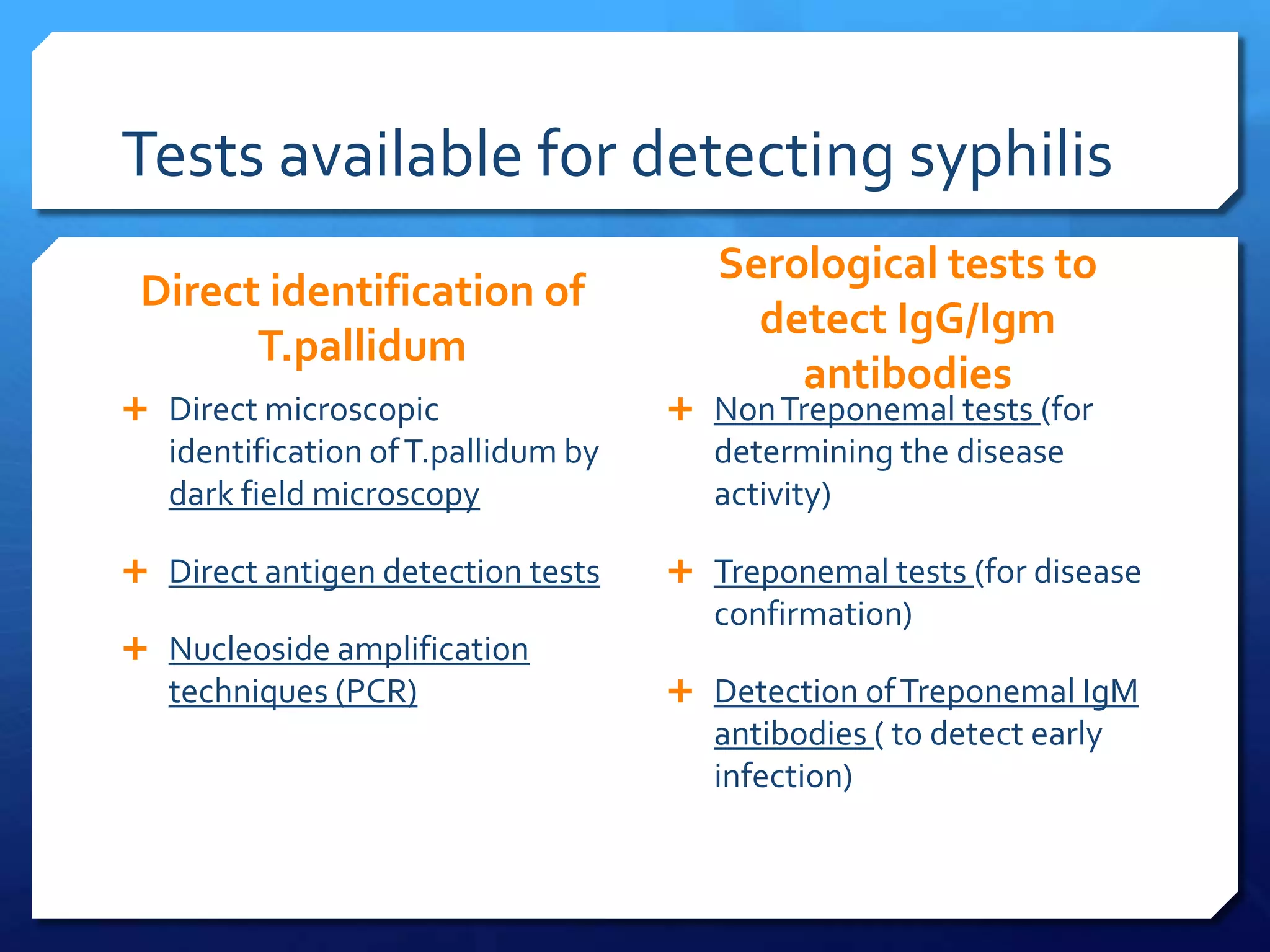
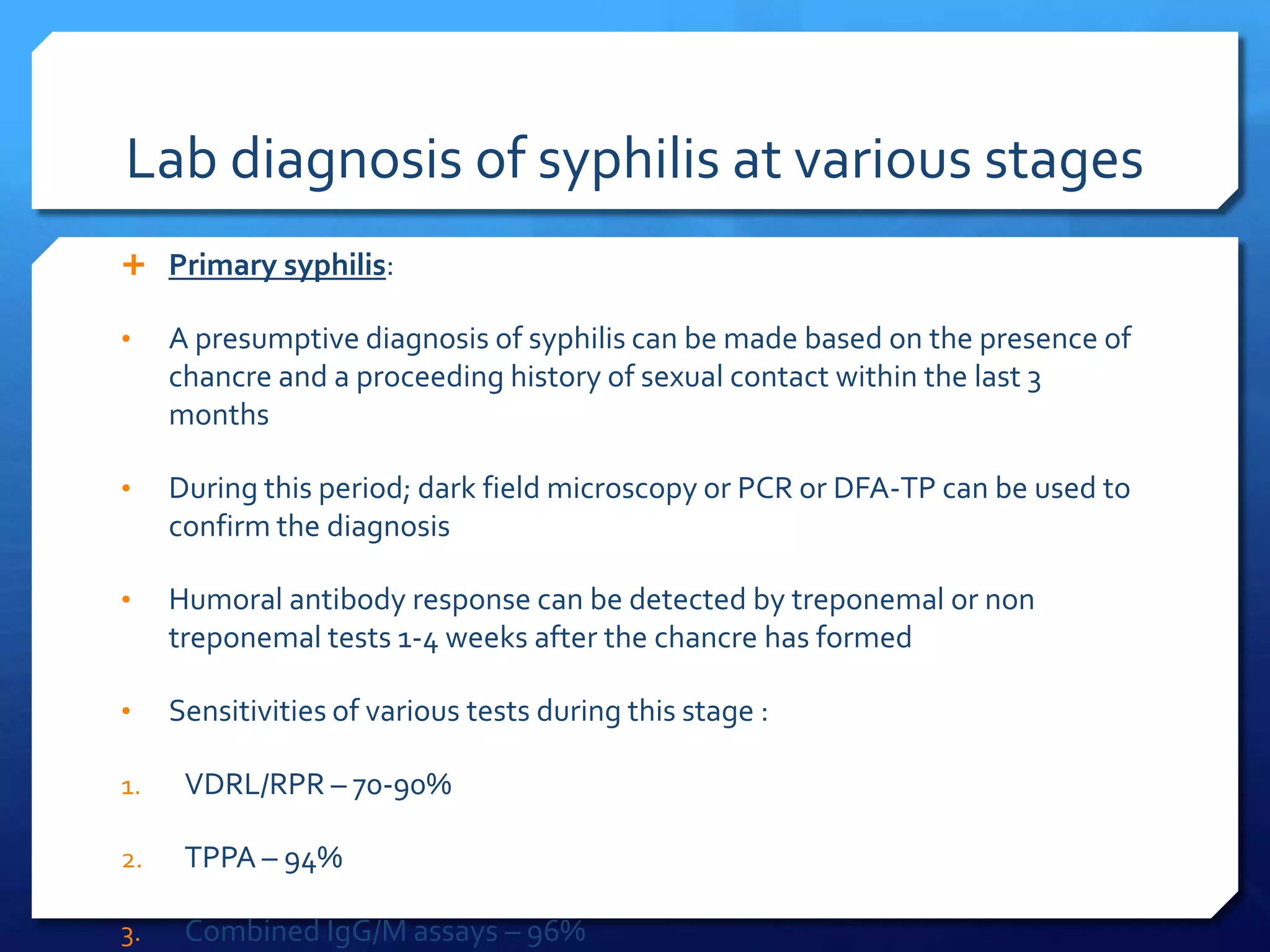
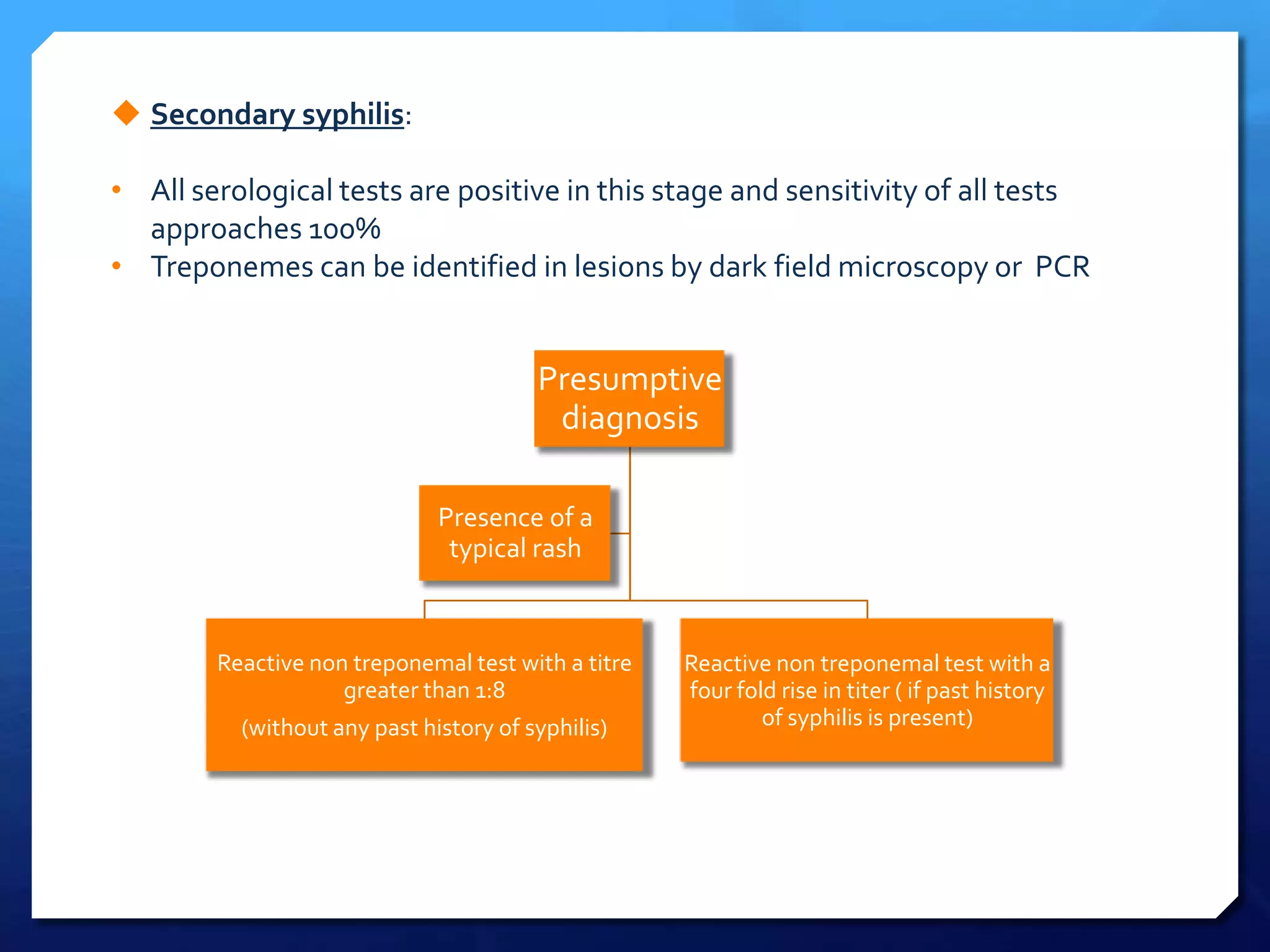
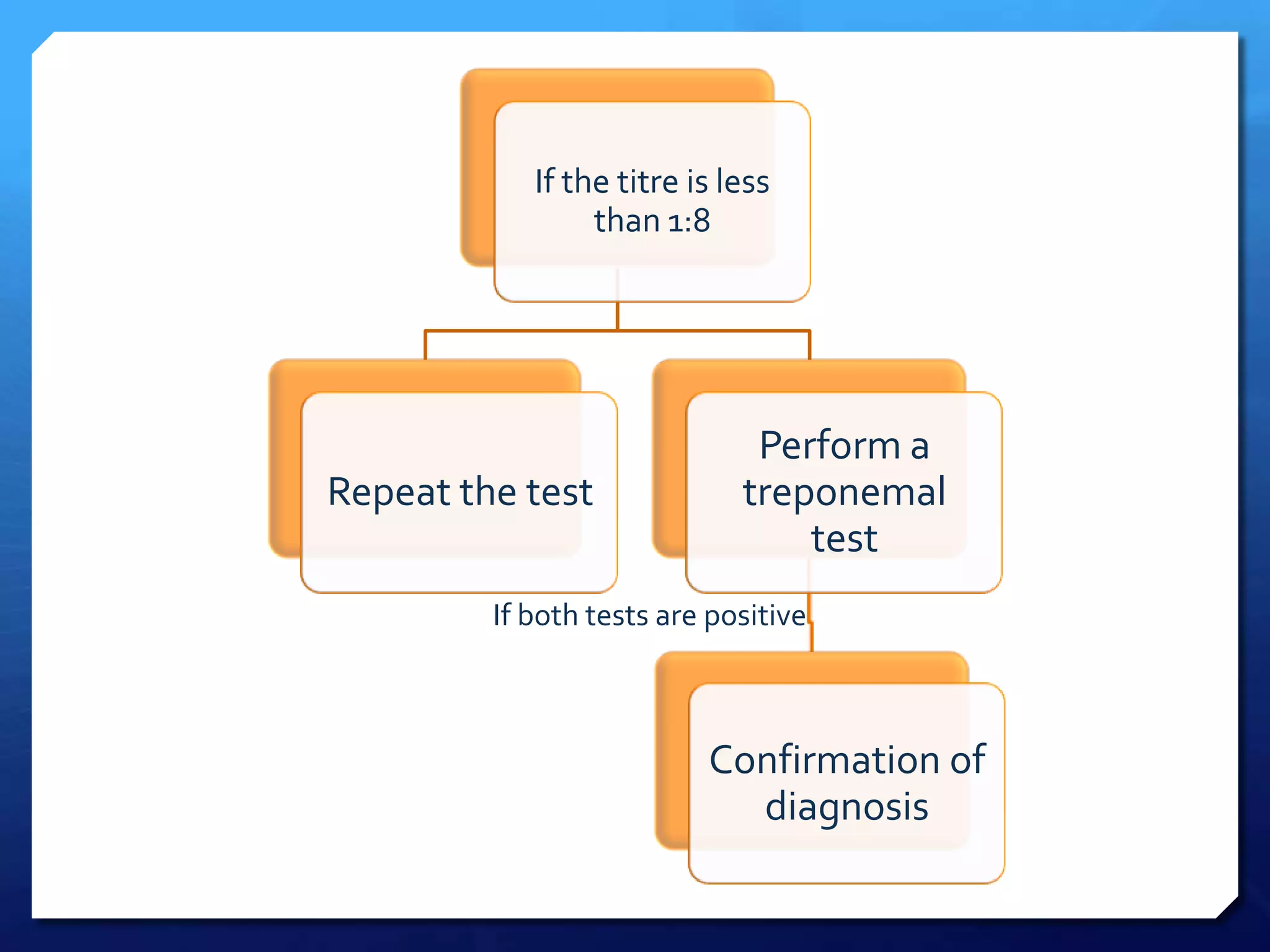
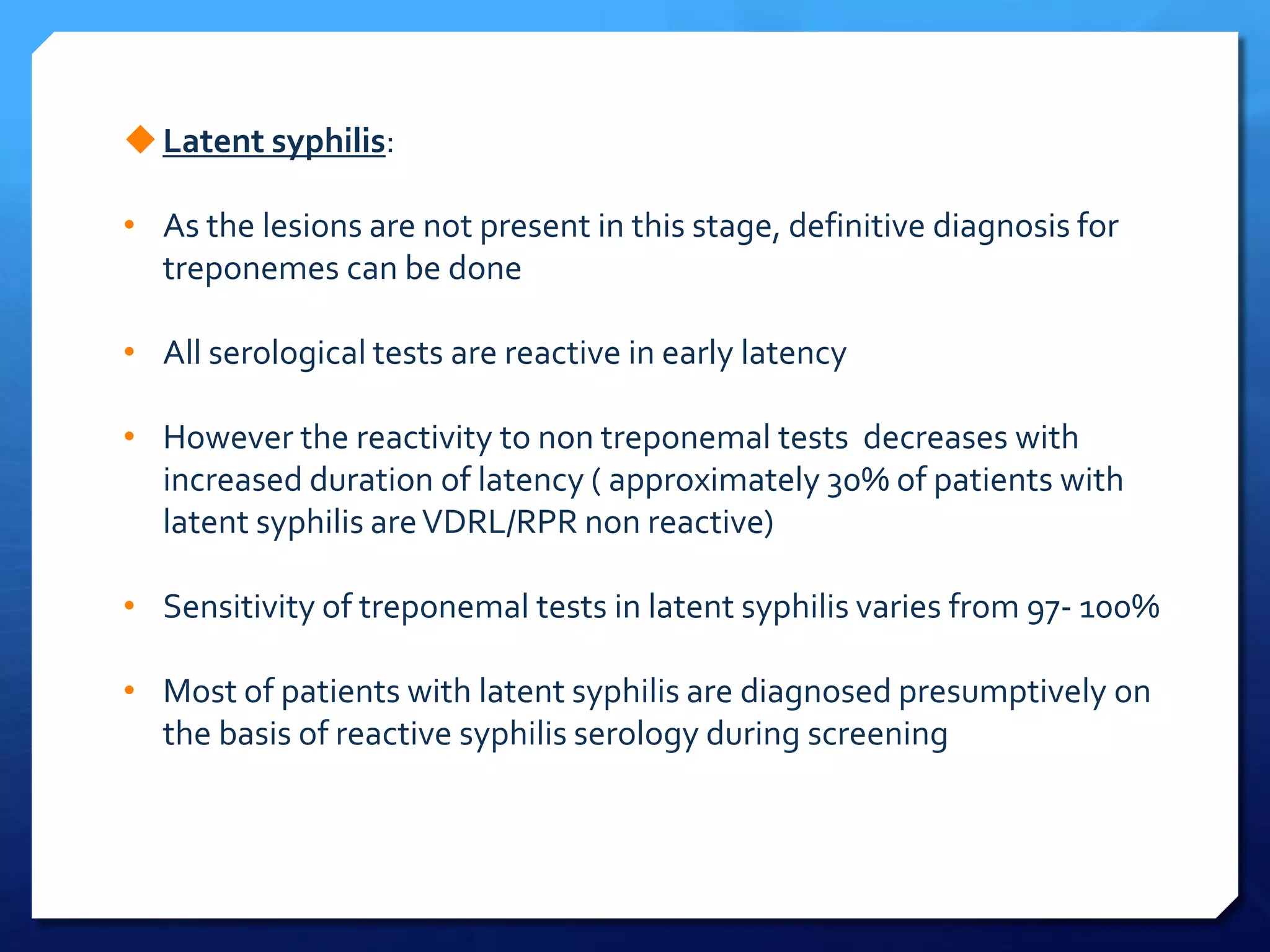
1. There are two main types of tests for diagnosing syphilis - direct tests that detect the bacteria Treponema pallidum, and indirect serological tests that detect antibodies produced in response to the infection.
