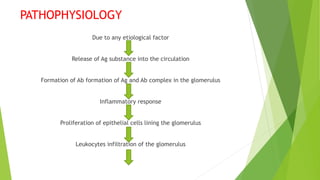
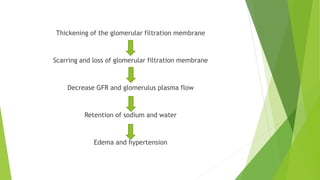
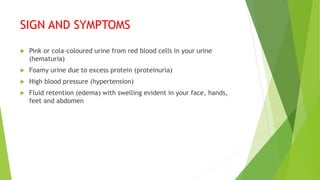
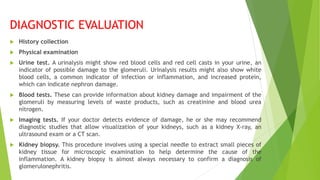
Glomerulonephritis is an inflammation of the kidney's filters, the glomeruli, which can be acute or chronic and result from various causes including infections and autoimmune diseases. Symptoms include hematuria, proteinuria, hypertension, and edema, and diagnosis involves urine and blood tests, imaging, and sometimes a kidney biopsy. Treatment varies based on the cause and severity, emphasizing blood pressure management, dietary restrictions, and supportive measures, with potential for dialysis in severe cases.