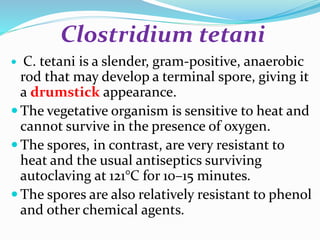
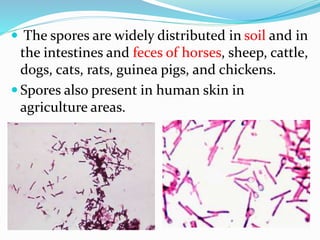
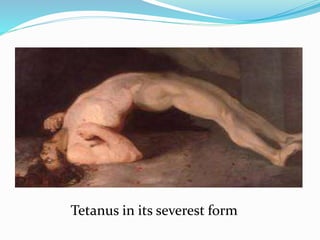
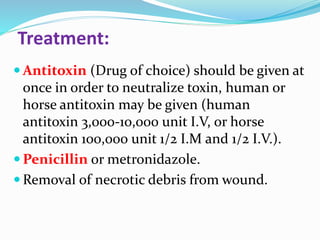
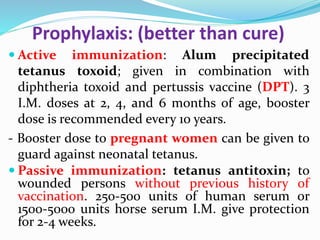
Tetanus is caused by Clostridium tetani bacteria entering the body through a wound. The bacteria produces a neurotoxin called tetanospasmin that causes painful muscle spasms and rigidity. Symptoms typically begin with lockjaw and stiffness of the neck muscles before becoming generalized. The disease is often fatal if untreated. Diagnosis is clinical based on symptoms, though the bacteria can sometimes be identified from wound samples. Treatment involves antitoxin administration to neutralize the toxin along with antibiotics. Prophylaxis through active immunization with tetanus toxoid vaccines or passive immunization with antitoxin is important to prevent occurrence.