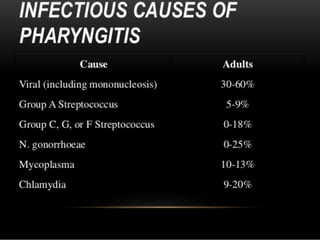
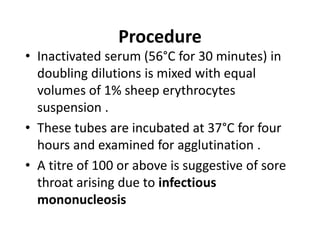
This document discusses the diagnosis of sore throat. It can be caused by various viruses and bacteria that are transmitted through respiratory droplets. Laboratory diagnosis involves collecting a throat swab and examining it under a microscope for pathogens like streptococcus pyogenes or doing cultures on selective media to identify organisms. Tests like bacitracin sensitivity and toxigenic tests help to further identify strep pyogenes and corynebacterium diphtheriae. The Paul Bunnell test detects heterophile antibodies to diagnose sore throat caused by Epstein Barr virus.