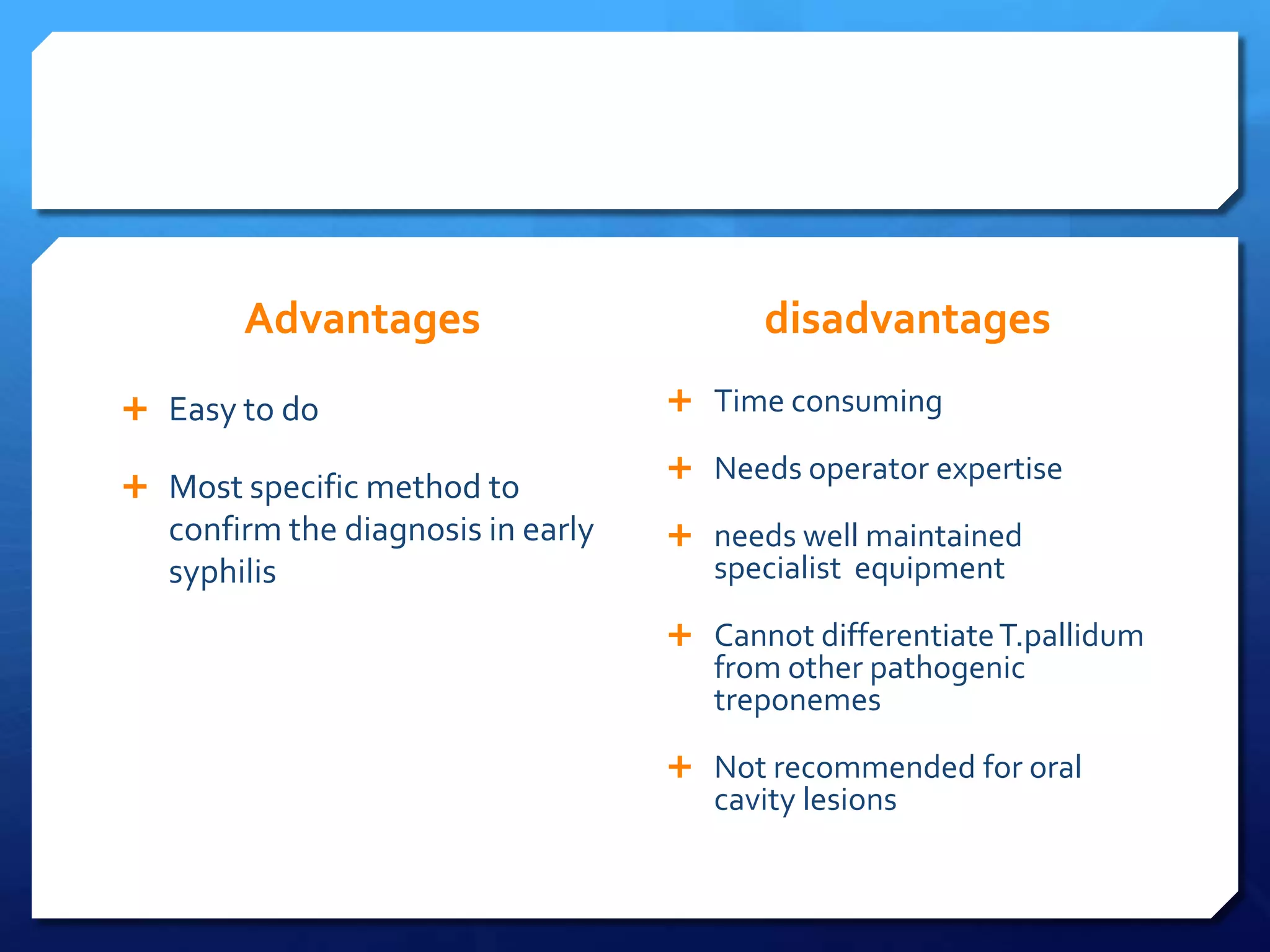
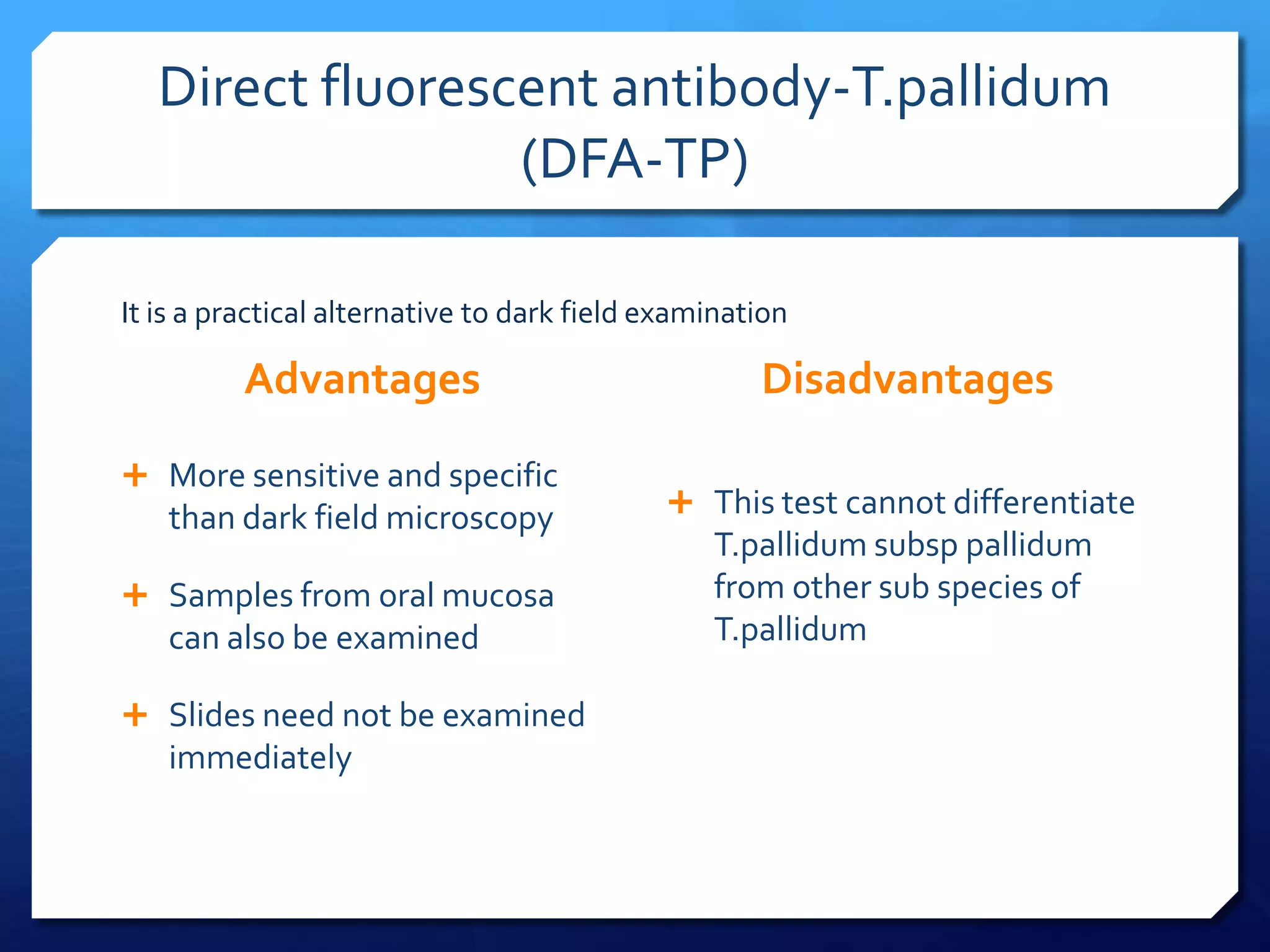
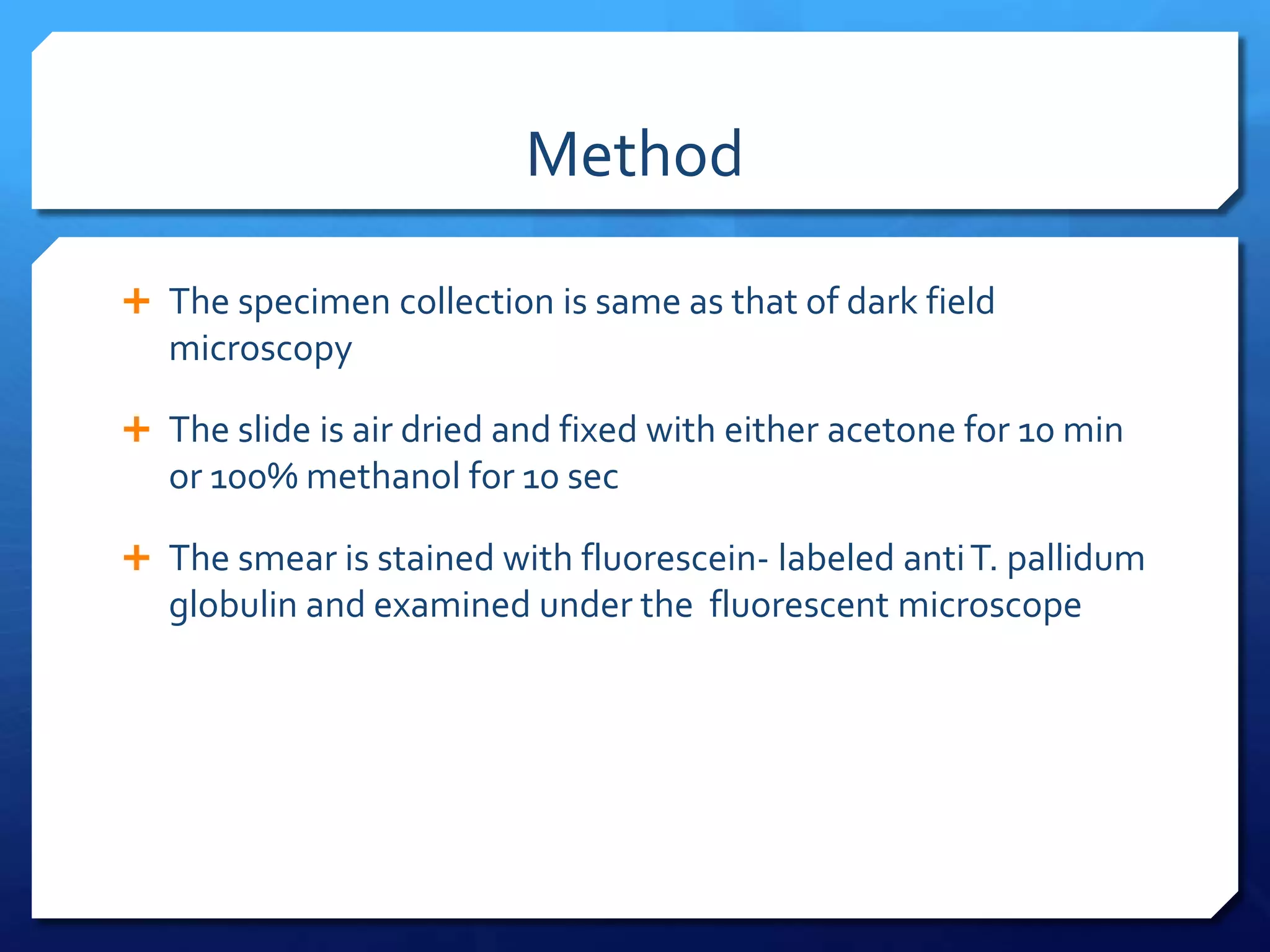
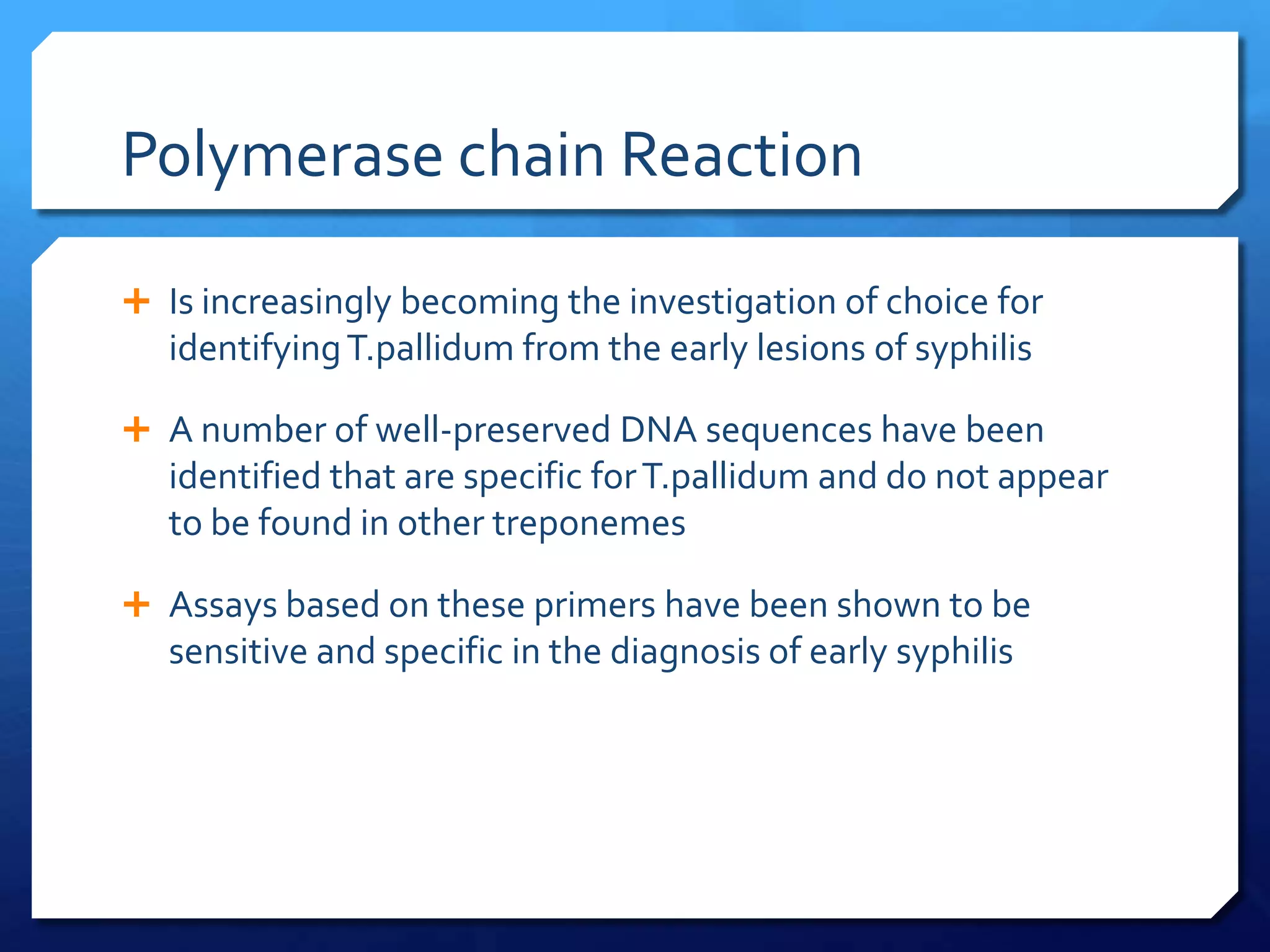
