This document discusses various ventilatory strategies for treating ALI/ARDS, including:
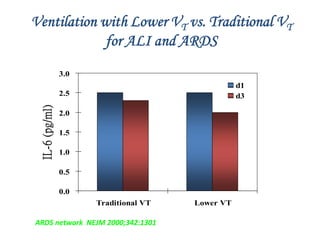
- Using low tidal volumes (6 ml/kg) instead of conventional volumes to decrease mortality.
- Using PEEP to recruit collapsed lung units and prevent atelectrauma.
- Pressure-controlled ventilation to limit peak pressures while maintaining oxygenation.
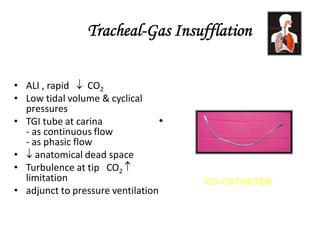
- Permissive hypercapnia to decrease lung injury even if it increases CO2 levels.
- Prone positioning and recruitment maneuvers to improve oxygenation by opening collapsed alveoli.
- High frequency ventilation and airway pressure release ventilation as rescue therapies.