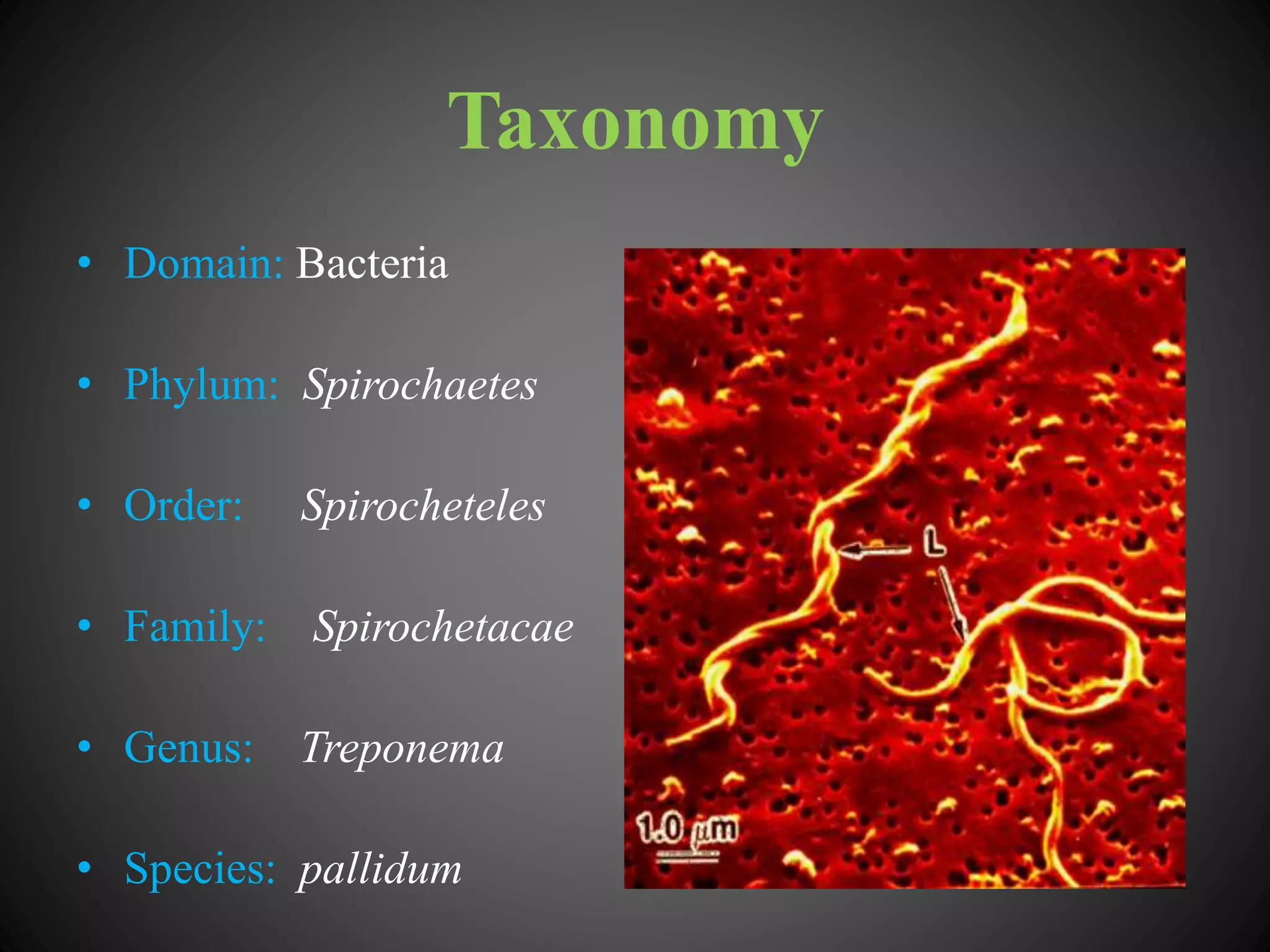
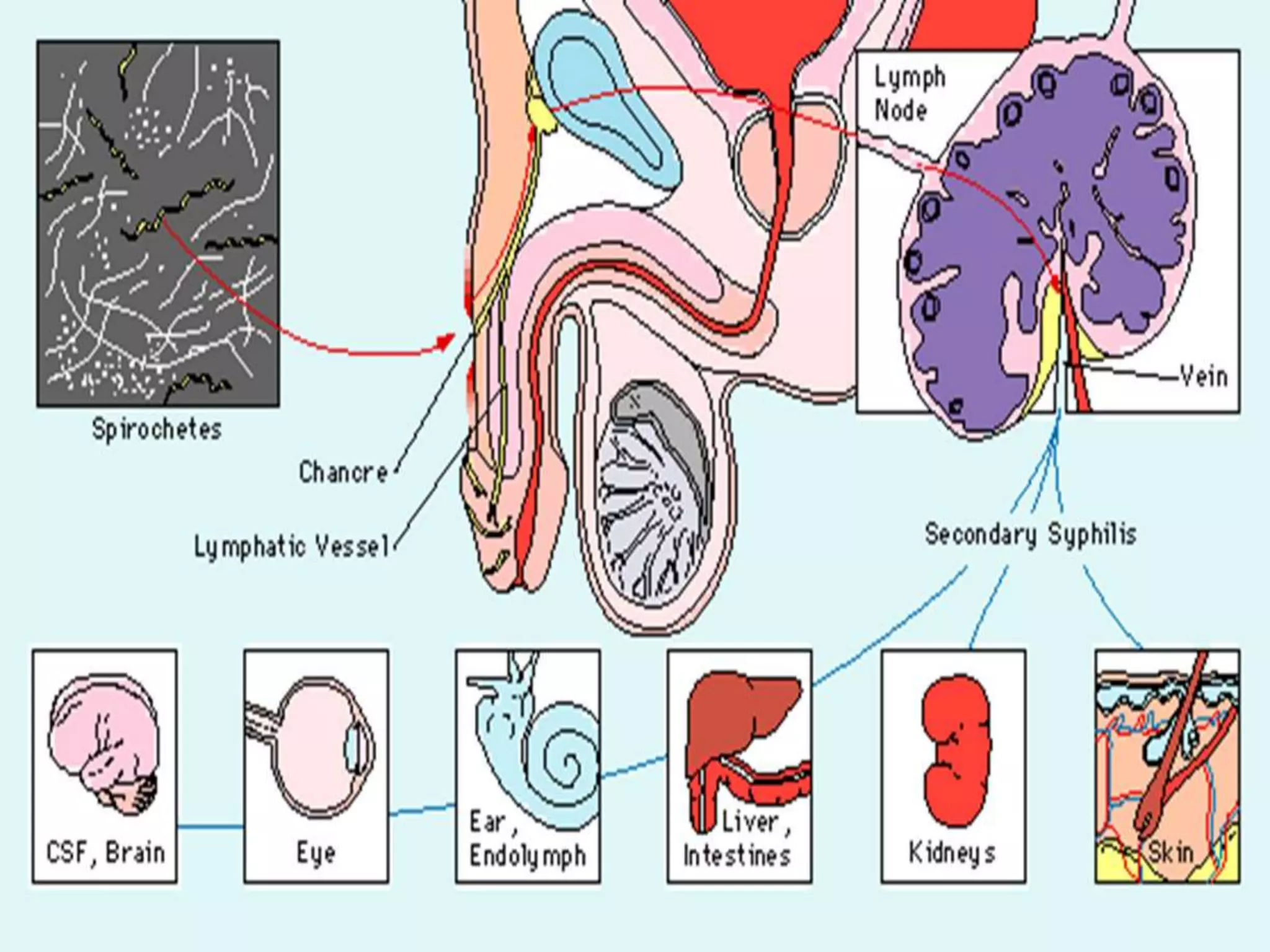
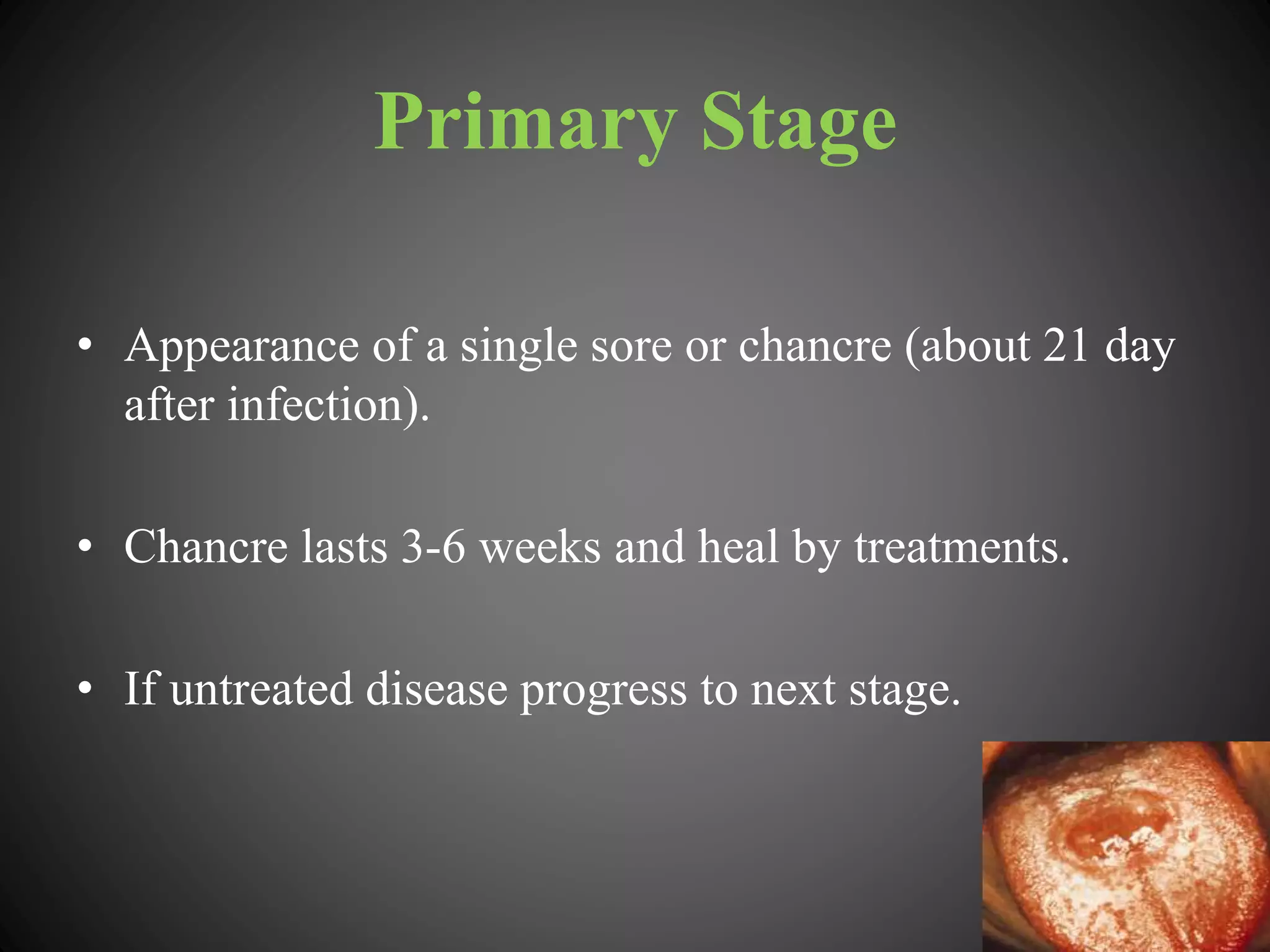
