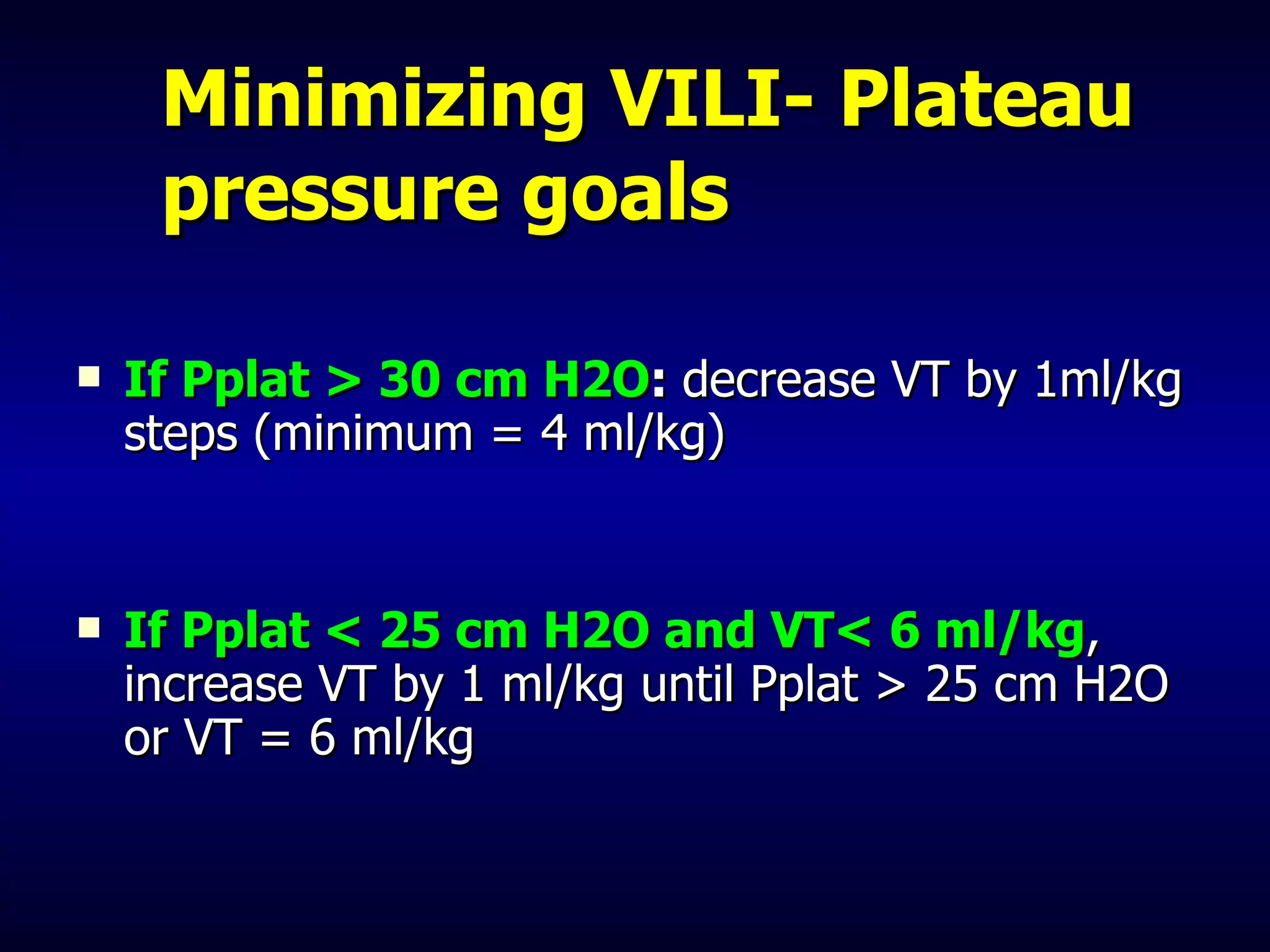
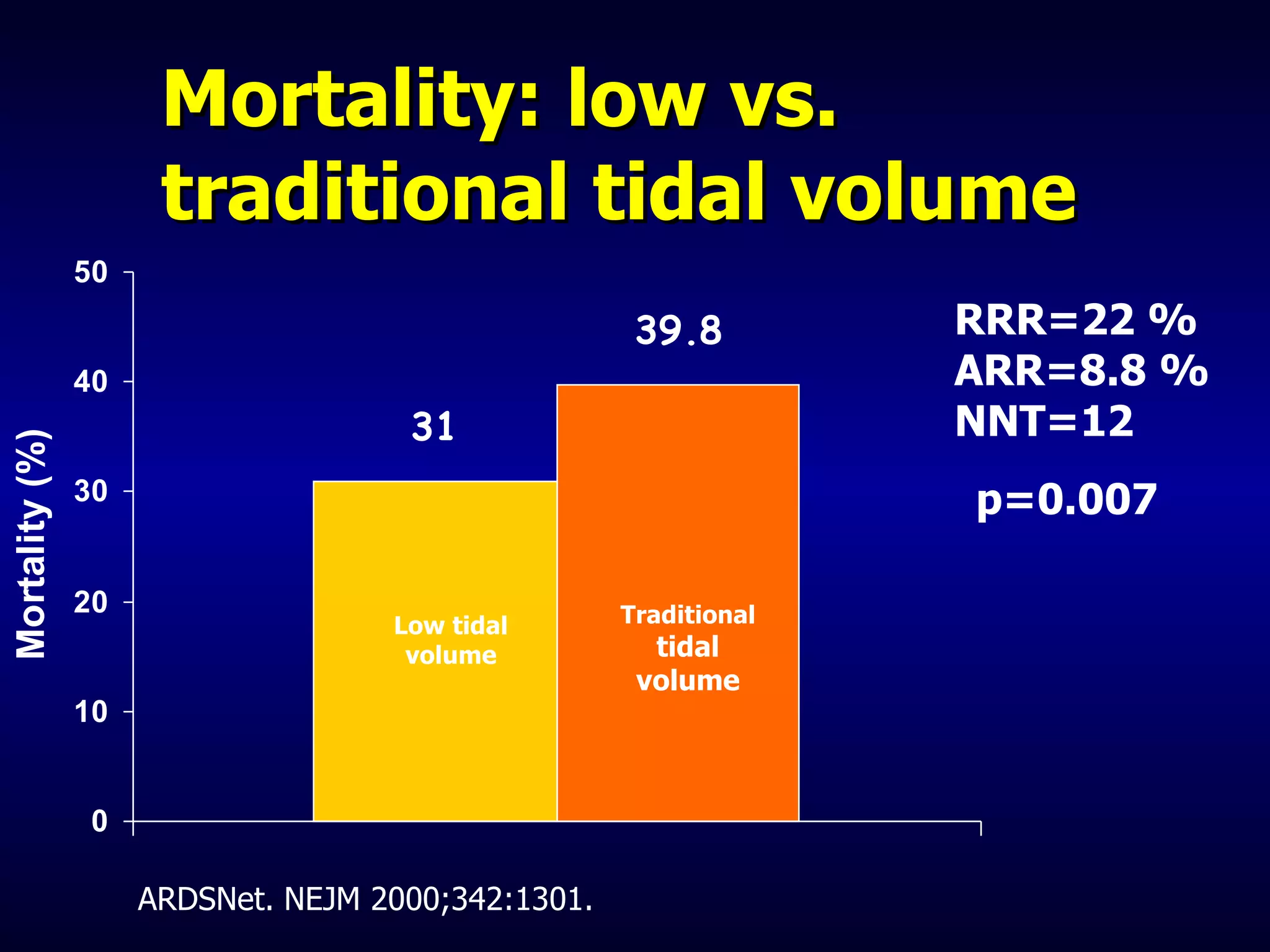
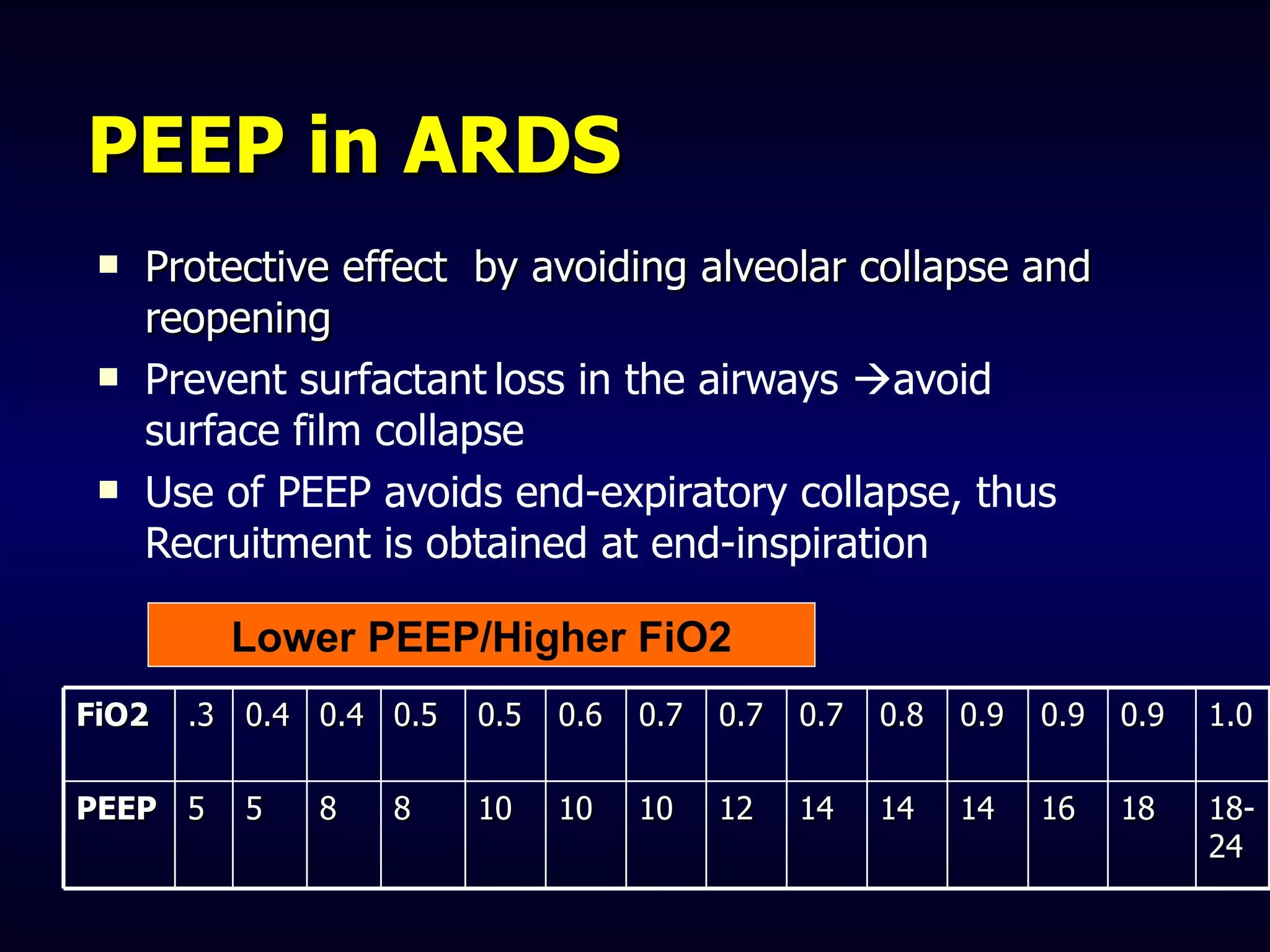
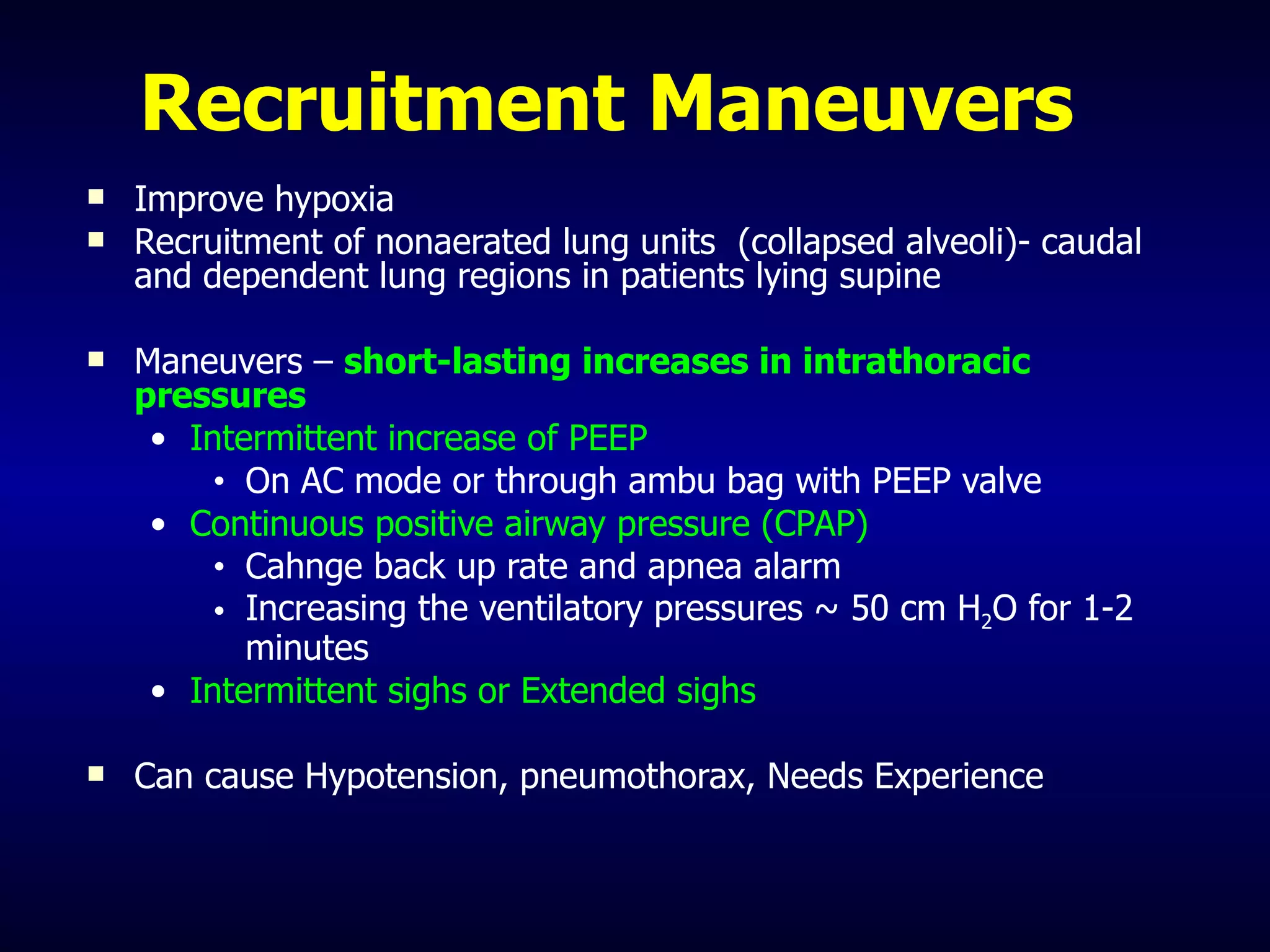
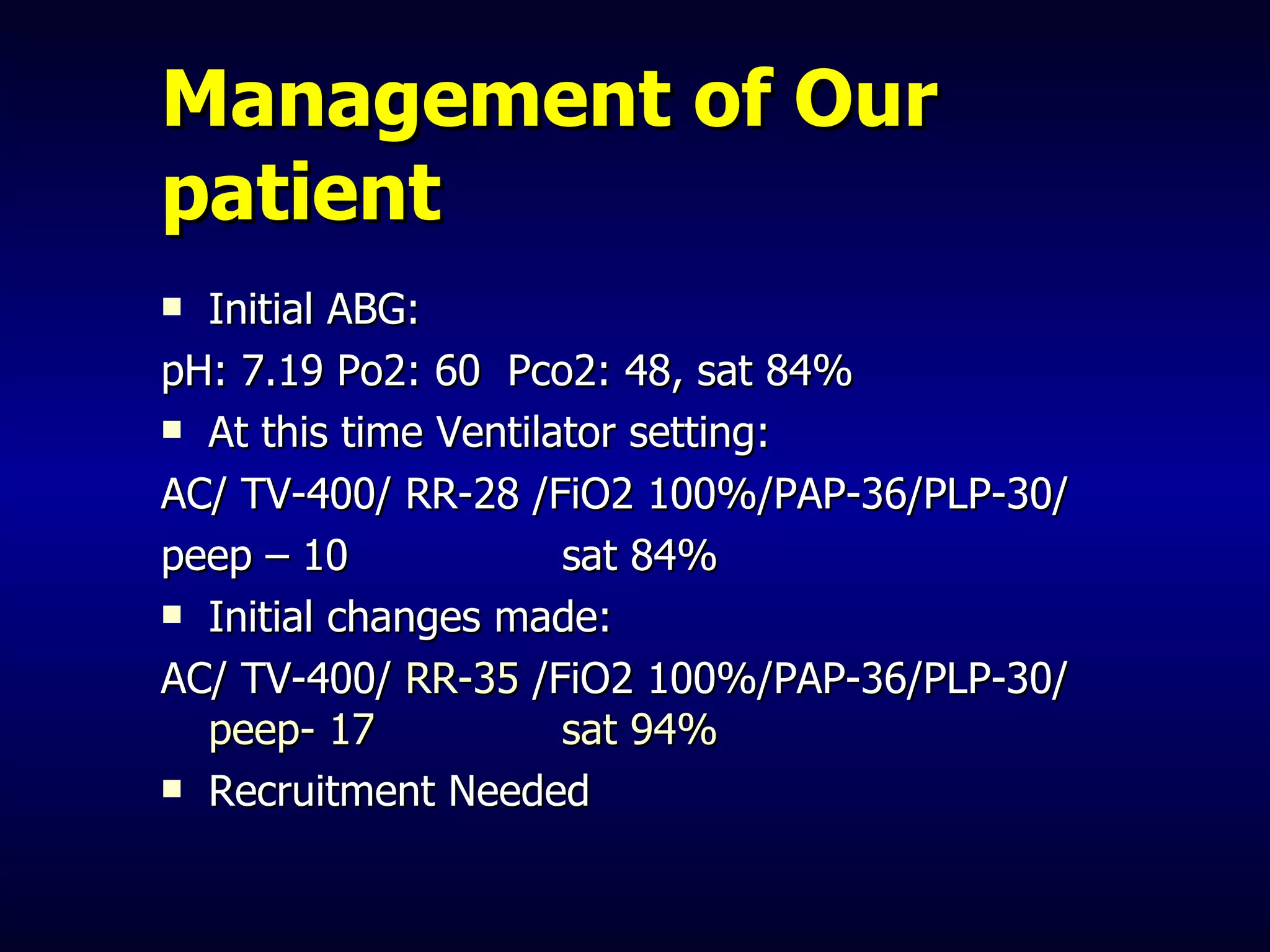