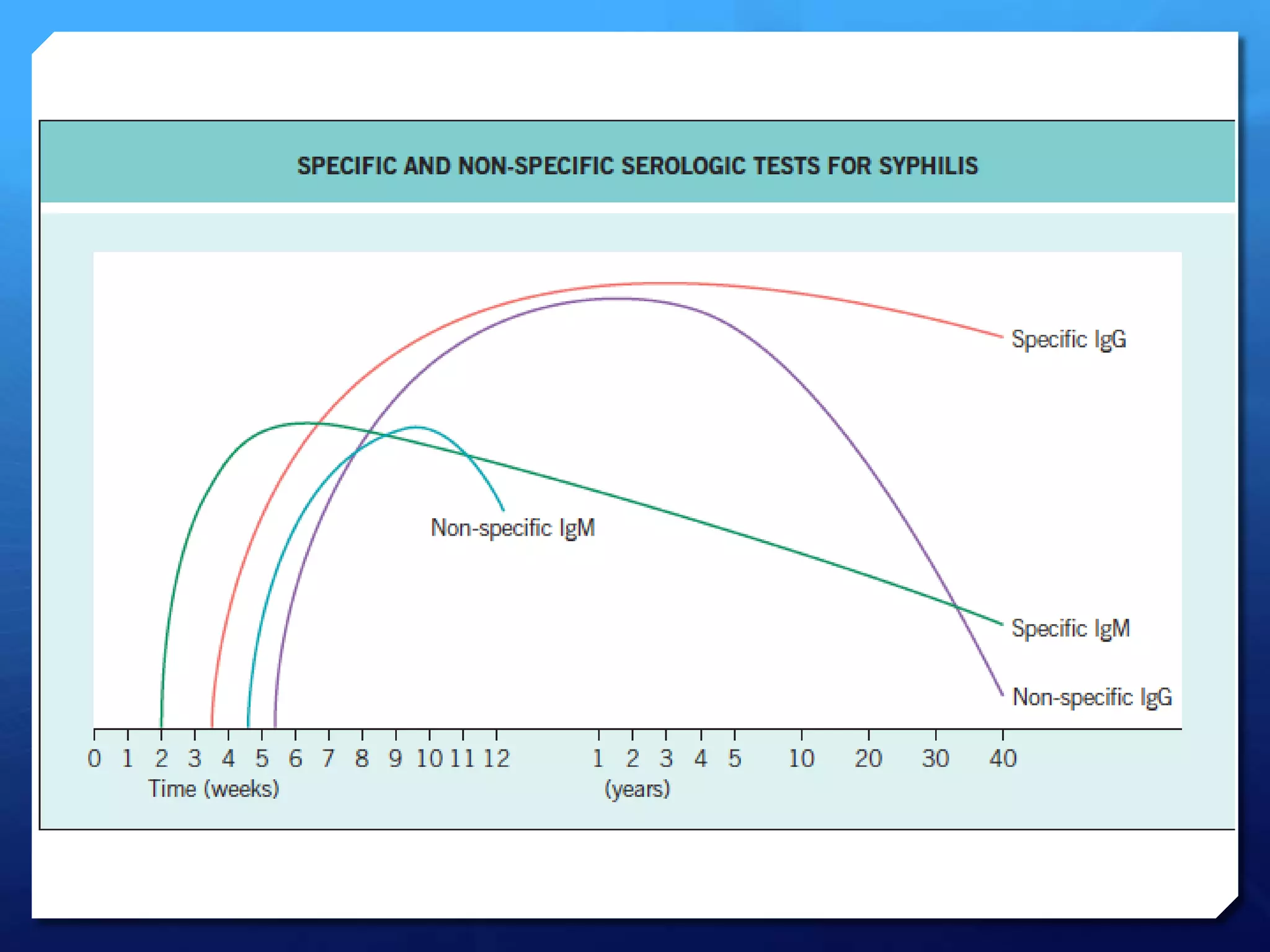
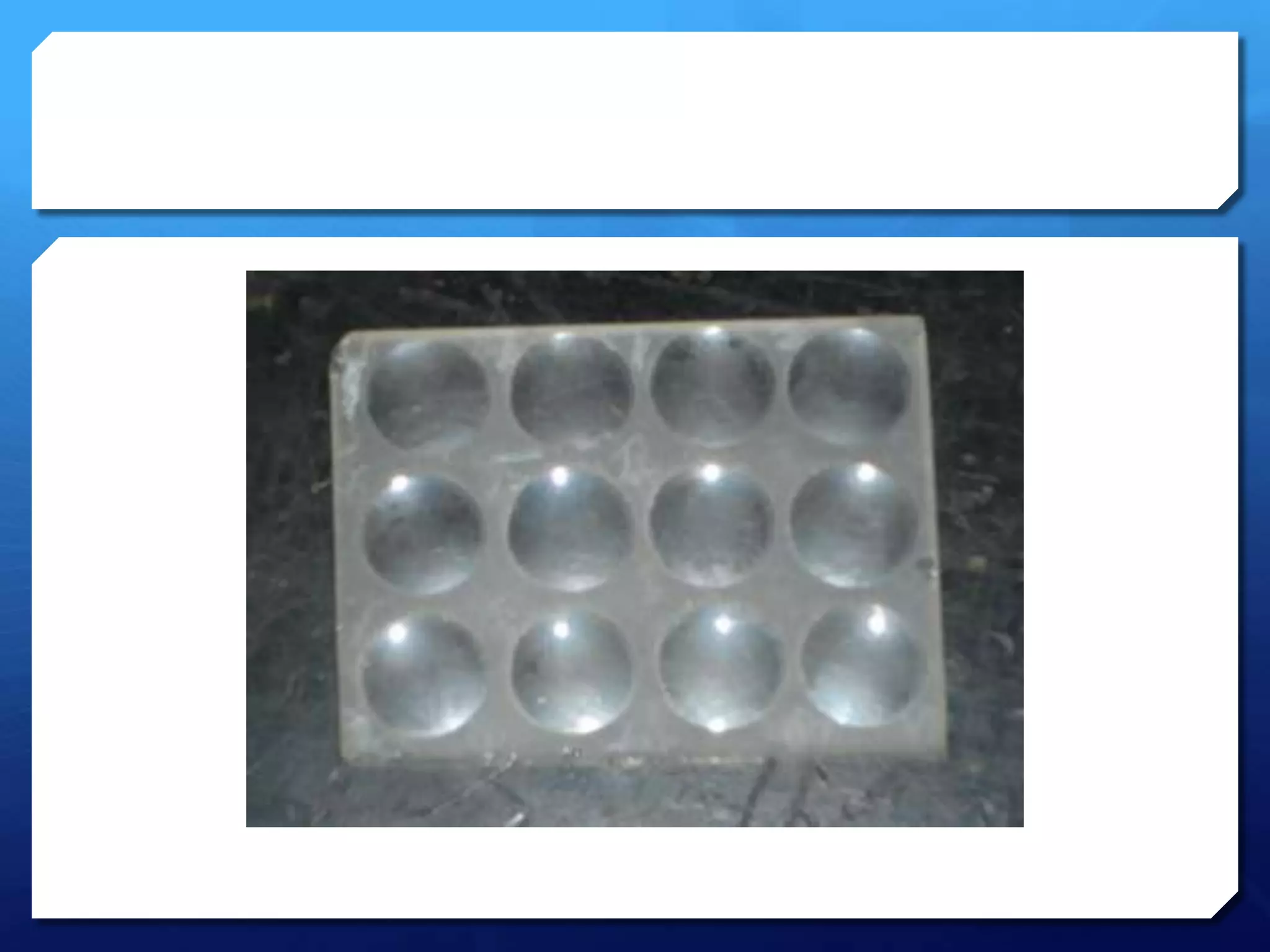
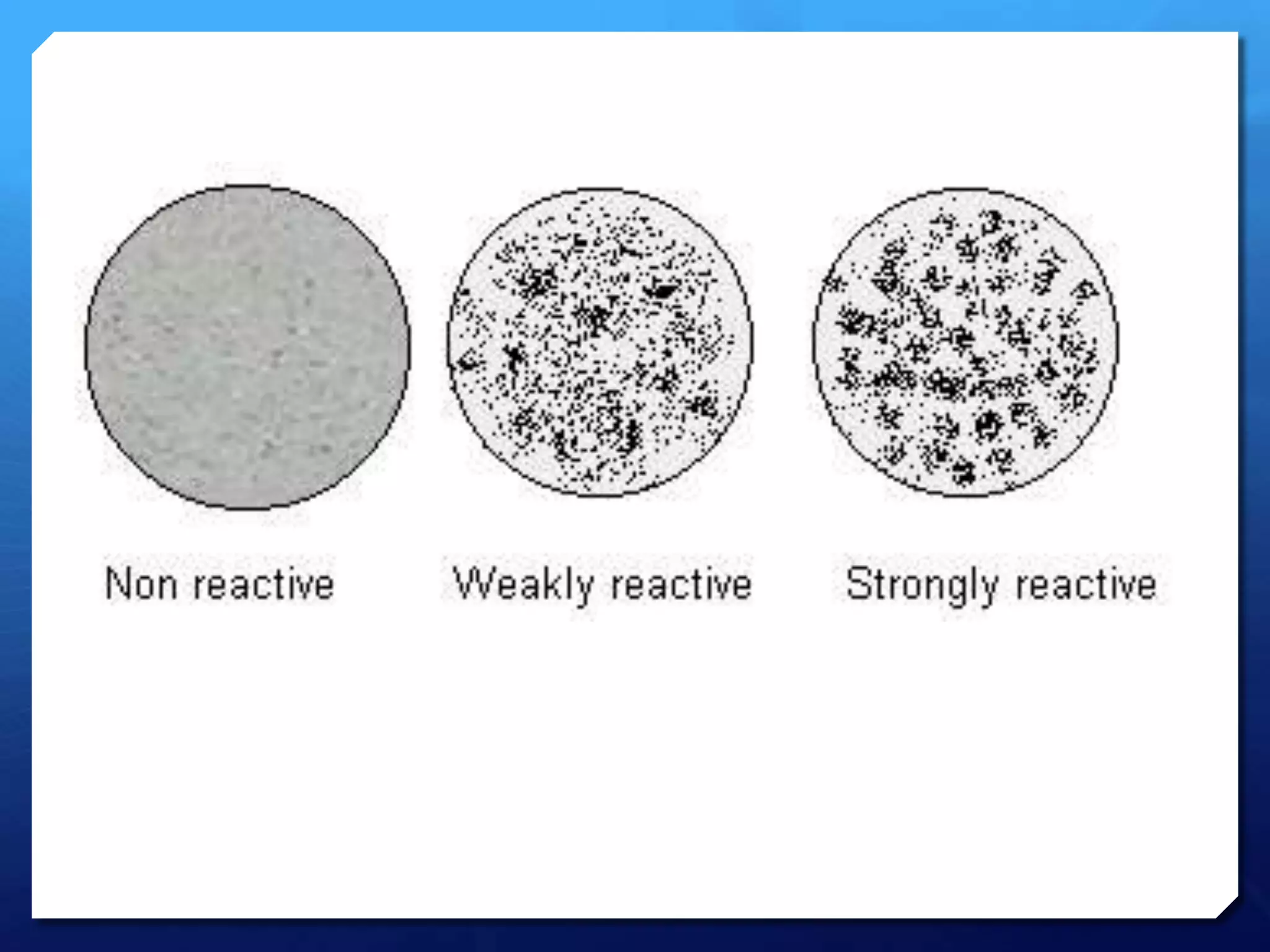
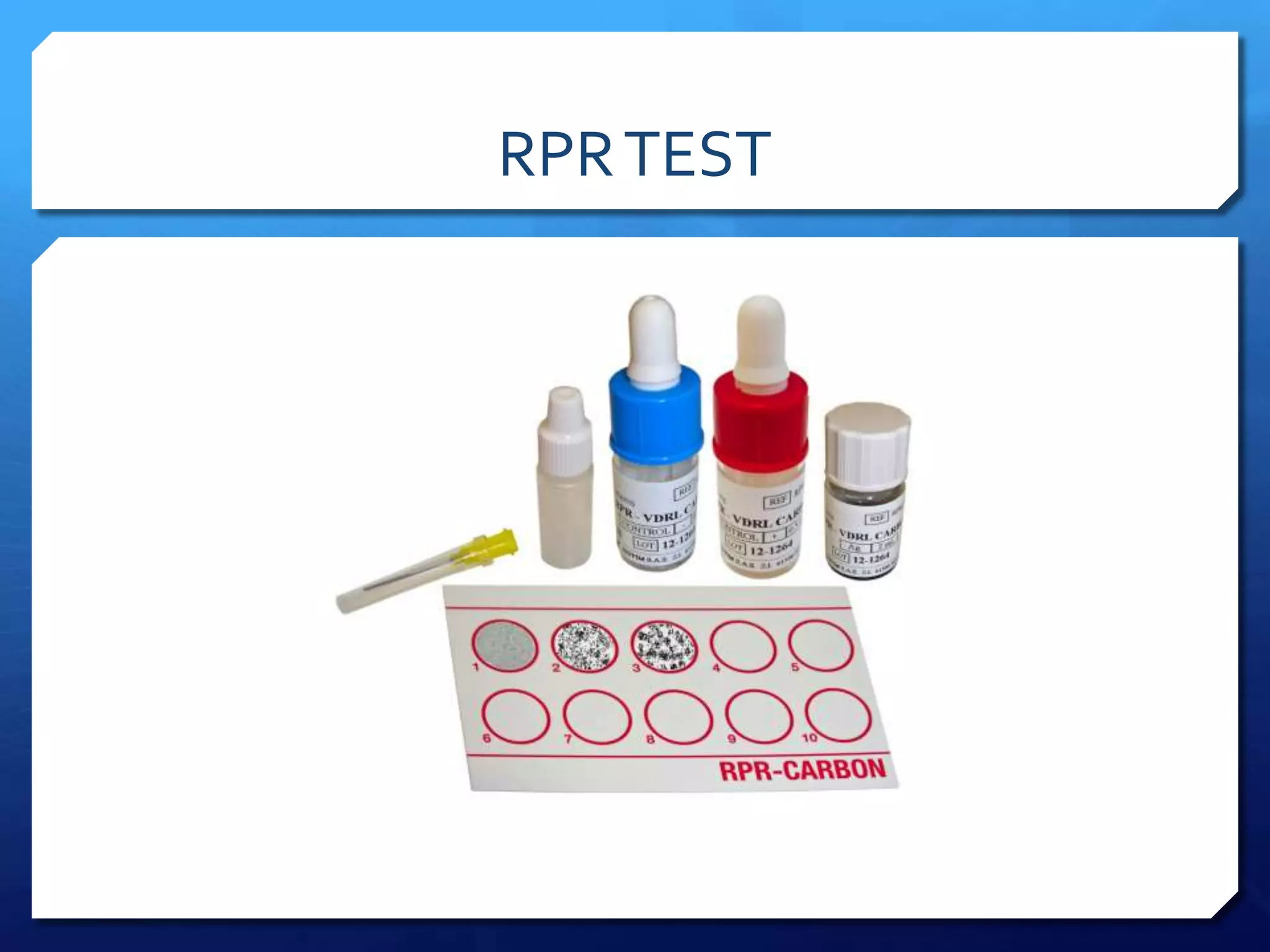
