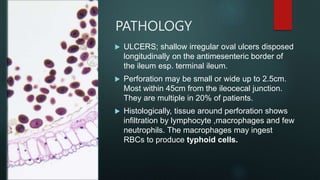
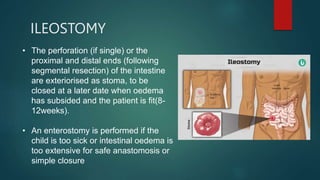
Typhoid intestinal perforation is a serious complication of typhoid fever caused by the bacterium Salmonella typhi. It occurs when the bacteria invade and damage the intestinal wall, usually in the terminal ileum, causing it to perforate. Risk factors include children and young adults in areas with poor sanitation and overcrowding. Symptoms include severe abdominal pain and tenderness. Diagnosis involves blood/stool cultures and imaging. Treatment requires correcting fluid/electrolyte deficits, antibiotics, and surgical closure of perforations with options like simple closure, resection, or temporary ileostomy.