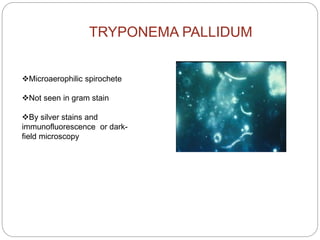
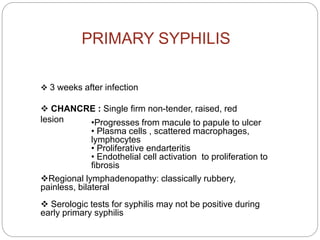
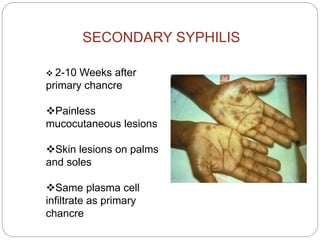
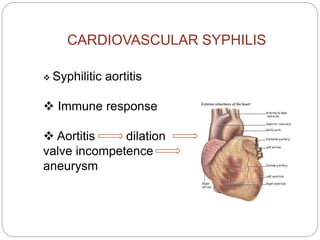
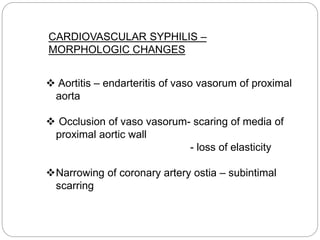
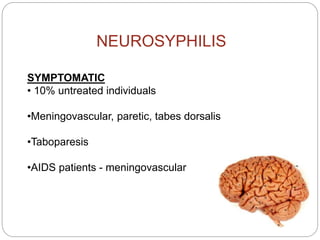
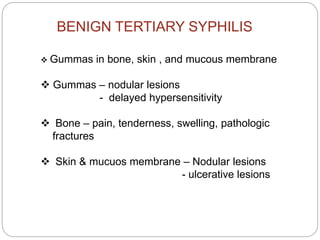
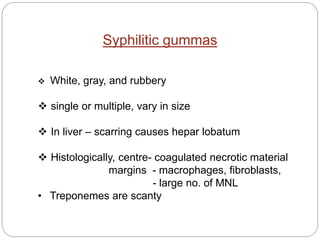
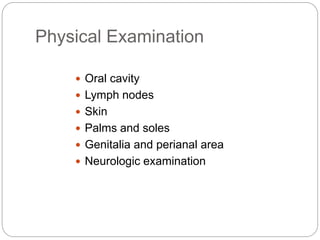
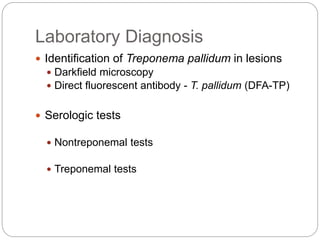
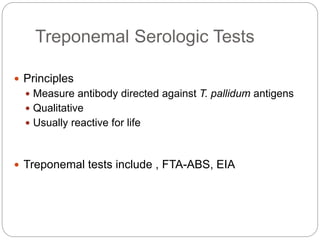
This document summarizes syphilis, caused by the spirochete Treponema pallidum. It is transmitted sexually or vertically. Primary syphilis presents as a chancre, which disseminates and causes secondary syphilis skin lesions. Without treatment, it can progress to latent, tertiary cardiovascular, or neurosyphilis stages involving the brain, heart and blood vessels. Diagnosis involves clinical history, exams, and serological tests detecting nontreponemal and treponemal antibodies. Penicillin is the treatment, while abstinence and safe sex practices prevent transmission.