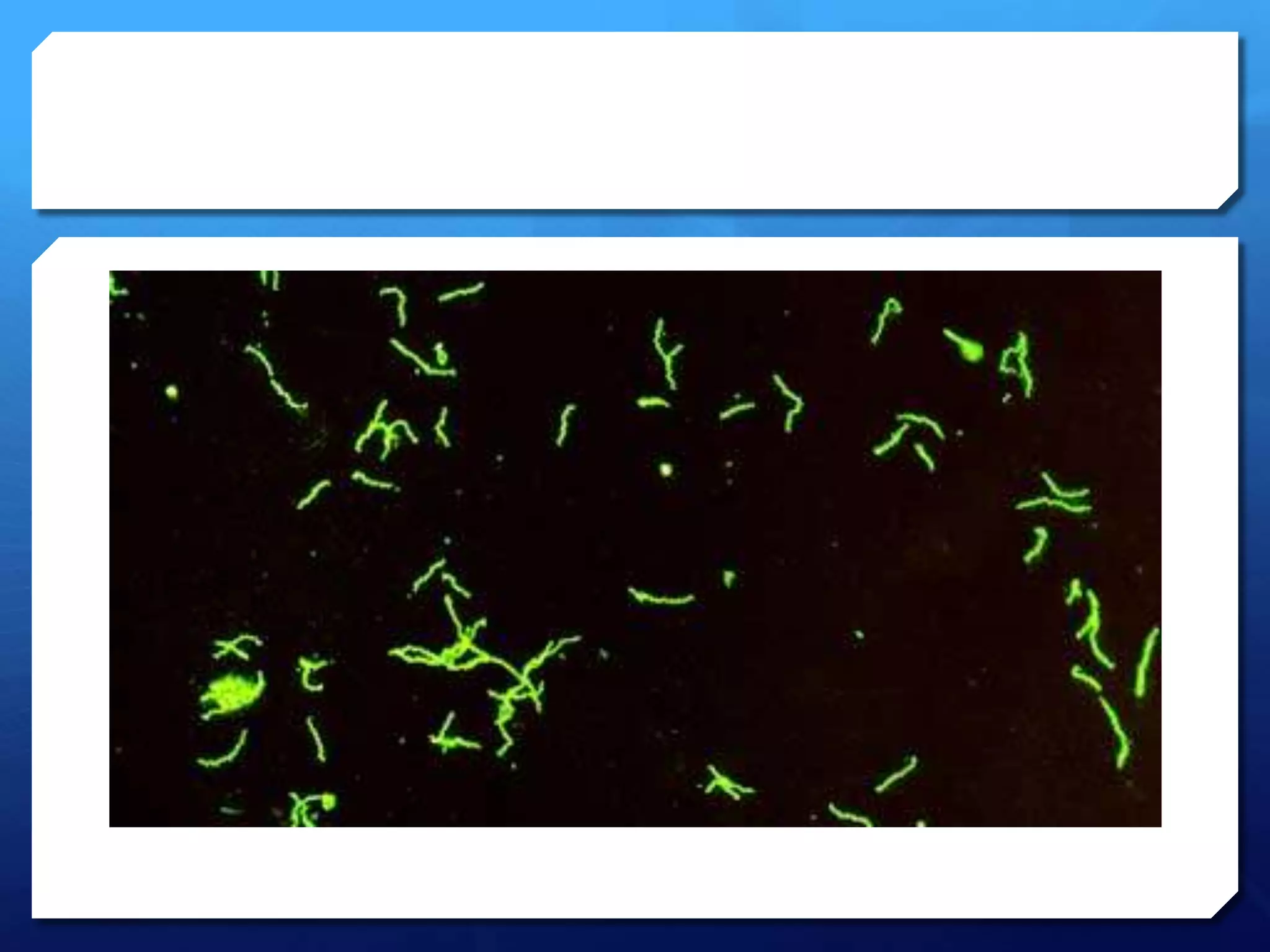
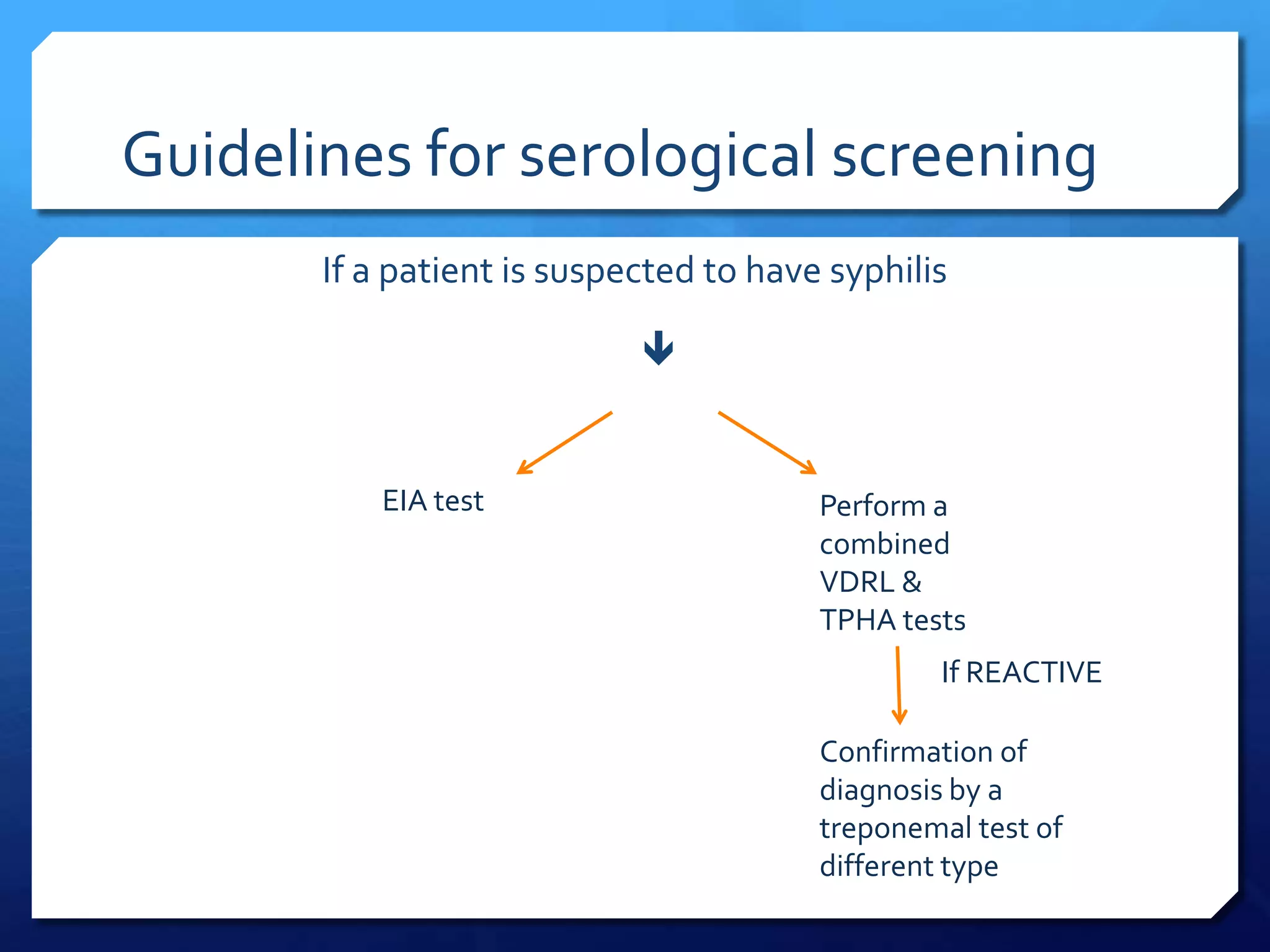
2. Direct tests include dark-field microscopy, direct fluorescent antibody testing, and PCR