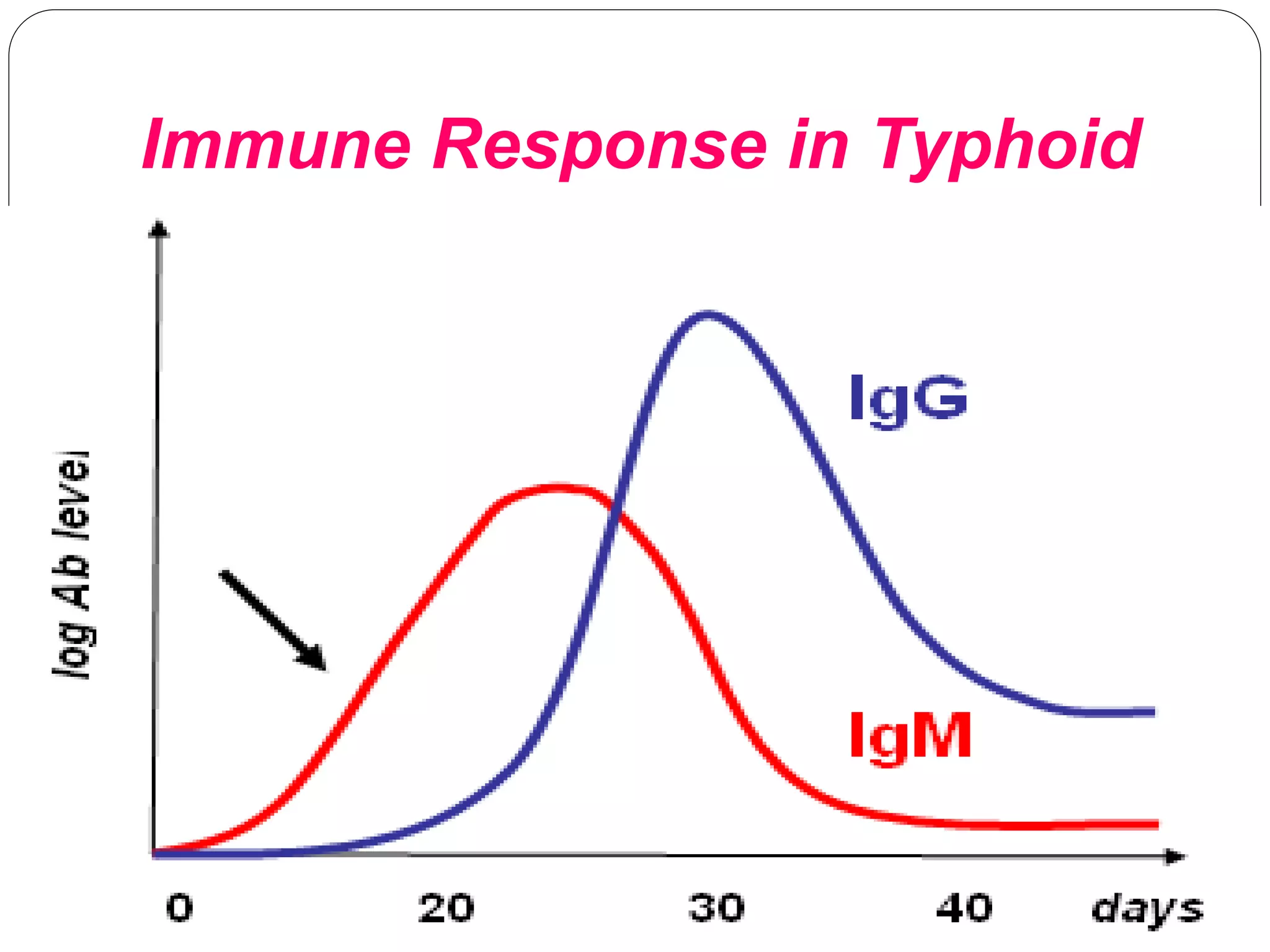
Enteric fever, primarily caused by Salmonella typhi, is a bacterial disease characterized by severe symptoms and potentially fatal complications. Historical milestones include the identification of the causative organism in the late 1800s and the development of serodiagnostic methods by 1896. Despite advancements in treatment and vaccination, typhoid fever remains a global public health concern with significant morbidity and mortality rates.