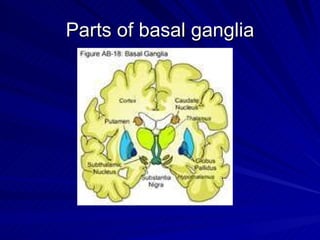
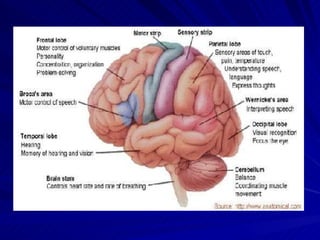
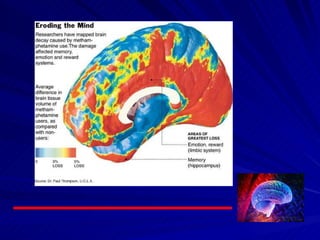
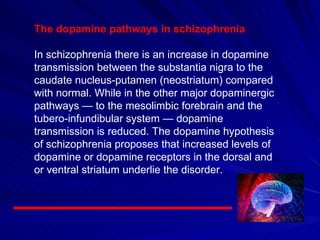
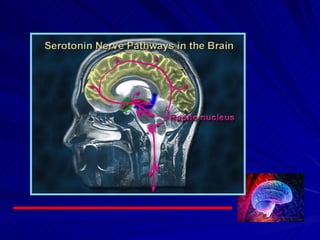
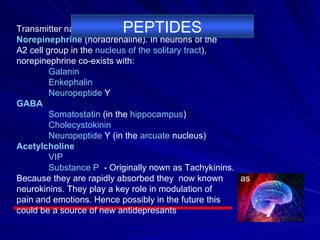
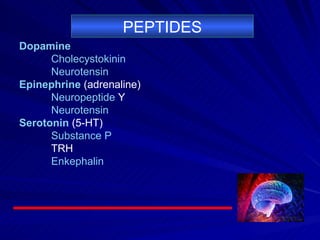
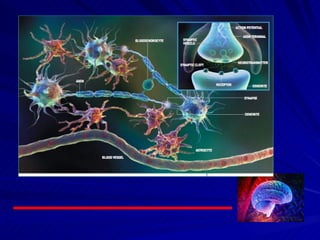
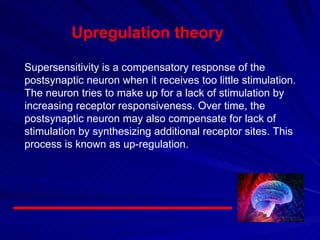
The document discusses the basal ganglia and various brain disorders associated with basal ganglia dysfunction such as Parkinson's disease. It describes the dopamine, glutamate, and serotonergic pathways in the brain and how they are affected in schizophrenia. Various neurotransmitters are also discussed including biogenic amines, amino acids like glutamate and GABA, and peptides. The concept of upregulation of neuronal receptors is introduced as a compensatory response when neurons receive too little stimulation.