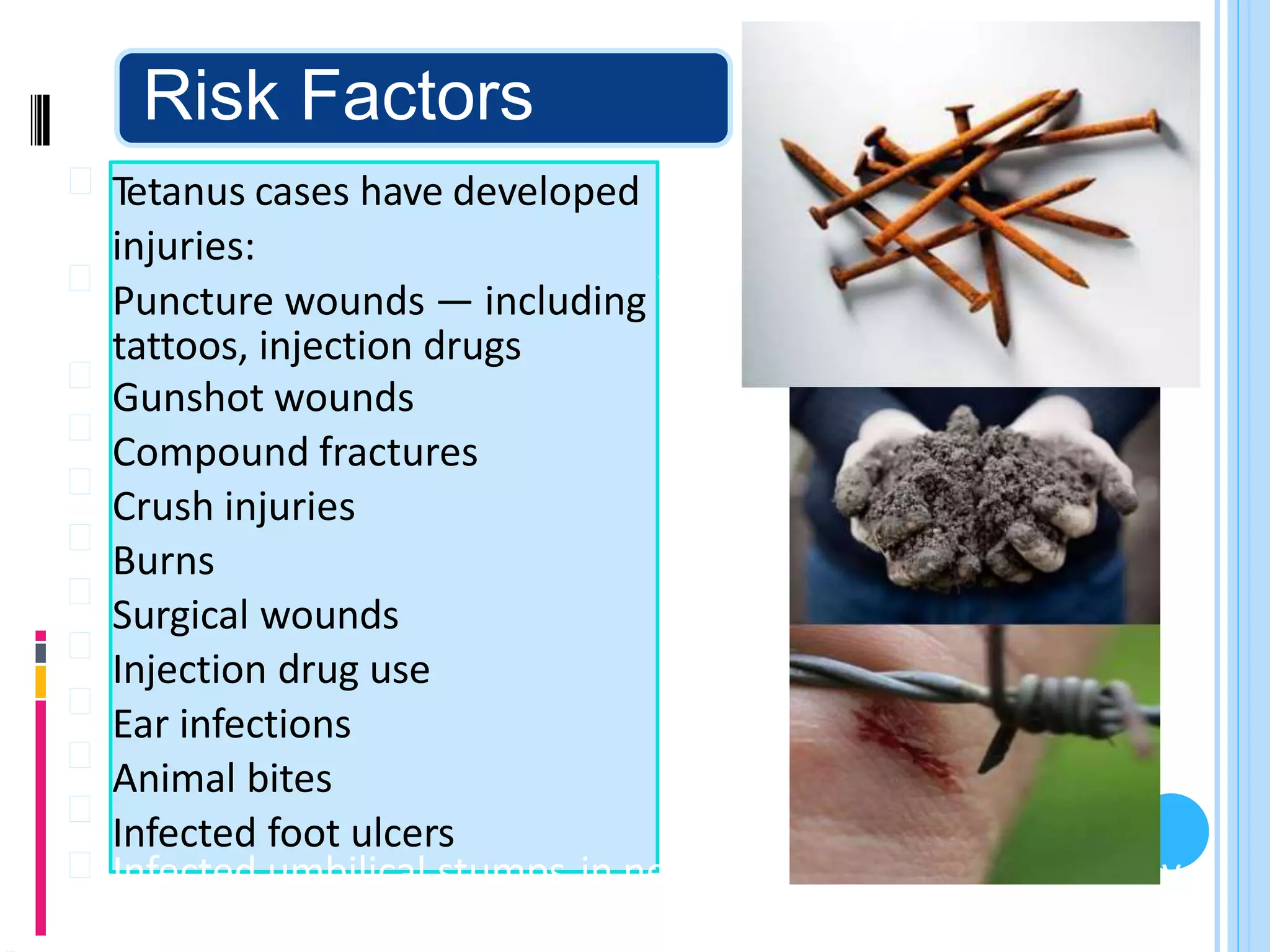
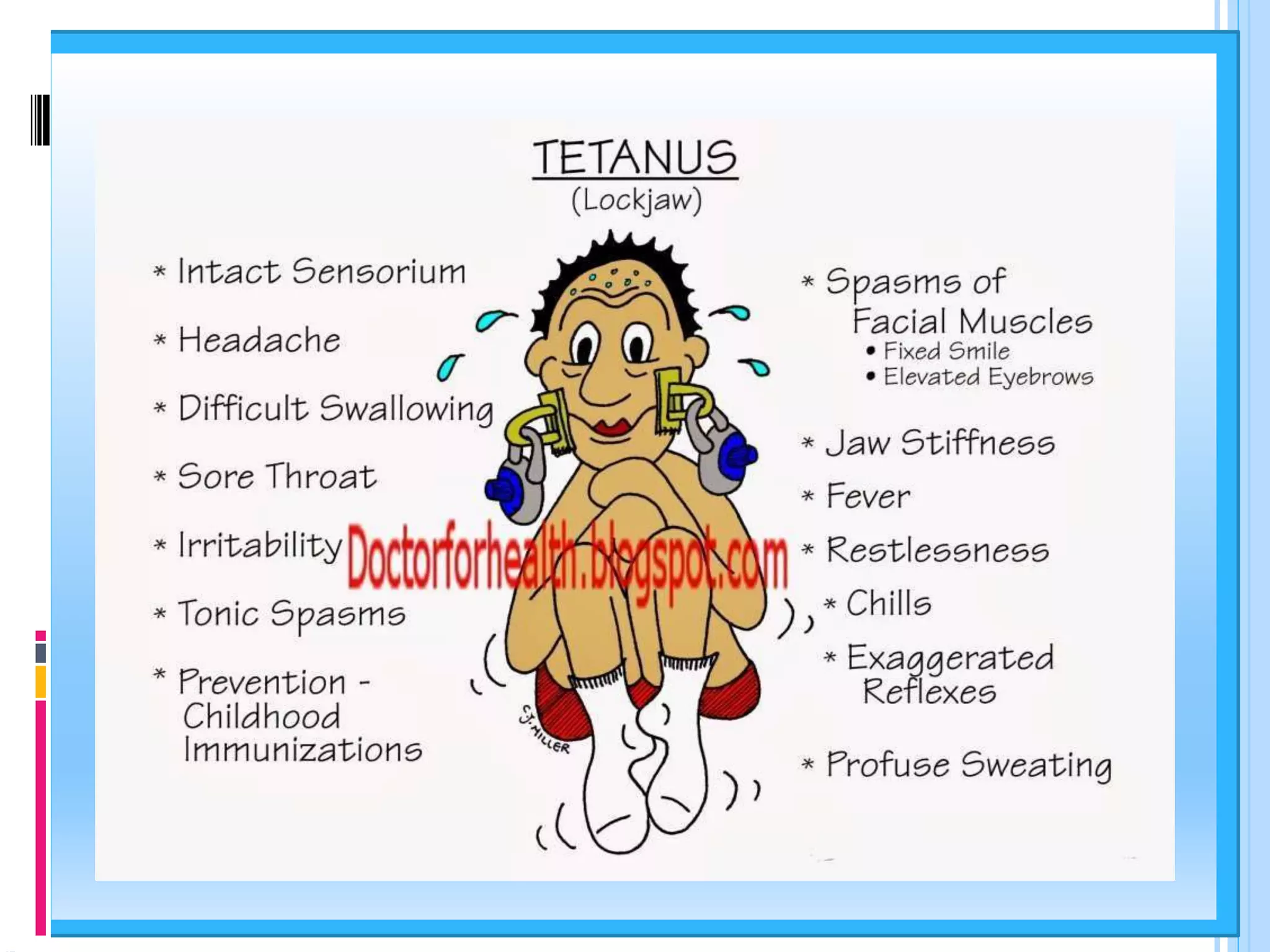
Tetanus is an infectious disease caused by the bacteria Clostridium tetani, primarily acquired through contaminated wounds, leading to muscle stiffness and spasms, commonly known as lockjaw. The disease can progress rapidly, with high mortality rates if untreated, particularly among unvaccinated individuals. Prevention through immunization and prompt treatment of wounds is essential to mitigate the risk of severe complications.