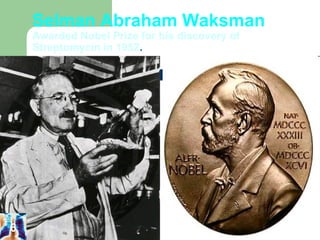
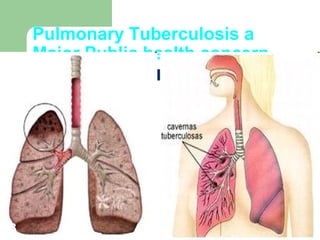
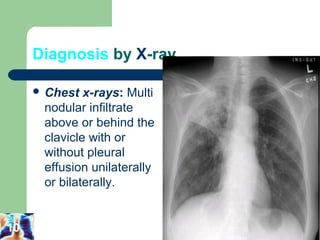
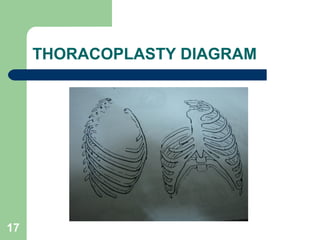
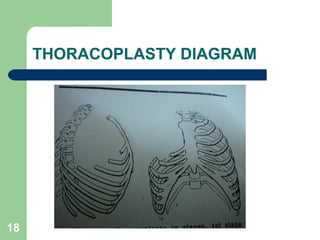
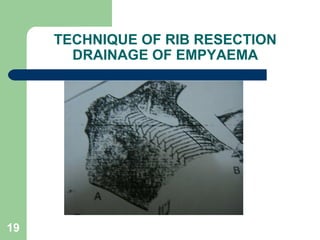
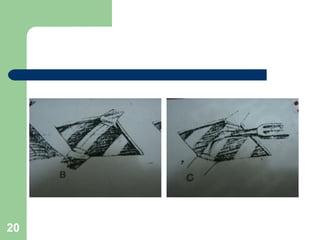
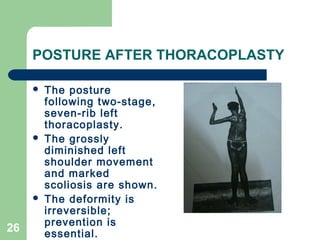
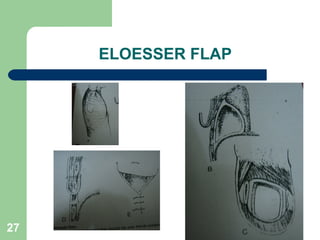
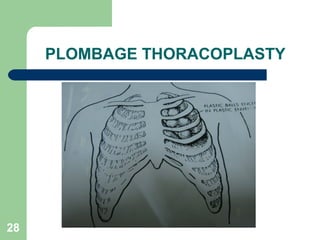
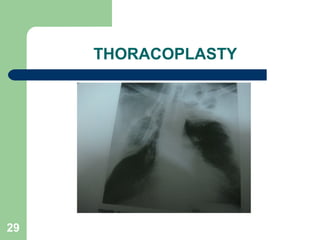
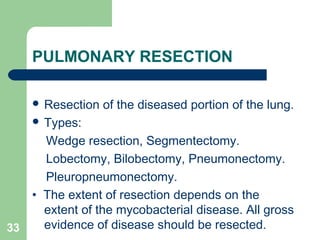
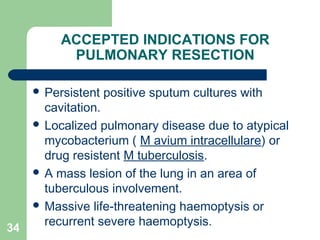
The document discusses the historical context, diagnosis, and surgical treatment of pulmonary tuberculosis, emphasizing the contributions of notable figures like Robert Koch. It details the roles of various diagnostic techniques, types of drug resistance, and outlines specific surgical interventions, including their indications, benefits, and potential complications. Despite advances in chemotherapy, surgery remains necessary for a small percentage of cases, highlighting the importance of careful patient selection and management.