This document provides information about syphilis, including:
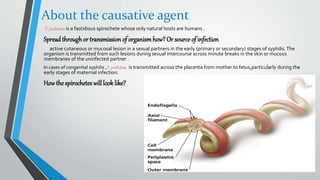
1. Syphilis is a chronic infection caused by the bacterium Treponema pallidum that is transmitted sexually or congenitally.
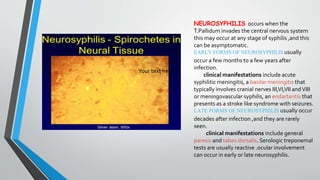
2. Primary syphilis presents as a chancre on the genitals or mouth. Secondary syphilis causes a rash and mucous membrane lesions. Tertiary syphilis can damage internal organs if left untreated.
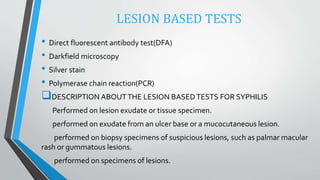
3. Diagnosis involves darkfield microscopy of lesions, serological tests like RPR and FTA-Abs, and PCR. Treatment is with penicillin. Counseling involves educating patients about transmission risks and screening of partners.