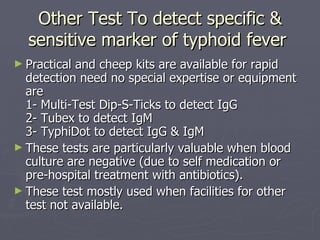
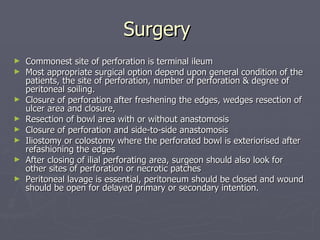
Typhoid fever is caused by the Salmonella typhi bacterium and is prevalent in developing countries, often linked to poor sanitation. Symptoms include persistent high fever, abdominal distension, and potential complications like bleeding and perforation of ulcers, confirmed by blood and stool cultures. Treatment involves fluid resuscitation, antibiotics, and possibly surgical intervention depending on the perforation's severity and location.