to identify the bacterium in lesions. Serological tests include non-treponemal tests like VDRL and RPR that detect nonspecific reagin antibodies, and treponemal tests like FTA-ABS, TPHA, and EIA that detect treponema-specific antibodies.
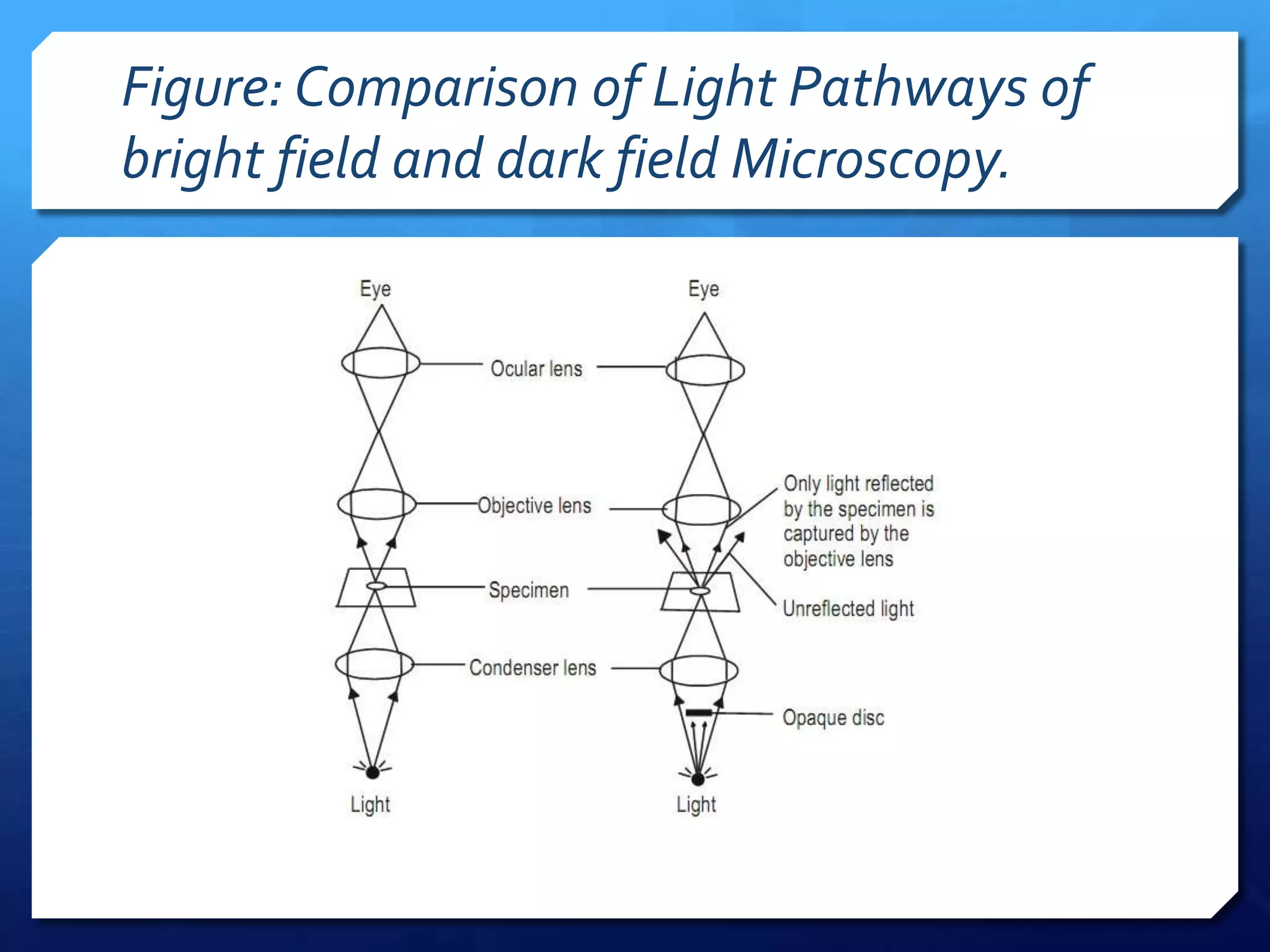
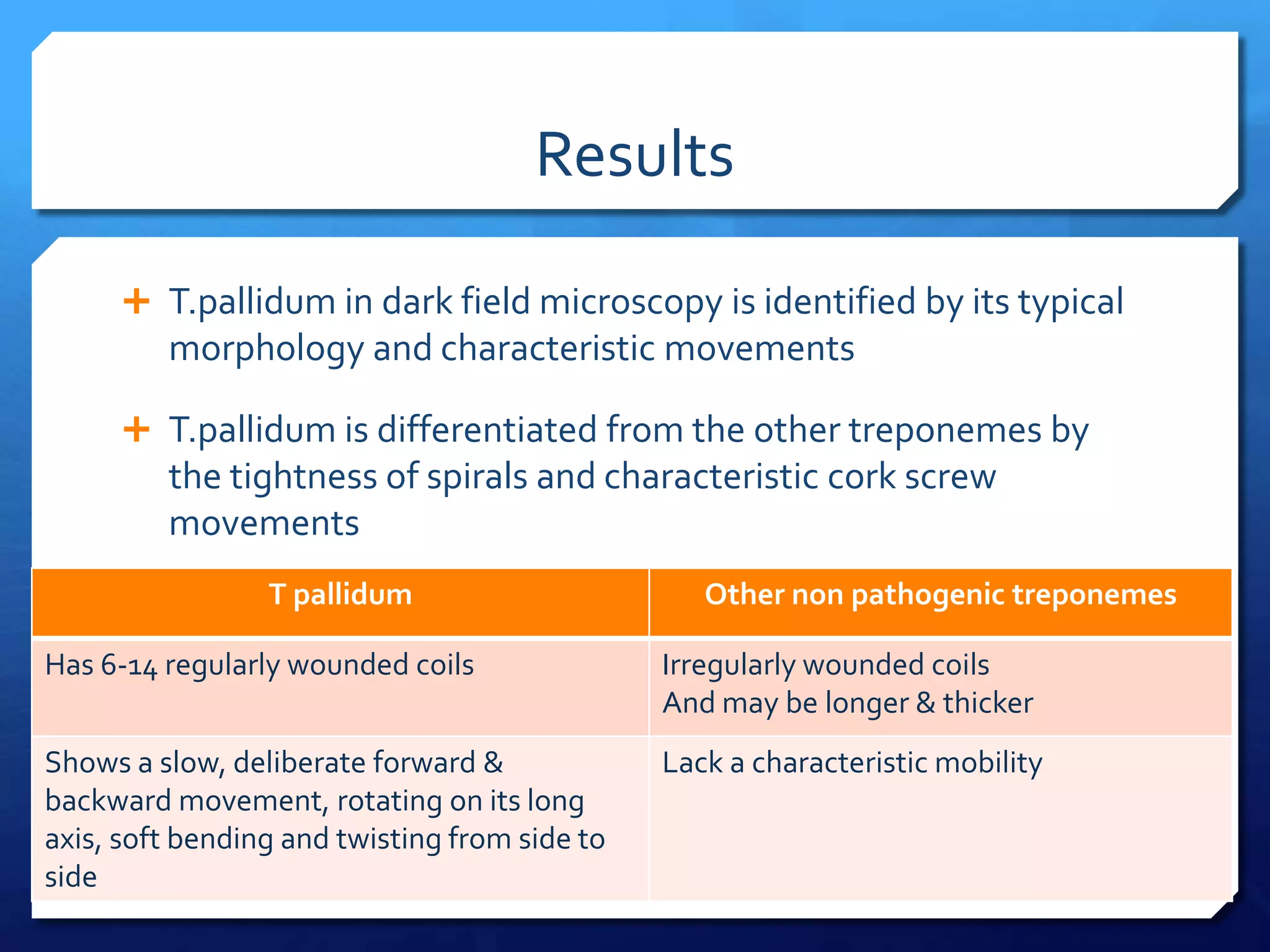
