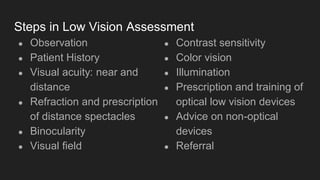
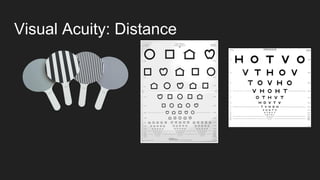
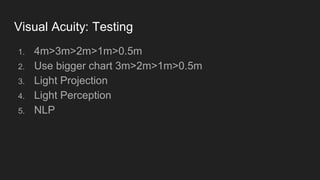
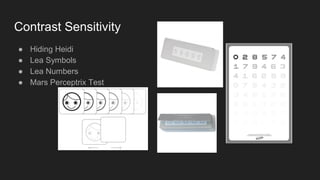
This document provides an overview of low vision assessment techniques. It outlines the underlying philosophy of assessing the psychosocial impact of visual impairment and the stages of grief patients may experience. The document then details the typical steps in a low vision assessment, including observation, patient history, visual acuity testing, refraction, tests of binocularity, visual fields, contrast sensitivity, color vision, and illumination needs. It provides information on techniques for visual acuity testing, refraction, and monitoring follow-up care. The goal of low vision assessment is to understand the patient's needs and vision abilities in order to provide optical and non-optical devices and training to improve their quality of life.