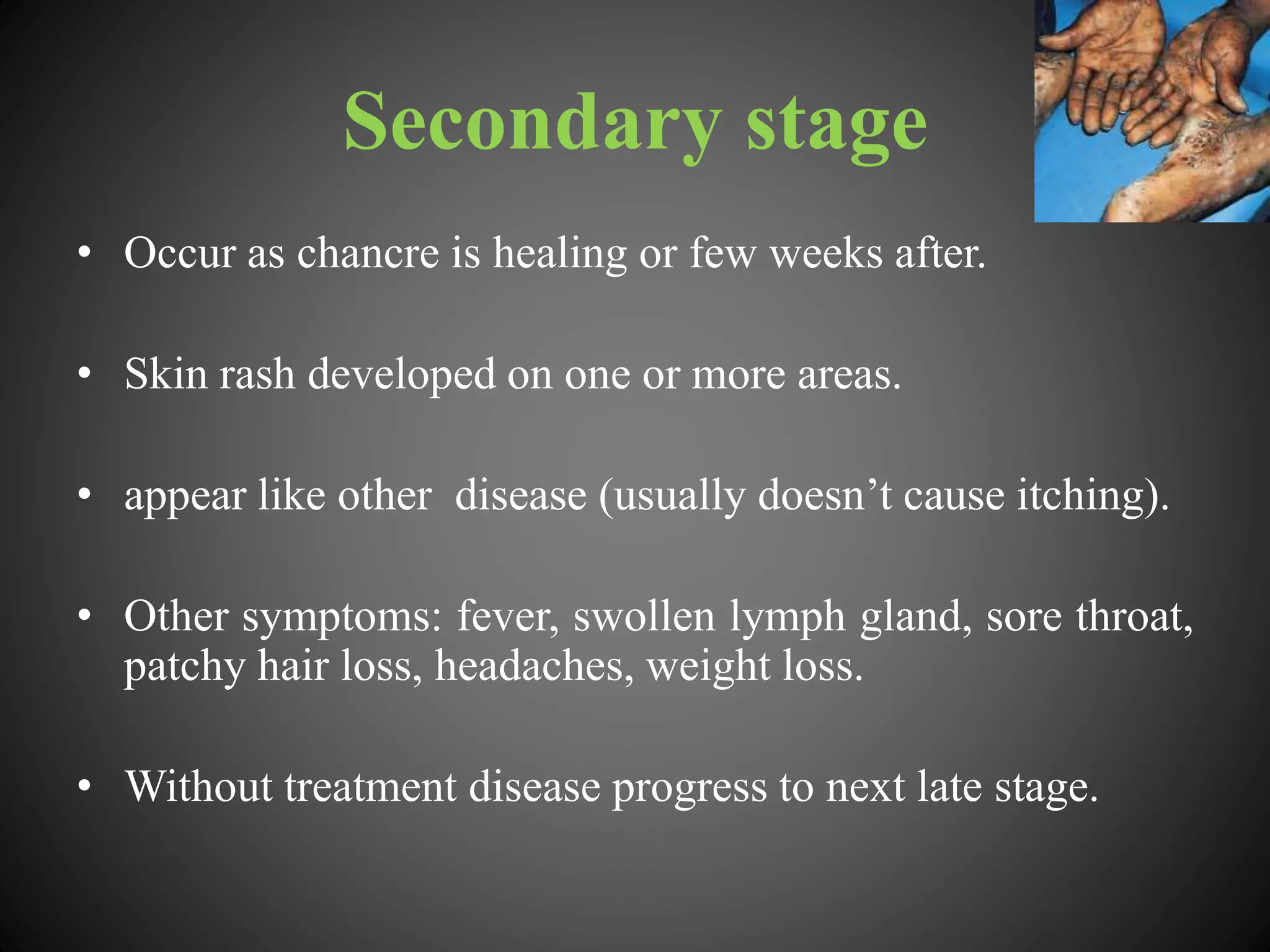
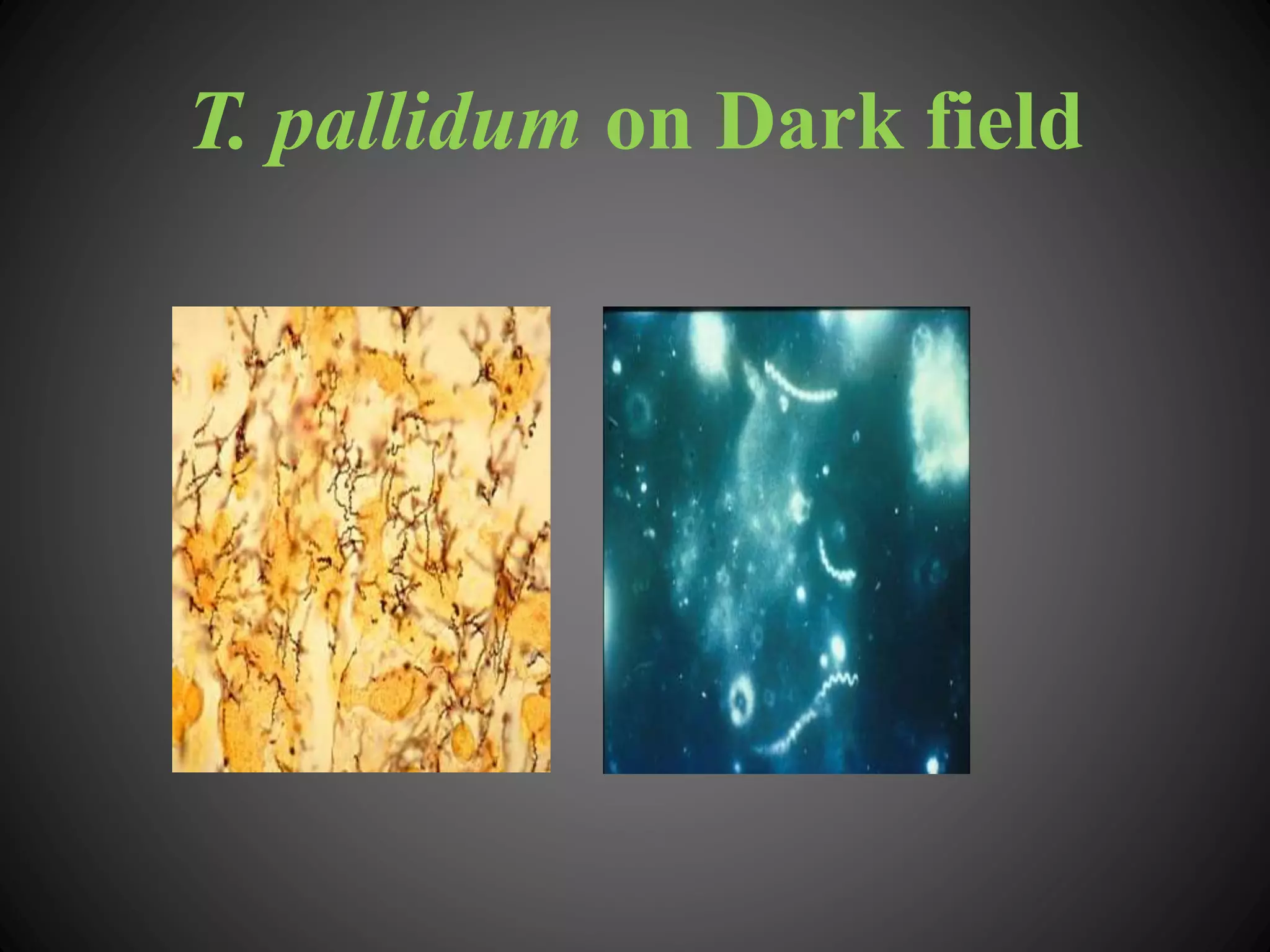
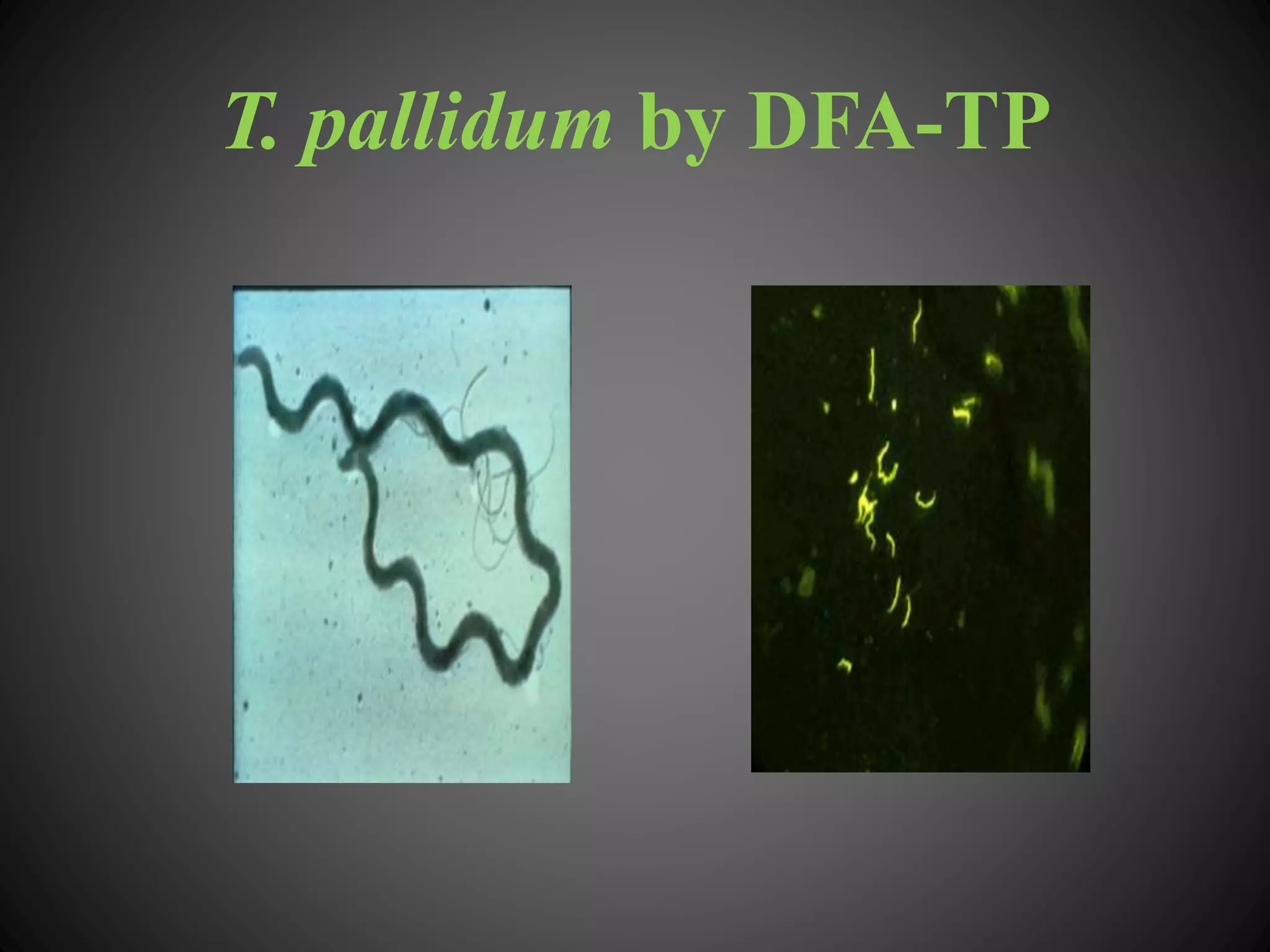
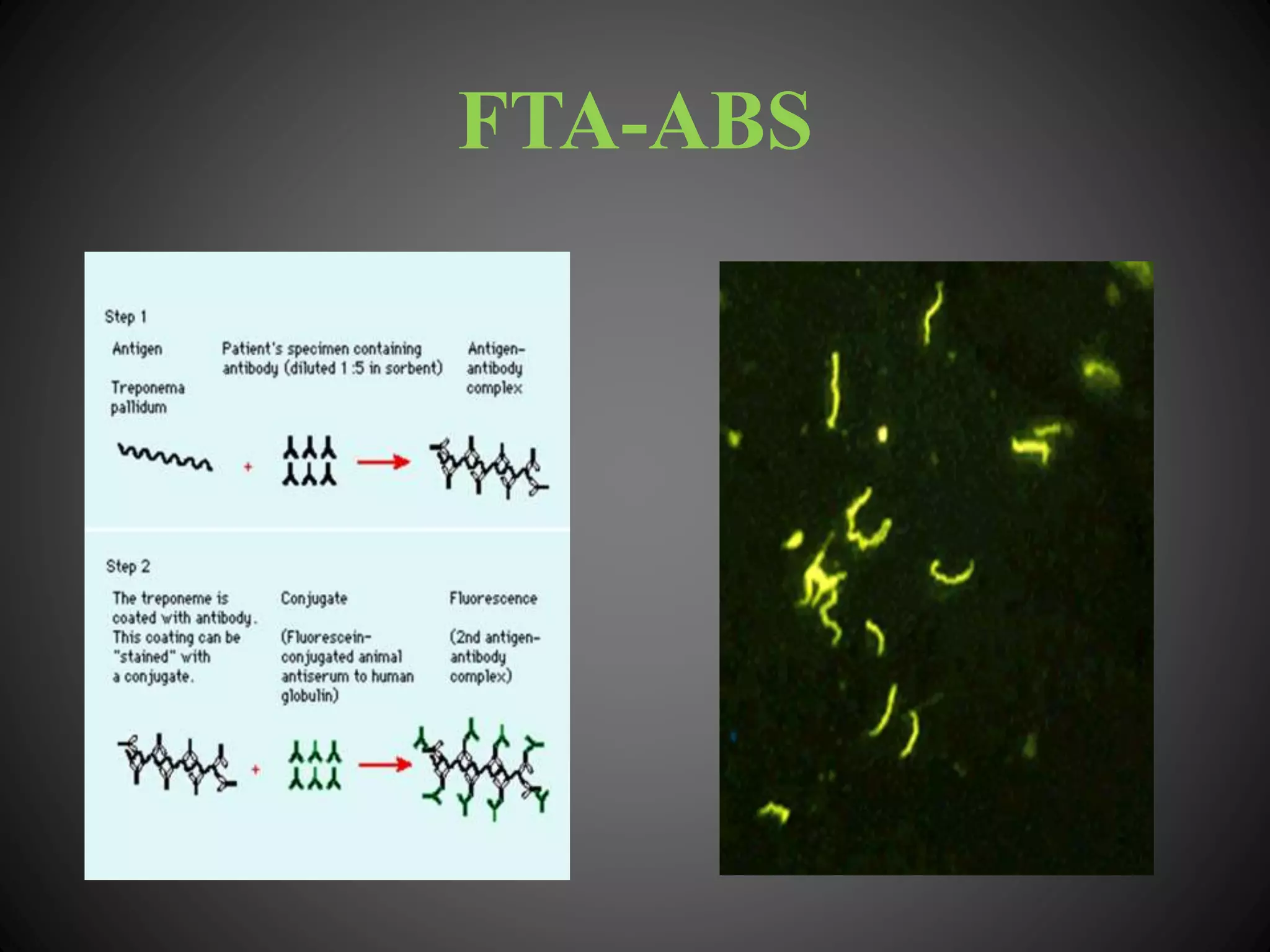
