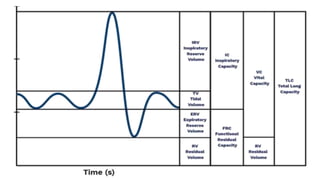
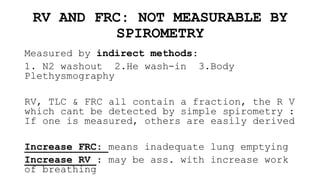
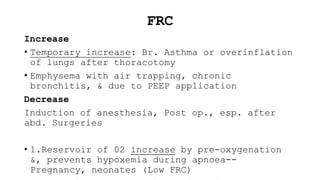
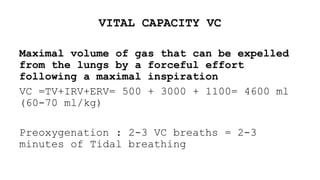
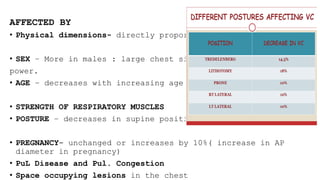
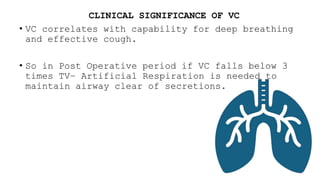
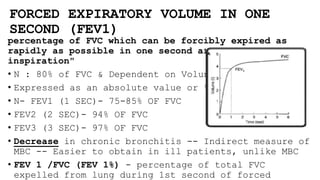
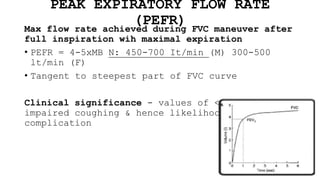
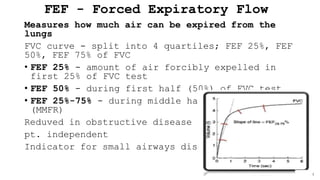
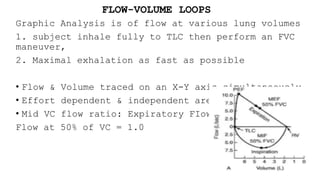
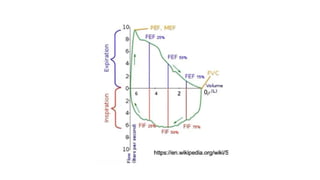
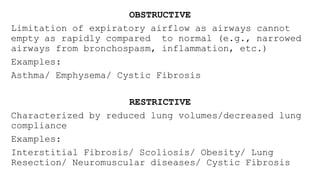
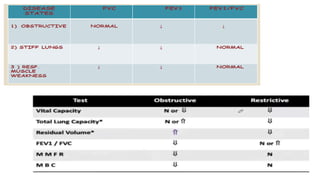
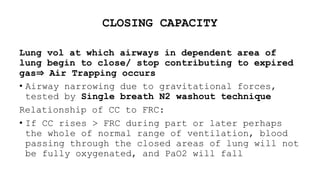
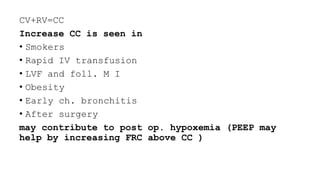
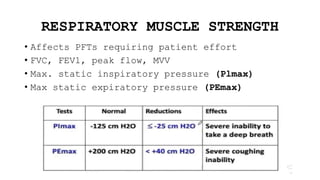
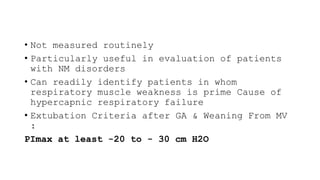
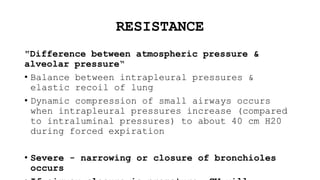
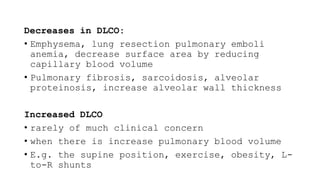
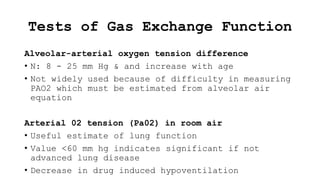
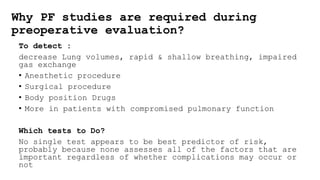
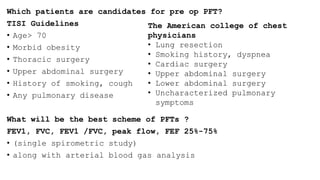
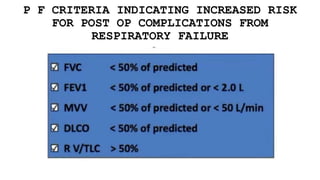
The document outlines the indications for pulmonary function tests (PFTs) which include diagnosing lung diseases, assessing treatment responses, and evaluating surgical risks. It details methods for testing lung capacity and ventilation, such as spirometry and peak flow measurements, along with their clinical significance in determining respiratory health. Additionally, it highlights contraindications for PFTs and criteria for selecting patients who may benefit from these evaluations preoperatively.