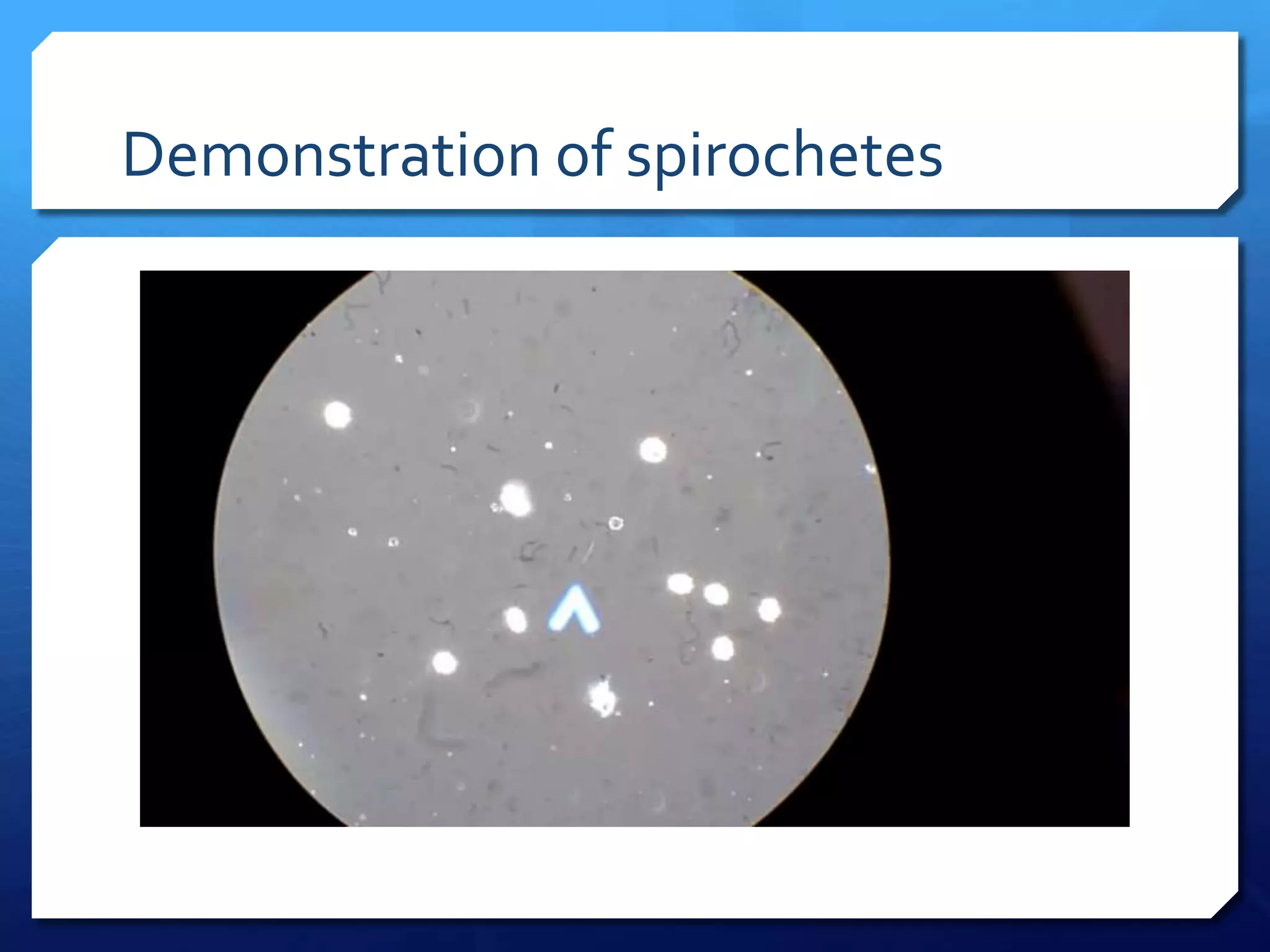
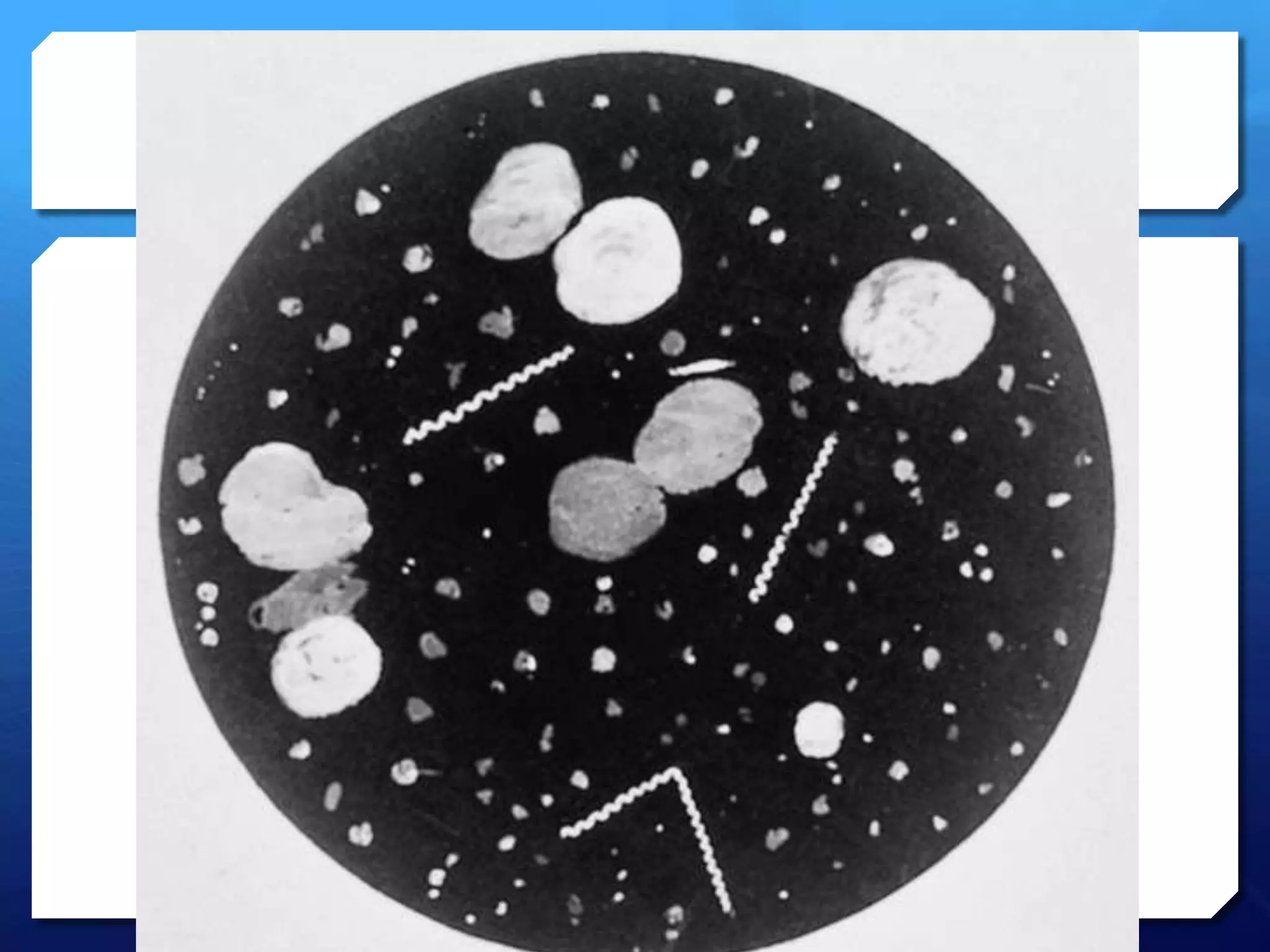
3. Dark-field microscopy examines exudate from lesions under a dark-field microscope to visualize