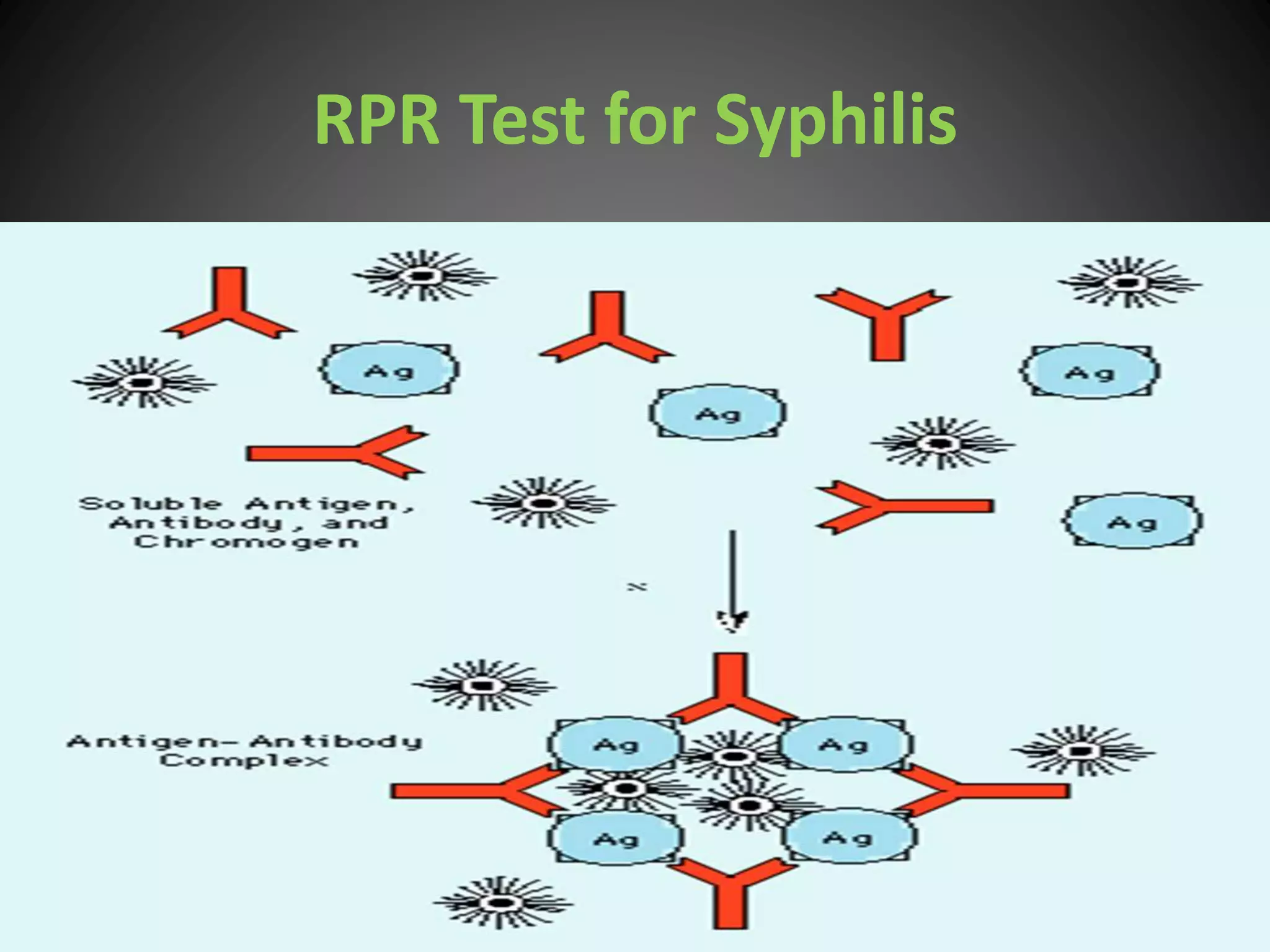
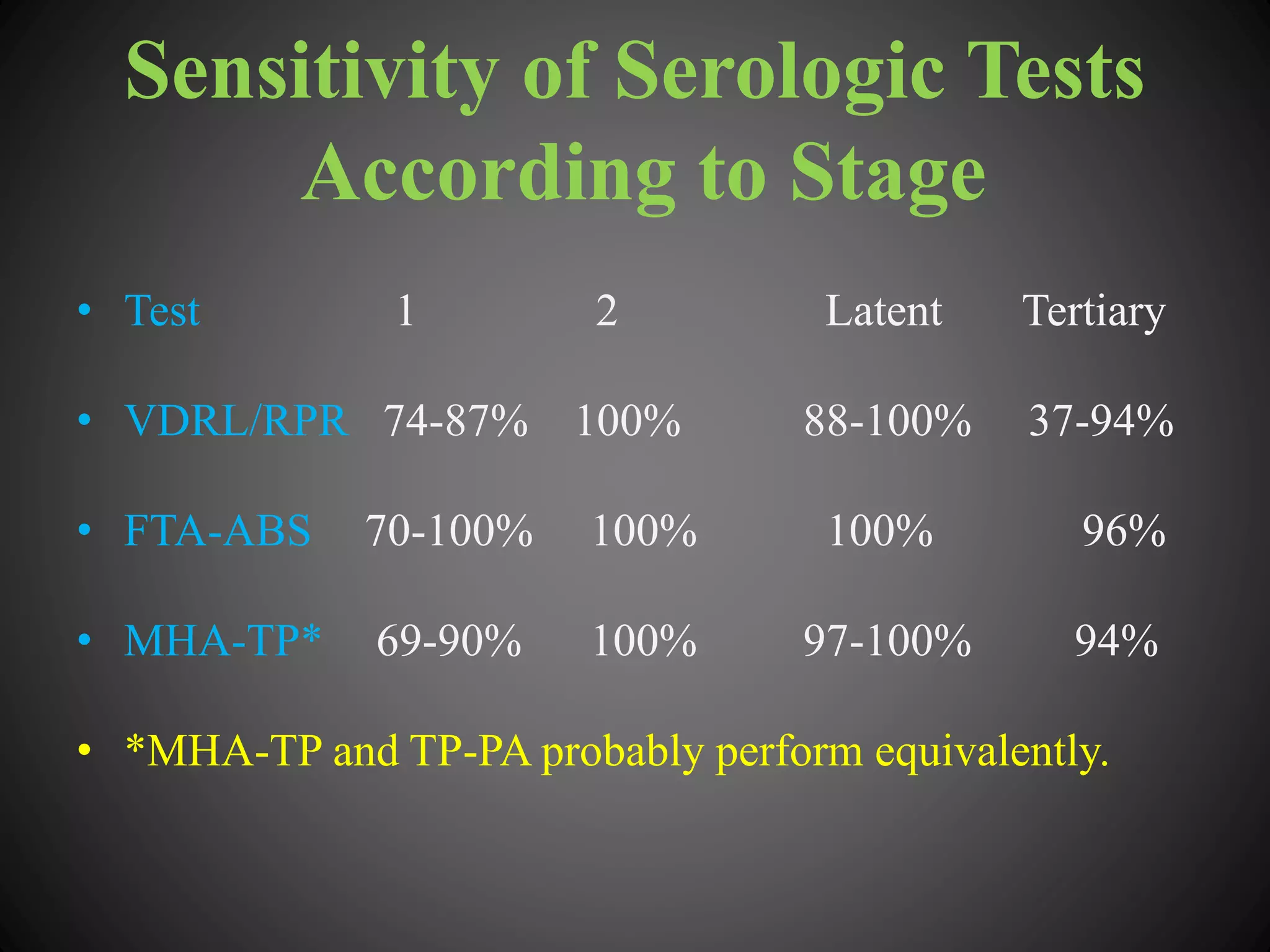
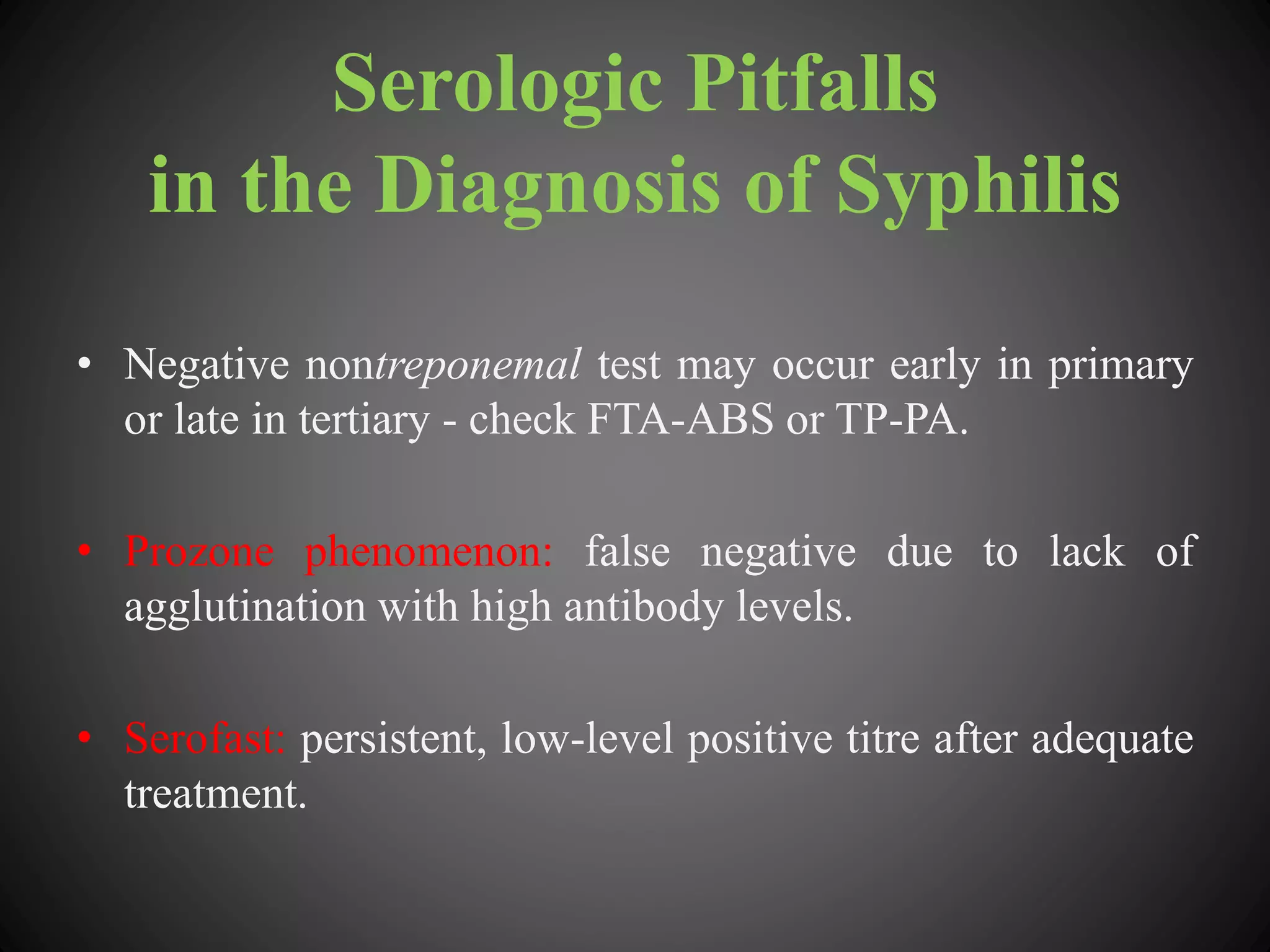