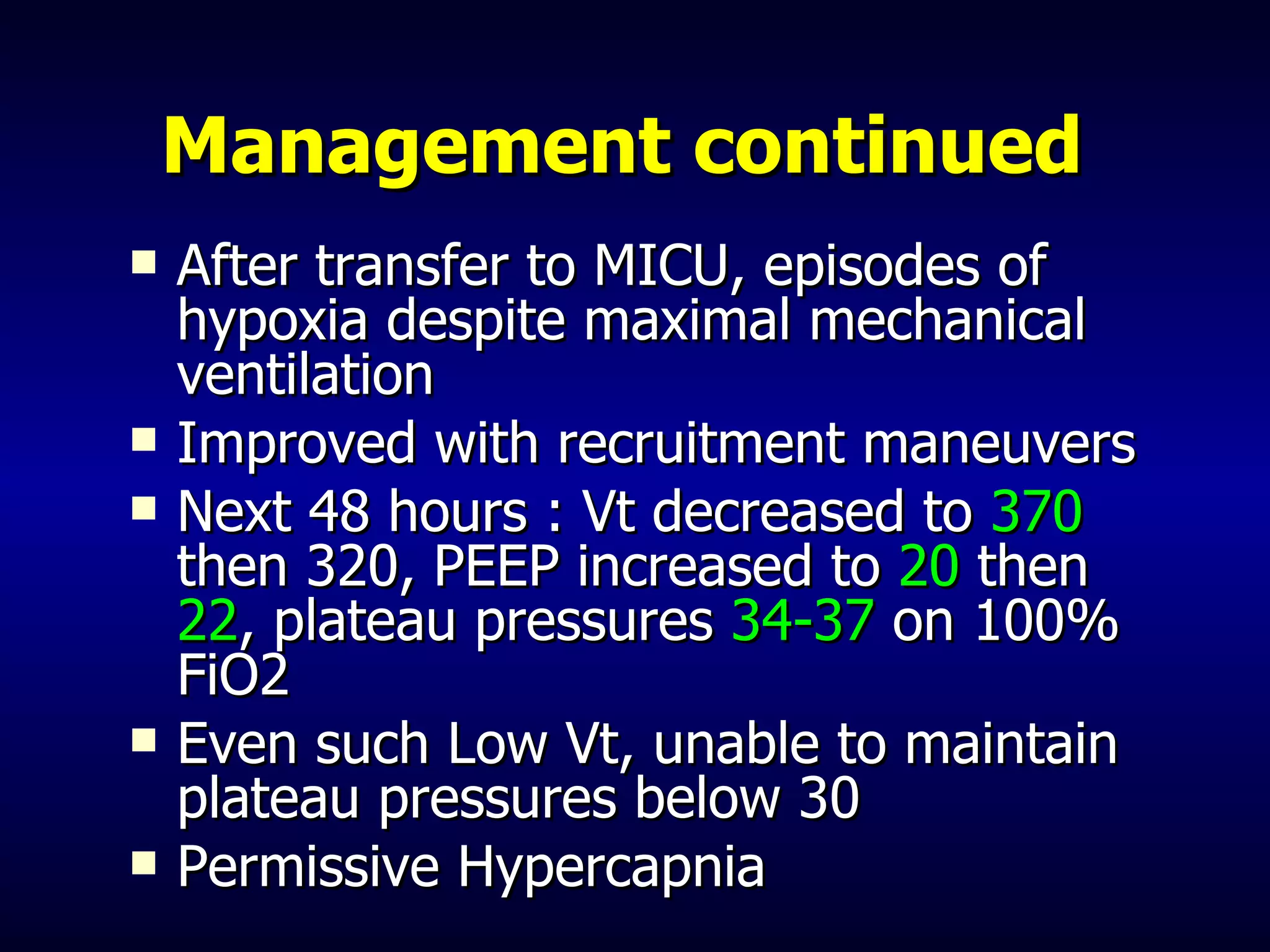
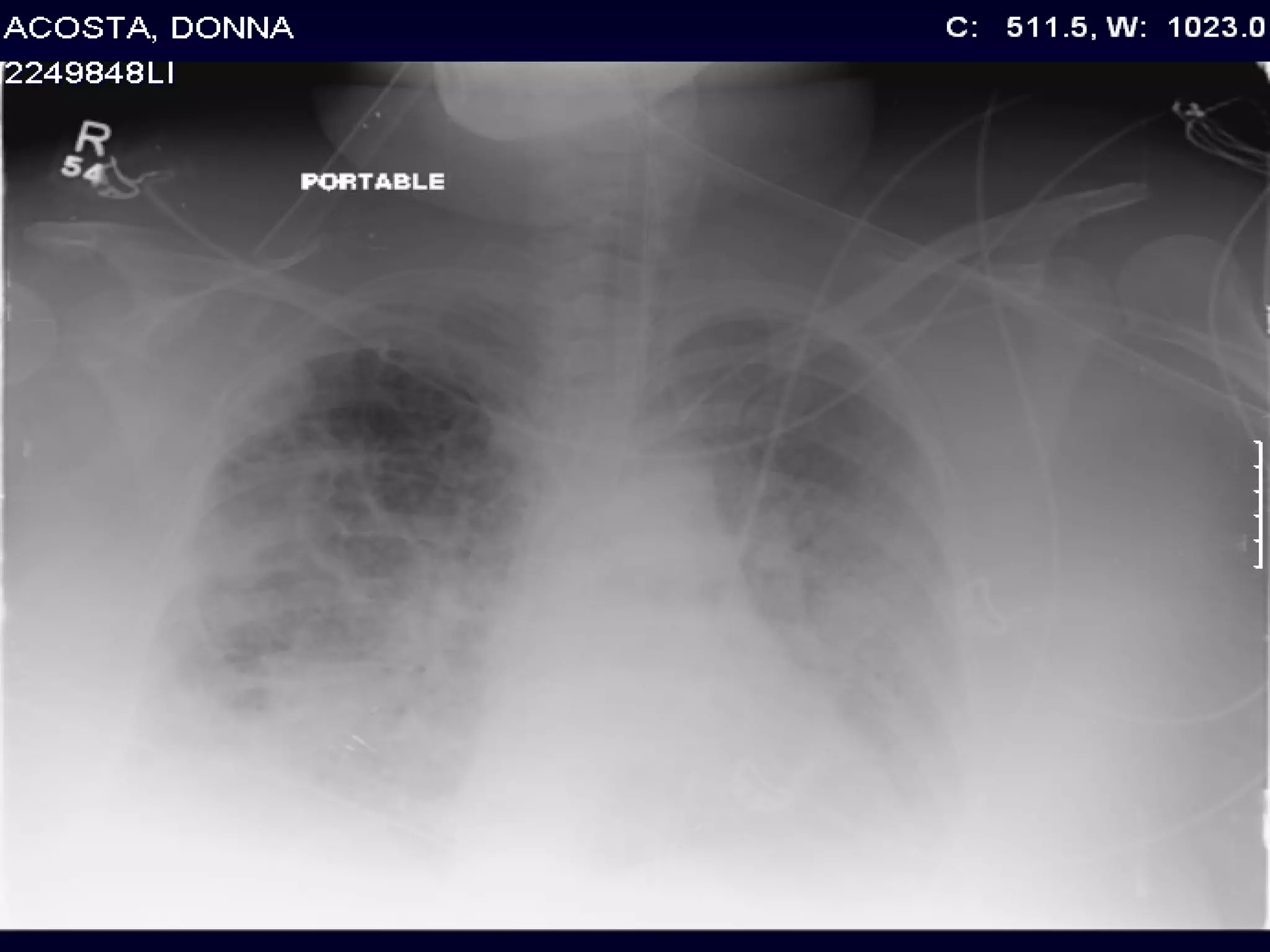
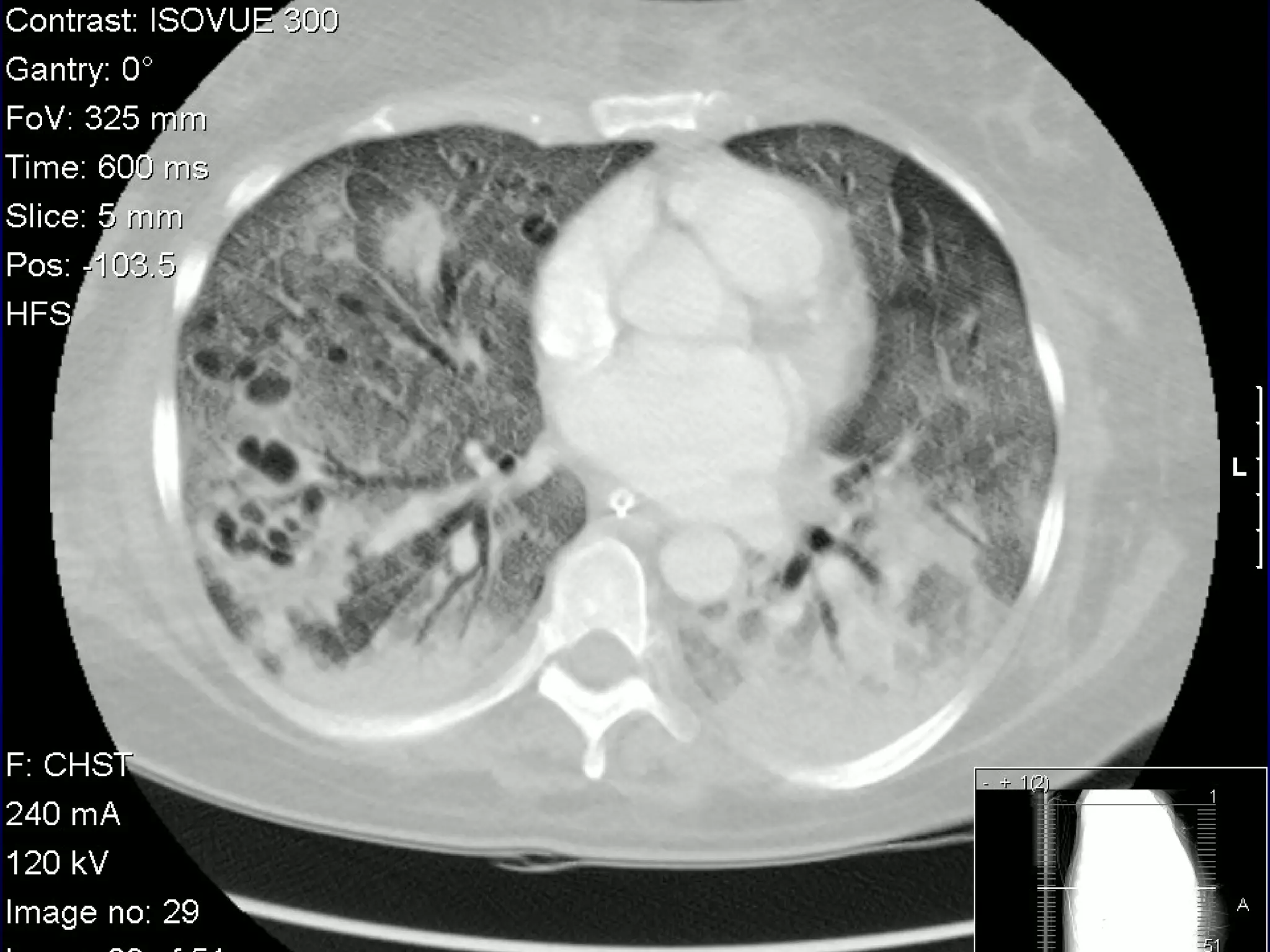
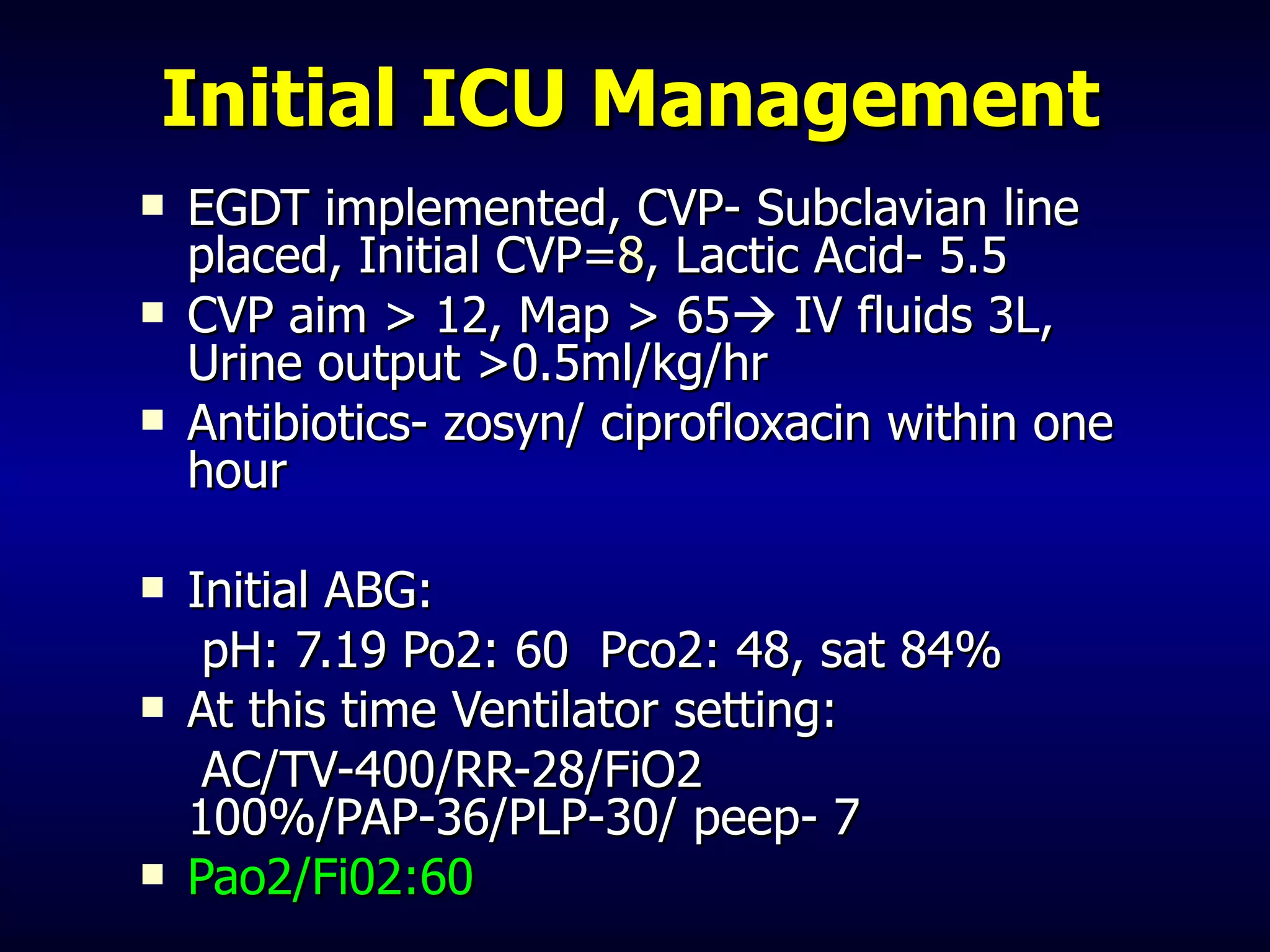
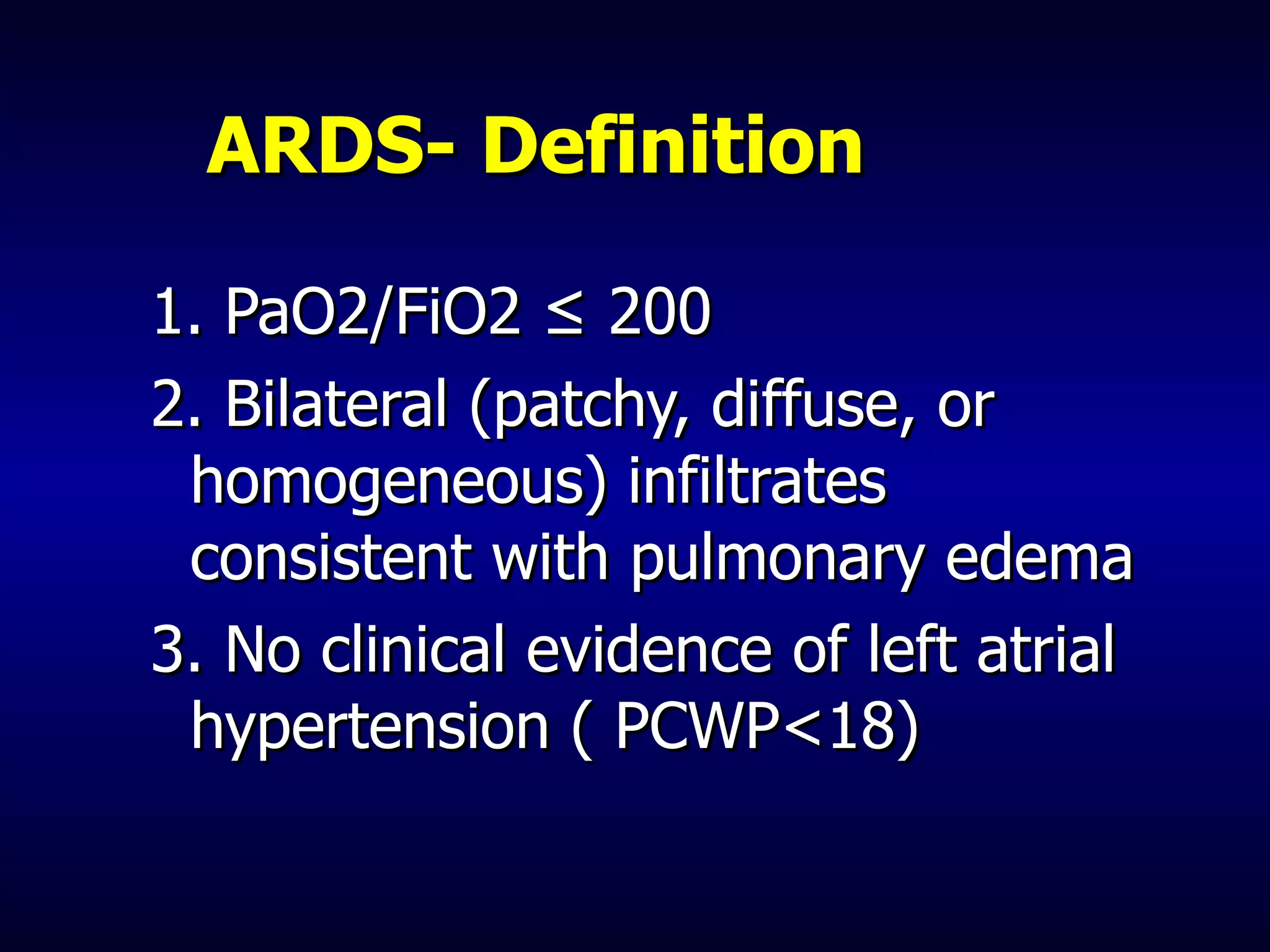
