Here are brief summaries of the requested liver conditions:
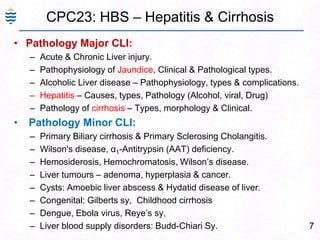
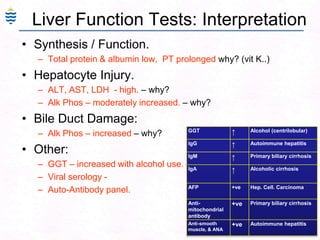
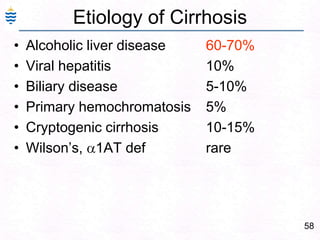
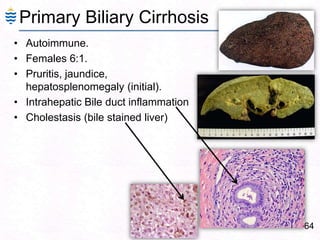
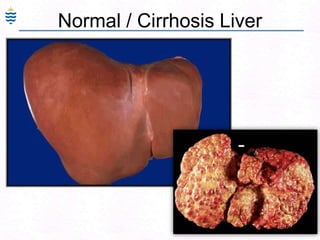
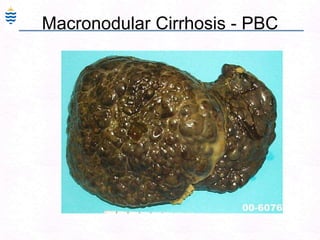
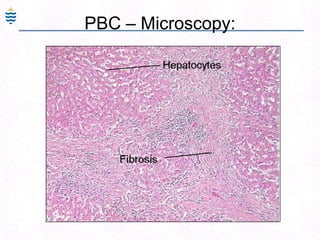
- Primary Biliary Cirrhosis (PBC) and Primary Sclerosing Cholangitis (PSC):
- PBC affects small bile ducts, PSC affects large bile ducts
- PBC more common in females, PSC more common in males
- PBC associated with autoimmune diseases, PSC associated with IBD
- Wilson's disease involves copper accumulation in liver due to ceruloplasmin defect
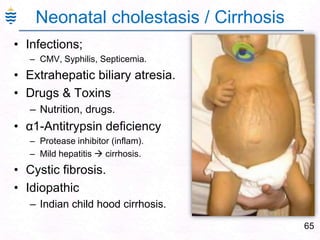
- Alpha-1 antitrypsin deficiency results in decreased protease inhibition and liver damage
- Hemochromatosis involves iron overload due to HFE gene mutation
- Hemosiderosis is iron overload from other causes like