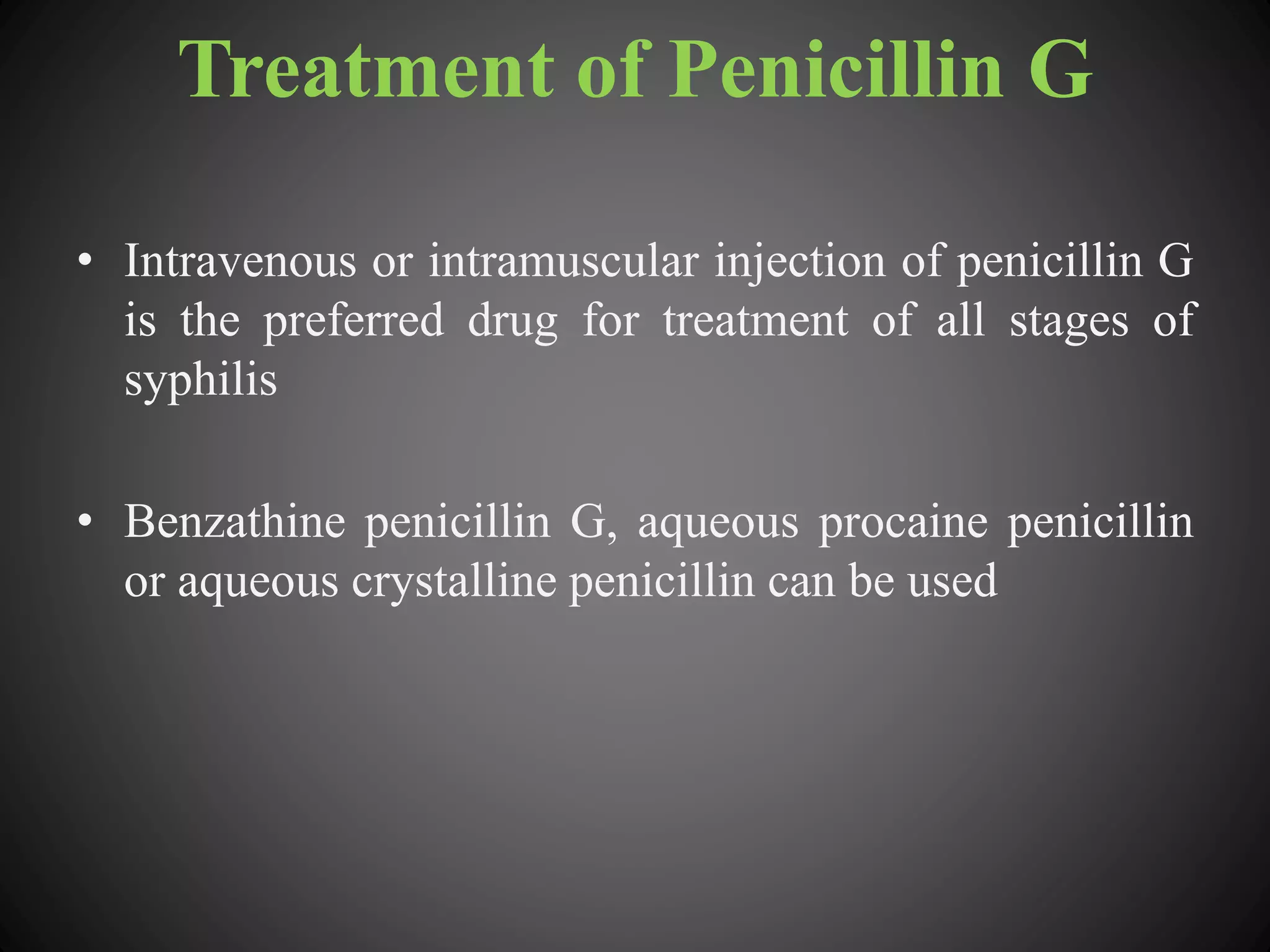
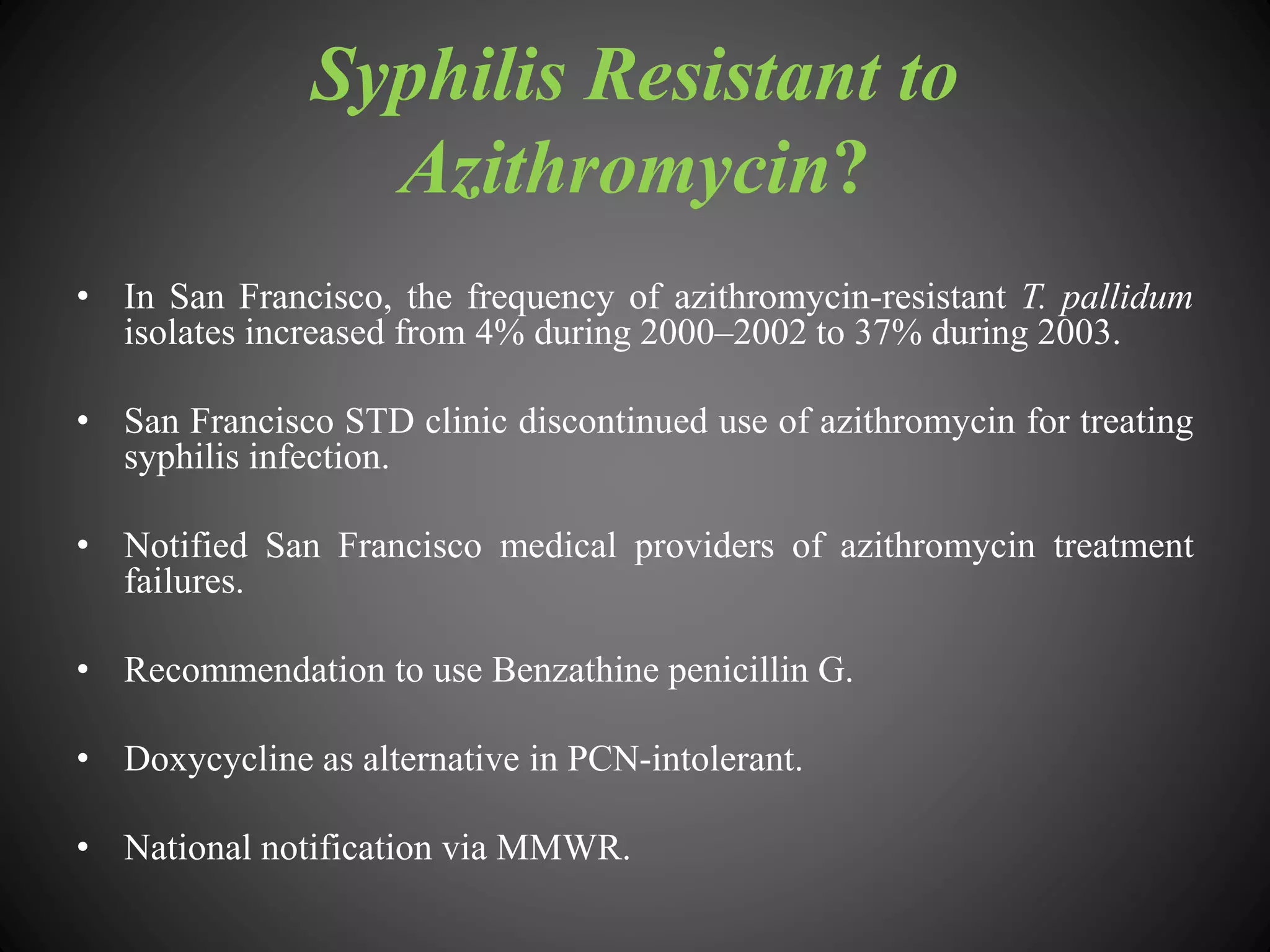
This document provides an overview of syphilis, including its history, transmission, stages, diagnosis, and treatment. It describes how syphilis was an epidemic in 15th century Europe that coincided with Columbus' return from America. The bacterium Treponema pallidum was identified in 1905 as the cause. Syphilis has primary, secondary, and latent stages involving the skin and other organs. Diagnosis involves dark-field microscopy, PCR and serological tests. Penicillin remains the preferred treatment, though some areas have reported resistance to azithromycin. Partner management and consistent condom use can help reduce transmission of the disease.