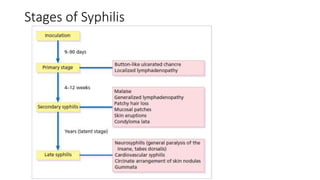
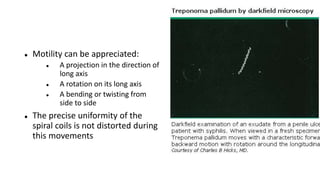
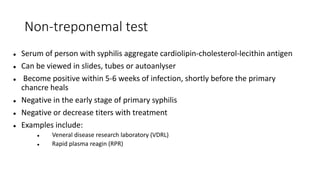
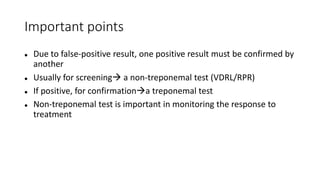
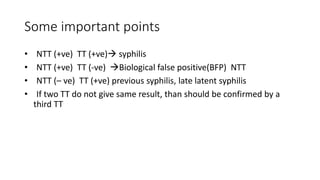
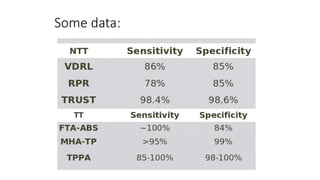
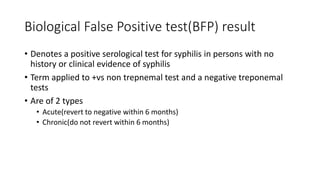
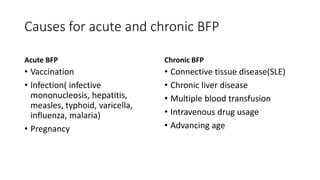
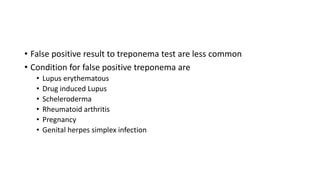
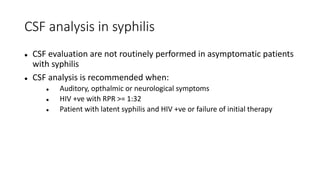
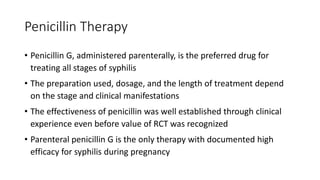
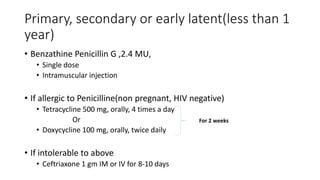
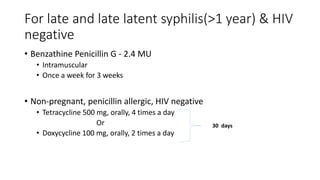
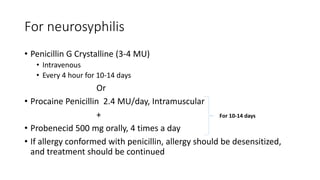
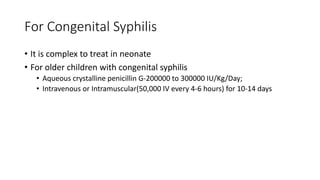
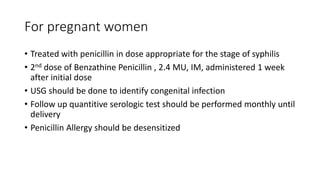
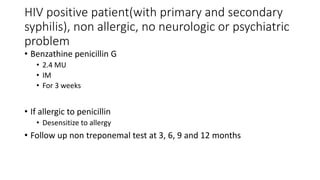
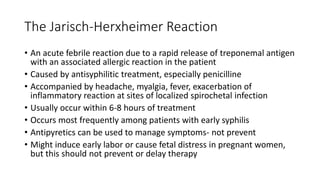
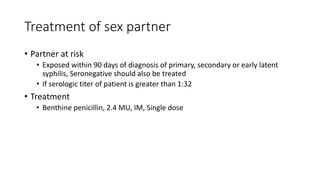
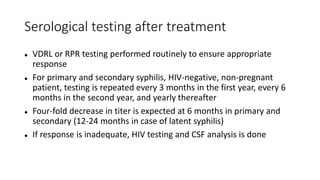
The document provides a comprehensive overview of the management of syphilis, detailing stages, investigation methods, and treatment options. It covers various diagnostic tests, including dark field microscopy, direct fluorescent antibody tests, and serological tests, along with their specificity and indications. Treatment is primarily with penicillin, with specific regimens tailored based on the stage of syphilis and patient factors.