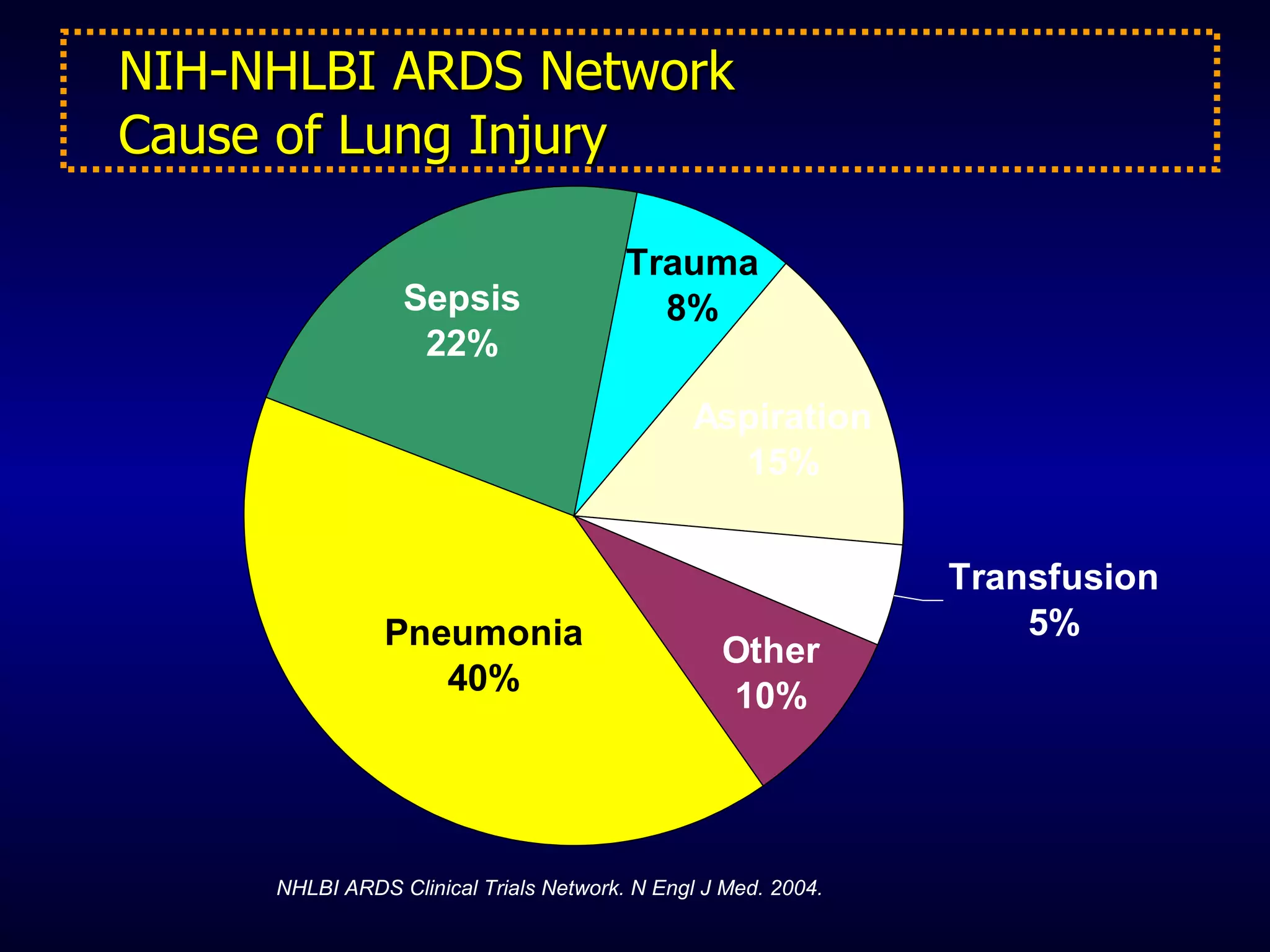
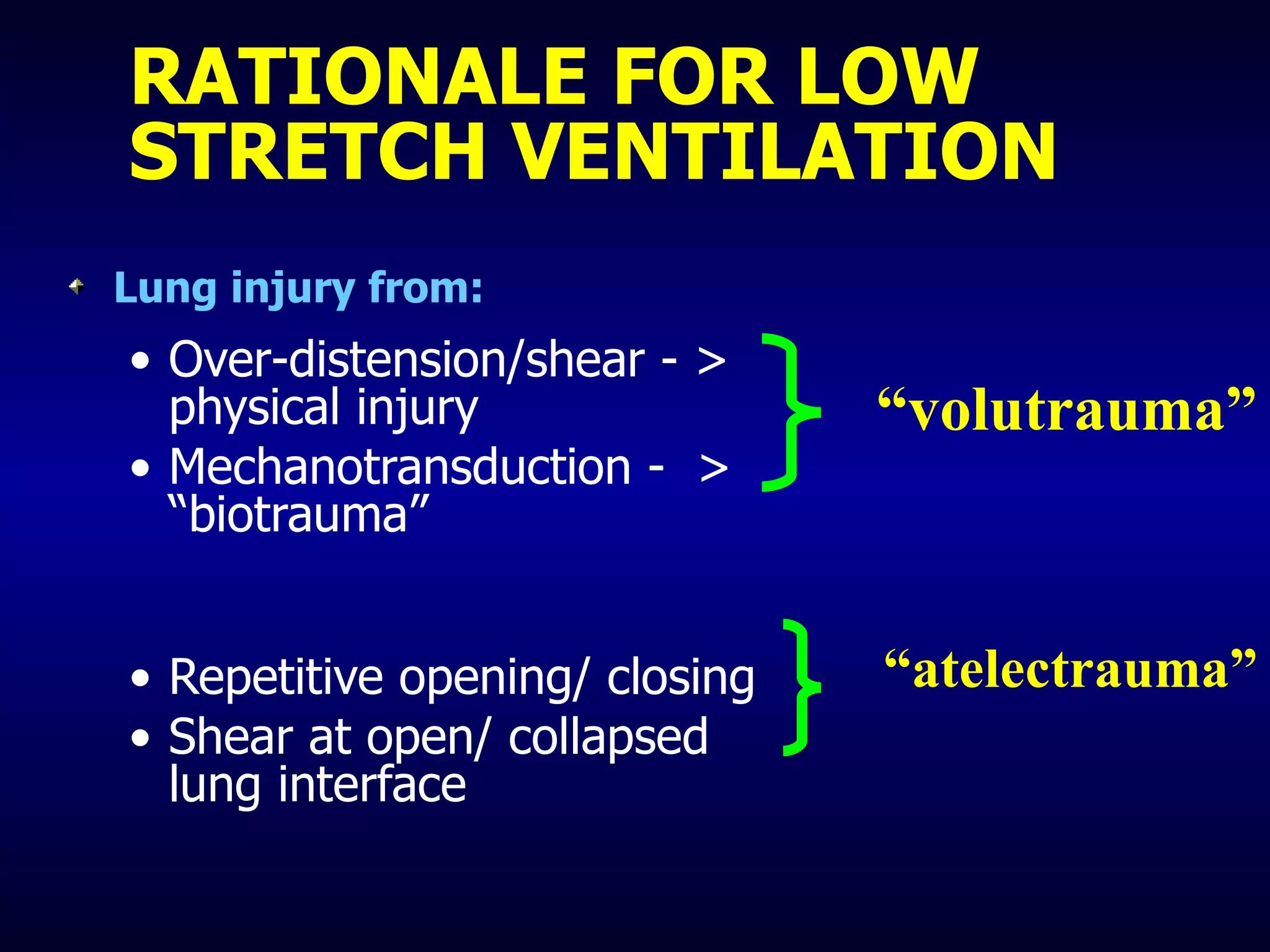
This document discusses ventilation strategies for a patient with acute respiratory distress syndrome (ARDS). It provides details of the patient's initial presentation and management, including mechanical ventilation settings. It describes the rationale for using low tidal volume ventilation to minimize ventilator-induced lung injury. The patient required aggressive management for sepsis and hypoxemia including recruitment maneuvers and increasing PEEP and mean airway pressures. Despite these efforts, the patient could not be weaned from high FiO2 and developed multi-organ failure and died. The document recommends using low tidal volumes, limiting end-inspiratory pressures, adequate PEEP, and considering recruitment maneuvers to optimize ventilation in ARDS.
![ARDSNET- Initial Ventilator Strategies Low Tidal Volume (6ml/kg) Calculate predicted body weight (PBW) Males = 50 + 2.3 [height (inches) – Females = 45.5 + 2.3 [height (inches) -60 ] Plateau Pressure < 30 cms](https://image.slidesharecdn.com/ventilationstrategiesinards-rachmale-100415230039-phpapp01/75/Ventilation-strategies-in-ards-rachmale-8-2048.jpg)